Asthma
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 20 Nov 2023
Meets Patient’s editorial guidelines
In this series:Asthma inhalersPeak flow meter for asthma
Asthma is a common condition that affects the airways. The typical symptoms are wheeze, cough, chest tightness, and shortness of breath. Symptoms can range from mild to severe. Treatment usually works well to ease and prevent symptoms.
Treatment is usually with inhalers. A typical person with asthma may take a preventer inhaler every day (to prevent symptoms developing) and use a reliever inhaler as and when needed (if symptoms flare up). This leaflet gives a general overview of asthma. There are other separate leaflets in this series.
In this article:
Continue reading below
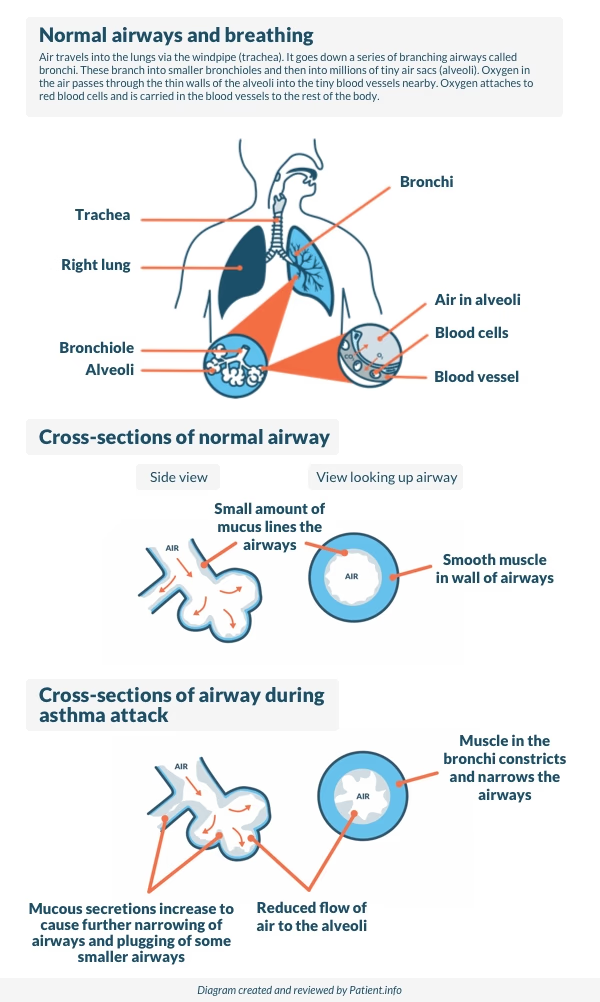
What is asthma?
Asthma is a condition that affects the smaller airways (bronchioles) of the lungs. From time to time the airways narrow (constrict) in people who have asthma.
This causes the typical symptoms of asthma (see below). The extent of the narrowing, and how long each episode lasts, can vary greatly.
About 8 million people in the UK have asthma, which is about 12 in every 100 people. Asthma can start at any age but it most often starts in childhood.
Asthma runs in some families but many people with asthma have no other family members affected.
Patient picks for Asthma
Asthma symptoms
Common asthma symptoms are:
Coughing.
Breathlessness.
Feeling of chest tightness.
Asthma symptoms can range from mild to severe between different people and at different times in the same person. Each episode of asthma symptoms could last for an hour or so, or persist for days or weeks unless treated.
Symptoms of mild untreated asthma
Mild asthma symptoms can occur from time to time. For example, a mild wheeze and a cough with a cold or a chest infection. Mild symptoms may also occur during the hay fever season, or with exercise.
Most of the time there may be no asthma symptoms at all. A child with mild asthma may have an irritating cough each night but is often fine during the day.
Symptoms of moderate untreated asthma
Typically there are episodes of wheezing and coughing from time to time. Sometimes breathless may occur. There is usually spells without symptoms. However, wheezing tends to occur for some of the time on most days.
Symptoms are often worse at night, or first thing in the morning. Symptoms may include waking some nights coughing or with a tight chest.
Young children may not have typical symptoms. It may be difficult to tell the difference between asthma and recurring chest infections in young children.
Symptoms of a severe asthma attack
A severe asthma attack causes severe wheezing, a tight chest and difficulty in breathing. It may be difficult to talk because of being severely breathless.
With severe breathlessness, there may be no wheeze because of insufficient air going to and from the lungs. This is called a silent chest and needs immediate medical attention.
Severe symptoms may develop suddenly in some people who usually just have mild or moderate symptoms.
Continue reading below
When to see a doctor about asthma
It is very important to see a doctor if there is any concern that an adult or child has asthma. Several conditions can cause similar symptoms, so it's important to get a proper diagnosis and correct treatment. The doctor will usually be able to diagnose asthma by asking about symptoms and carrying out some simple tests.
If asthma has already been diagnosed, a doctor or nurse should be seen if the symptoms become worse and cannot be controlled by the usual treatments.
A severe asthma attack, especially with difficulty breathing that does not respond to usual asthma treatment, is a medical emergency. Call an ambulance immediately.
What causes asthma?
The symptoms of asthma are caused by inflammation in the airways, which may be triggered by different things in different people. The inflammation causes the muscles around the airways to squeeze (contract).
This causes narrowing of the airways. It is then more difficult for air to get in and out of the lungs. This leads to wheezing and breathlessness. The inflammation also causes the lining of the airways to make extra mucus which causes cough and further blockage to the airflow.
The following diagram below shows how an episode of asthma develops.
How asthma develops
Asthma symptoms may flare up from time to time. There is often no obvious reason why asthma symptoms flare up.
Asthma triggers
However, some people find that symptoms are triggered, or made worse, in certain situations. It may be possible to avoid certain triggers, which may help to reduce symptoms. Things that may trigger asthma symptoms include the following:
Infections - particularly colds, coughs and chest infections.
Pollens and moulds - asthma is often worse in the hay fever season.
Exercise - getting asthma symptoms with exercise often means asthma is undertreated. If it happens, it may be necessary to step up usual preventer treatment (see below). Use an inhaler before exercise to prevent symptoms from developing.
Certain medicines - for example, about 1 in 50 people with asthma are allergic to aspirin, which can trigger symptoms. Other medicines that may cause asthma symptoms include:
Anti-inflammatory painkillers such as ibuprofen (for example, Nurofen®), diclofenac, etc.
Beta-blockers such as propranolol, atenolol, or timolol. This includes beta-blocker eye drops used to treat glaucoma.
Smoking and cigarette fumes - smoking makes asthma much worse and every effort should be made to stop smoking. Passive smoking can make asthma worse too. Even where adults smoke away from children, smoke on clothes, hair, etc, may make asthma worse.
Other fumes and chemicals - for example, fumes from paints, solvents and pollution. The increase in air pollution may be a reason why asthma is becoming more common. Details about current levels of air pollution, are available from The Daily Air Quality Index, which can be found on the Department for Environment Food and Rural Affairs (DEFRA) website (see further reading for link).
Certain pillows and mattresses - feathers in pillows may trigger symptoms. It is thought that some people develop asthma symptoms from chemicals (isocyanates/methyl ethyl ketones, etc) that are emitted in very low quantities from memory foam pillows and mattress toppers.
Emotion - asthma is not due to 'nerves'; however, such things as stress, emotional upset, or laughing may trigger symptoms.
Allergies to animals - for example, pet cats and dogs, and horses. Some people notice that their symptoms become worse when close to certain animals.
House dust mites - this is a tiny creature which lives in mattresses and other fabrics around the home. Allergy to house dust mites may make symptoms worse. It is impossible to get rid of house dust mite completely.. However, if symptoms are difficult to control with treatment and allergy to house dust mite has been confirmed, it may be worth considering trying to reduce their number. See the separate leaflet called House Dust Mite and Pet Allergy for more details.
Some foods - this is uncommon. Food is not thought to be a trigger in most cases.
Some people only develop asthma symptoms when exposed to a certain trigger - for example, exercise-induced asthma. However, there are some people who only develop symptoms when they exercise; the rest of the time they are fine. Another example is that some people only develop symptoms when exposed to specific chemicals.
Continue reading below
How is asthma diagnosed?
In the past, many cases of asthma were diagnosed on the basis of typical symptoms. However, these days guidelines recommend that doctors perform tests to confirm the diagnosis.
Spirometry
Spirometry is a test which measures how much air can be blown out into a machine called a spirometer. Two results are important:
The amount of air that can be blown out in one second - called forced expiratory volume in one second (FEV1).
The total amount that can be blown out in one breath - called forced vital capacity (FVC).
Age, height and sex affect lung volume. So, spirometry results are compared with a graph showing the average predicted for age, height and sex.
A value is calculated from the amount of air that can be blown out in one second divided by the total amount of air that can be blown out in one breath (called FEV1:FVC ratio).
A low value indicates narrowed airways which are typical in asthma (but a low value can occur in other conditions too). Therefore, spirometry may be repeated after treatment with a reliever inhaler. An improvement in the value after treatment to open up the airways, is typical of asthma.
Note: spirometry may be normal in people with asthma who do not have any symptoms when the test is done. Remember, the symptoms of asthma typically come and go. Therefore, a normal result does not rule out asthma. However, if symptoms suggest asthma, ideally the test should be repeated when symptoms are present.
See the separate leaflet called Spirometry for more details.
Assessment with a peak flow meter
This is an alternative test. A peak flow meter is a small device to blow into. A doctor or nurse will demonstrate how to use a peak flow meter. It measures the speed of air that can be blow out of the lungs.
If the airways are narrowed, the peak flow reading will be lower than expected for age, height and sex.
Untreated asthma will usually cause low and variable peak flow readings. Also with asthma, peak flow readings in the morning are usually lower than in the evening.
It is useful to keep a diary of peak flow readings over about two weeks. Typically, a person with asthma will usually have low and variable peak flow readings over several days. Peak flow readings improve when the narrowed airways are opened up with treatment.
Regular peak flow readings can be used to help assess how well the treatment is working. See the separate leaflet called Peak Flow Meter for Asthma and our editorial article called Peak flow diary for more details.
FeNO test
The National Institute for Health and Care Excellence (NICE) issued guidance in 2017 that most patients suspected of having asthma should have a fractional exhaled nitrous oxide (FeNO) test. A FeNO test measures the levels of nitric oxide in the breath.
Increased levels are thought to be related to lung inflammation and asthma. A GP may be able to provide this test, or refer to a local asthma clinic for further assessment, including an FeNO test.
Other tests
If the diagnosis remains in doubt then a specialist may perform further, more complex tests. However, these are not needed in most cases.
Although not recommended for diagnosis, allergy tests may be used to identify any asthma triggers after a diagnosis of asthma has been made. See also the separate leaflet called Allergies.
Diagnosing asthma in children under 5 years old
Children under 5 often can't do the tests above accurately. So guidelines recommend that if a doctor suspects that an under 5-year-old has asthma, they offer treatment based on symptoms. However, once they reach the age of 5, they should have one or more of the tests below if they still have symptoms.
Diagnosing asthma in 5- to 16-year-olds
The European Respiratory Society (ERS) has suggested the main tests that should be used to diagnose asthma in young people. These include:
Spirometry.
FeNO (see above).
Using a 'reliever' inhaler to compare peak flow within a few minutes compared to before using it.
Some other specialist tests if the tests above don't give a diagnosis either way.
Asthma treatment
For most people with asthma, the symptoms can be prevented most of the time with treatment. This allows a person with asthma to get on with a normal life at school, work, sport, etc.
Inhalers
Most people with asthma are treated with inhalers. Inhalers deliver a small dose of medicine directly to the airways. The dose is enough to treat the airways. However, the amount of medicine that gets into the rest of the body is small so side-effects are unlikely, or minor.
There are various inhaler devices made by different companies. Different ones suit different people. A doctor or nurse will advise on the different types. See the separate leaflet called Asthma Inhalers for more details.
Bone strength (density) may be reduced following long-term use of high doses of inhaled steroids. Therefore people who regularly use steroid inhalers for asthma need to make sure they have a good supply of calcium in their diet. Milk and dairy are good sources of calcium. Other good dietary sources of calcium include bread, some vegetables (curly kale, okra, spinach and watercress) and some fruits (for example, dried apricots). See the separate leaflet called Preventing Steroid-induced Osteoporosis for more details.
Medicines delivered by inhalers can be grouped into relievers, preventers and long-acting bronchodilators (medicines that keep the airway open for a longer time):
Reliever inhalers
This type of inhaler is taken as needed to ease symptoms. The medicine in a reliever inhaler relaxes the muscle in the airways. This makes the airways open wider and symptoms usually quickly ease.
These medicines are also called bronchodilators, as they widen (dilate) the bronchi and airways (bronchioles). There are several different reliever medicines - for example, salbutamol (Ventolin®)and terbutaline.
If a reliever inhaler is needed three times a week or more to ease symptoms, a preventer inhaler is usually advised.
Preventer inhalers
This is taken every day to prevent symptoms from developing. The medicine commonly used in preventer inhalers is a steroid. Steroids work by reducing the inflammation in the airways.
When the inflammation has gone, the airways are much less likely to become narrow and cause symptoms. It takes 7-14 days for the steroid in a preventer inhaler to build up its effect. Therefore, it will not give any immediate relief of symptoms.
However, after a week or so of treatment, the symptoms have often gone, or are much reduced. It can take up to six weeks for maximum benefit.
The preventer inhaler should be used every day even when symptoms have gone - this is to prevent symptoms from coming back. A reliever inhaler should then not be needed very often (if at all).
Long-acting bronchodilators
These may be advised in addition to a preventer inhaler. Long-acting bronchodilators relieve symptoms as they widen the lung airways but work for longer than reliever inhalers. The medicines in these inhalers work for up to 12 hours after each dose has been taken.
They include salmeterol and formoterol. (Some brands of inhaler contain a steroid plus a long-acting bronchodilator for convenience.) A long-acting bronchodilator may be needed if symptoms are not fully controlled by the preventer inhaler alone.
Spacer devices
These devices are used with some types of inhaler. They are commonly used by children; however, many adults also use them. A spacer is like a small plastic chamber that attaches to the inhaler. It holds the medicine like a reservoir when the inhaler is pressed.
A valve at the mouth end makes sure that the medicine is kept within the spacer until breathing it in. When breathing out, the valve closes. Good co-ordination is not needed to inhale the medicine from a spacer device.
A face mask can be fitted on to some types of spacers instead of a mouthpiece. This is sometimes done for babies and young children who can then use the inhaler simply by breathing in and out normally through the mask.
Tablets to open up the airways
Most people do not need tablets, as inhalers usually work well. However, in some cases a tablet (or medicine in liquid form for children) is prescribed in addition to inhalers if symptoms are not fully eased by inhalers alone.
Various tablets may be used which aim to open up the airways. Some young children use liquid medication instead of inhalers.
Leukotriene receptor antagonists (LTRAs)
Chemicals called leukotrienes are produced in some people who have asthma which is triggered by an allergic reaction (eg, pollen) or sometimes exercise. LTRAs such as montelukast act by blocking the action of these chemicals.
Montelukast comes in the form of tablets or granules. In people whose asthma is not well controlled by a reliever inhaler and a preventer inhaler, NICE recommends trying an LTRA before adding a long-acting bronchodilator inhaler.
Steroid tablets
A short course of steroid tablets (such as prednisolone) is sometimes needed to ease a severe or prolonged attack of asthma. Steroid tablets are good at reducing the inflammation in the airways. For example, a severe attack may occur with a cold or a chest infection.
Some people worry about taking steroid tablets. However, a short course of steroid tablets (for a week) usually works very well and is unlikely to cause side-effects. Most of the side-effects caused by steroid tablets occur if they are taken for a long time (more than several months), or after a lot of short courses of high-dose steroids over a short period of time.
Biologic therapies
Monoclonal antibodies are biologic treatments used for treating many diseases. They work by targeting specific cells and proteins to make the disease better. In asthma, they work by interfering with the immune system to reduce inflammation in the airways.
These are medicines that are only used in a small number of people who have severe persistent allergic asthma that have not been controlled by other treatments. So, it is not a common treatment.
Currently there are five treatments used in the NHS and recommended by NICE:
Mepolizumab (Nucala).
Reslizumab (Cinqaero®).
Benralizumab (Fasenra®).
Omalizumab (Xolair®).
Dupilumab (Dupixent®).
Tezepelumab (Tezspire®).
They are most commonly given by injection. These treatments can only be started by a specialist. Each medication has its own rules on when they can be started by a specialist. If needed, an asthma specialist will go into much more detail about that specific one.
What are the dosages of treatment?
Everyone is different. The correct dose of a preventer inhaler is the lowest dose that prevents symptoms. A doctor may prescribe a high dose of a preventer inhaler at first, to 'get on top of symptoms' quickly. When symptoms have gone, the dose may then be reduced by a little every few weeks. The aim is to find the lowest regular dose that keeps symptoms away.
Some people with asthma put up with symptoms. They may think that it is normal still to have some symptoms even when they are on treatment. A common example is a night-time cough which can cause disturbed sleep.
But, if this occurs and symptoms are not fully controlled, it is very important to see a doctor or nurse for an asthma review. Symptoms can often be prevented - for example, by adjusting the dose of the preventer inhaler, or by adding in a long-acting bronchodilator.
A typical treatment plan for asthma
A common treatment plan for a typical person with moderate asthma is:
A preventer inhaler (usually a steroid inhaler), taken each morning and at bedtime. This usually prevents symptoms throughout the day and night.
A reliever inhaler may be needed now and then if breakthrough symptoms occur. For example, if symptoms flare up with a cough or cold.
If exercise or sport causes symptoms then a dose of a reliever inhaler just before the exercise usually prevents symptoms.
The dose of the preventer inhaler may need to be increased for a while during a cough or cold, or during the hay fever season.
Some people may need to add in an LTRA and/or a long-acting bronchodilator if symptoms are not controlled with the above.
At first, adjusting doses of inhalers is usually done on the advice of a doctor or nurse. An asthma action plan should be agreed with a doctor or nurse.
Asthma action plan
An asthma action plan is a plan agreed by anyone with asthma with a doctor or nurse. The plan enables changes to the dose of the inhalers, depending on symptoms and/or peak flow readings. The plan is tailored to each individual. It is written down, usually on a standard form, so that it's clear what to do at any time.
The plan should include:
What to do when unwell - for example, with a cold - and when to seek help.
What to do if symptoms become worse with hay fever or exercise.
A discussion on ways to reduce exposure to air pollution, both indoors and outdoors. If asthma is triggered by household sprays, air fresheners or aerosols, it is important to avoid using them or use non-spray alternatives instead. Mould and house dust mites in the home can also make asthma worse. If problems with mould in the home, a GP can sometimes help request a housing assessment from the local authority.
Research studies suggest that people who complete personal asthma action plans find it easier to manage their asthma symptoms and that their plan helps them to go about their lives as normal. Asthma+Lung UK provides asthma action plans which can be downloaded (see 'Further Reading' below).
Does asthma go away?
There is no once-and-for-all cure. However, about half of the children who develop asthma grow out of it by the time they are adults.
For many adults, asthma is variable with some good spells and some spells that are not so good. Some people are worse in the winter months and some are worse in the hay fever season. Although not curable, asthma is treatable. Stepping up the treatment for a while during bad spells will often control symptoms.
Don't underestimate asthma
Because modern management is so effective, many people with asthma are well controlled. However, this has led to the belief that asthma is a mild and even trivial condition.
The fact is that when asthma goes wrong, it can do so quickly. Deaths from asthma are rising. More than 1,400 people died from asthma in 2020, representing an increase of nearly 4% over the previous year..
There are several things to lower the risk of asthma getting out of control:
Make sure you are accessing basic asthma care. This should involve at least an annual review from your GP or asthma nurse, including an inhaler technique check. You should be given a written asthma action plan.
Take your medication as prescribed.
If you develop symptoms which are not responding to your action plan, seek advice from a healthcare professional immediately.
"It's only asthma" is not a phrase that should pass anybody's lips.
Some other general points about asthma
It is vital to learn how to use inhalers correctly. In some people, symptoms persist simply because they do not use their inhaler properly and the medicine from the inhaler does not get into the airways properly. See a pharmacist or practice nurse if not sure if using asthma inhalers properly.
See a doctor or nurse if symptoms are not fully controlled, or if they are getting worse. For example, if:
A night-time cough or wheeze is troublesome.
Sport is being affected by symptoms.
Peak flow readings are lower than normal.
A reliever inhaler is needed more often than usual.
An adjustment in inhaler timings or doses may control these symptoms.See a doctor urgently if you develop severe symptoms that are not eased by a reliever inhaler. In particular, if having difficulty talking due to shortness of breath. This may need emergency treatment with high-dose reliever medicine and other treatments, sometimes in hospital. A severe asthma attack can be life-threatening. In this case, call for an ambulance.
Have an influenza immunisation every autumn (the flu jab) if need continuous or repeated use of high-dose inhaled steroids and/or take steroid tablets and/or have had an episode of asthma which needed hospital admission.
Further reading and references
- Inhaled corticosteroids for the treatment of chronic asthma in children under the age of 12 years; NICE Technology appraisal guidance, November 2007
- Inhaled corticosteroids for the treatment of chronic asthma in adults and in children aged 12 years and over; NICE Technology appraisal guidance, March 2008
- Global Initiative for Asthma (GINA)
- Asthma + Lung UK
- Asthma: diagnosis, monitoring and chronic asthma management; NICE Guideline (November 2017 - last updated April 2021)
- British guideline on the management of asthma; Scottish Intercollegiate Guidelines Network (SIGN), British Thoracic Society (BTS), NHS Scotland (2003 - revised July 2019)
- Corticosteroids - inhaled; NICE CKS, May 2020 (UK access only)
- Air pollution forecast; Department for Environment Food and Rural Affairs (DEFRA)
- Indoor air quality at home. NICE guideline [NG149], January 2020
- Asthma; NICE CKS, August 2023 (UK access only)
- Your asthma action plan; Asthma and Lung UK.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 18 Nov 2028
20 Nov 2023 | Latest version

Feeling unwell?
Assess your symptoms online for free

