Hip problems
Peer reviewed by Dr Caroline Wiggins, MRCGP Last updated by Dr Rachel Hudson, MRCGPLast updated 20 Mar 2023
Meets Patient’s editorial guidelines
Hip problems are pretty common. The cause may be obvious, like an injury that comes on suddenly while playing sports. Sometimes the cause is not as clear and you will need to be checked out by a doctor or physiotherapist.
In this article:
Continue reading below
How common are hip problems?
Hip problems are common and can be an occupational hazard. They may occur as a result of getting older, although they may also affect younger people. They are usually due to a problem with the hip joint. Joints are junctions between two bones.
In the UK alone, 8.5 million people live with joint pain, and hips are prime candidates. Pain in your hip can also come from your lower back or from any of the structures near your hip joint. Your doctor or physiotherapist will check this out.
Patient picks for Joint problems
Causes of hip problems in adults
Osteoarthritis
Osteoarthritis is the most common cause of hip problems. Your joints go through constant wear and tear, and keep repairing themselves. Sometimes, the repair process can't keep up with the damage and osteoarthritis develops. Wear and tear increase with age and body weight. Injury or deformity of your joints - from a break, a joint infection or other damage - also makes you more prone to osteoarthritis.
Women suffer more often than men, and it can sometimes run in families. Hip osteoarthritis causes pain (usually felt in the groin) and stiffness. This can affect your ability to walk and may eventually mean that you would benefit from a hip replacement. See the separate leaflet called Hip Replacement.
Greater trochanteric pain syndrome
Another very common cause of hip pain, it is particularly common in middle-aged women but can also affect younger people, especially runners and footballers. Unlike hip joint pain, when the pain is usually felt in the groin, greater trochanteric pain syndrome gives you pain on the outside of the top of your thigh. See the separate leaflet called Greater Trochanteric Pain Syndrome (Trochanteric Bursitis).
Hip fracture (broken hip)
A very common fracture in older people that usually happens after a fall. A hip fracture is the most common reason for being admitted as an emergency to a bone (orthopaedic) ward. This is because it is usually necessary to have an operation to fix a hip fracture. Hip fractures are most likely in someone who has a condition called osteoporosis, which makes the bones weaker and more likely to break. See the separate leaflet called Hip Fracture.
Femoroacetabular impingement (FAI)
FAI happens because of slight abnormalities in the shape of the 'ball-and-socket'. The movement between the bones can then cause damage to the cartilage on the surfaces and to the other tissues around the edge of the hip joint. It is not known how common FAI is but it is increasingly thought to be a common cause of hip problems, particularly in young adults.
Rheumatoid arthritis
Rheumatoid arthritis is the second most common kind of arthritis. It's an autoimmune disease - your body's immune system attacks itself. Often many joints are affected at the same time, but in the early stages it tends to cause hand and foot problems and doesn't often cause hip problems.
Septic arthritis
Septic arthritis is an infection in a joint. It is a rare cause of a hip problem but is serious and needs urgent treatment. It can affect people of any age. See the separate leaflet called Septic Arthritis.
Reactive arthritis
Reactive arthritis is inflammation of a joint that occurs in response to infection in the body. See the separate leaflet called Reactive Arthritis.
Soft tissue pain and referred pain
Soft tissue injuries such as muscular strains or inflamed tendons - eg, from exercise - can cause pain, swelling, inflammation and fluid build-up in the affected muscle or area.
Pain can be referred to, or from, the hip. For example, a back problem can cause pain in the hip area and hip problems can be felt as pain in the knee on the same side of the body.
What causes hip pain?
Continue reading below
Causes of hip problems in children
Developmental dysplasia of the hip (DDH)
A painless condition that can affect newborns, DDH makes the hip joint unstable so that it can dislocate (something that very rarely happens to the hip joint otherwise). It is important to pick this up and treat it, as if it isn't treated the joint won't develop normally. See the separate leaflet called Developmental Dysplasia of the Hip.
Perthes' disease
Older children, particularly boys, although girls may be affected, can develop a problem with the blood vessels to the hip joint. This is called Perthes' disease. It mainly affects children aged over 4 years but younger than 13 years. Often the first symptom is that the child develops a limp. The hip is not always painful. See the separate leaflet called Perthes' Disease.
Slipped capital femoral epiphysis
Older children can also develop a problem called slipped capital femoral epiphysis. This hip problem affects a slightly older age group than Perthes' disease. It usually causes a problem around the age of 11, 12 or 13 years. The main symptoms are pain around the hip or knee, and limping. See the separate leaflet called Slipped Capital Femoral Epiphysis.
Septic arthritis (see above) can also affect children.
Symptoms of hip problems
Pain (usually in the groin if the hip joint itself is affected), especially on movement or weight bearing. Referred pain may also occur - eg, down the thigh to the knee.
Stiffness.
Giving way of the leg.
Loss of muscle bulk of the thigh.
Difficulty walking.
Continue reading below
How are hip problems diagnosed?
Your doctor or physiotherapist should be able to make a diagnosis on the basis of your symptoms and examining you. You may need any of the following tests, depending on what they suspect to be the cause of your hip problem:
X-ray of your hip. Knee or spine X-ray may also be requested Note: X-ray changes don't always match the severity of your symptoms and therefore aren't always helpful.
Rarely a bone scan may be suggested.
How are hip problems treated?
Medication
Anti-inflammatory and pain relief medication can be taken to help reduce the pain caused by hip problems.
Physiotherapy
Including stretching and strengthening exercises and treatments such as massage, hydrotherapy and taping.
Surgery
Some causes of hip problems may require an operation such as a hip replacement or arthroscopy (a keyhole procedure).
Injections
Some conditions, such as arthritis or trochanteric bursitis, may be treated with an injection of a steroid and local anaesthetic into the area of concern to relieve pain and inflammation.
Weight loss and increasing physical activity
To reduce the load on the joint and increase muscle strength and support. Losing weight can be an extremely effective way to reduce pain from some long-term hip conditions.
RICE (rest, ice, compression, elevation)
As with most acute muscular strains and injuries with inflammation, these measures (although really just rest and ice with hips) can help in the first few days.
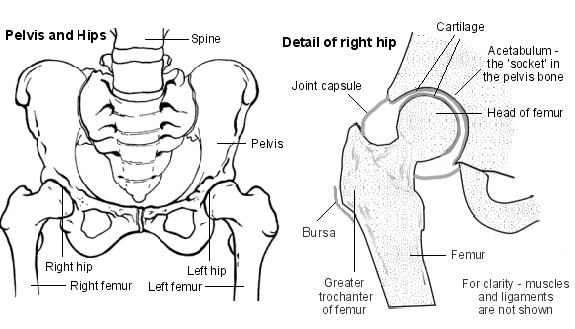
What does the hip joint look like?
Your hip joint is known as a 'ball-and-socket' joint. It allows you to move your hip. The ball (head) of your thigh bone (femur) fits into the socket of your pelvic bone to make your hip joint. This hip socket is called the acetabulum. The adjoining bone ends are covered in a tough, smooth material called cartilage, which lets the bones glide smoothly over each other.
The joint is surrounded by a strong but flexible capsule. It helps to give stability to the joint and also produces a fluid called synovial fluid to give lubrication and help joint movement. Ligaments across the joints keep it all stable.
Trochanteric bursa
Further reading and references
- Arthroscopic femoro-acetabular surgery for hip impingement syndrome, NICE Interventional Procedure Guideline (2011)
- Chamberlain R; Hip Pain in Adults: Evaluation and Differential Diagnosis. Am Fam Physician. 2021 Jan 15;103(2):81-89.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Feb 2028
20 Mar 2023 | Latest version
Last updated by
Dr Rachel Hudson, MRCGP
Peer reviewed by
Dr Caroline Wiggins, MRCGP
21 Feb 2018 | Originally published
Authored by:
Dr Jacqueline Payne, FRCGP

Feeling unwell?
Assess your symptoms online for free

