ECG identification of conduction disorders
Peer reviewed by Dr Laurence KnottLast updated by Dr Colin Tidy, MRCGPLast updated 21 Mar 2022
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Electrocardiogram article more useful, or one of our other health articles.
In this article:
See also the separate ECG A Methodical Approach, ECG Identification of Arrhythmias, Supraventricular Tachycardia in Adults, Paediatric Supraventricular Tachycardia, Ventricular Tachycardias, Narrow Complex Tachycardias and Broad Complex Tachycardias articles.
Continue reading below
The heart's pacemaker and conducting systems - electrocardiogram correlations
Each normal cardiac electrical cycle starts with the generation of a regular depolarisation in a specialised area of cardiac tissue in the right atrial wall, known as the sinoatrial (SA) node.
The electrical impulse spreads from here as a wave of depolarisation that causes atrial contraction. This corresponds with the P wave of the electrocardiogram (ECG).
The process of spread of the electrical impulse from the SA node to the myocardium corresponds with the P-R interval of the ECG. The spread of conduction is as follows:
The depolarising wave reaches the atrioventricular (AV) node at the AV junction, where the electrical impulse is conducted more slowly by another specialised area of cardiac tissue.
From here, the wave of depolarisation is then rapidly conducted down a specialised bundle of tissue in the interventricular septum, known as the bundle of His.
This bundle divides in its course in the septum into the right and left bundle branches that conduct the electrical impulse to the right and left ventricular myocardium respectively.
A nebulous network of smaller conducting fibres known as Purkinje's fibres spreads the electrical impulse, from the bundles, throughout the myocardial tissues, causing ventricular systole.
The spread of the wave of depolarisation through the myocardium and consequent ventricular activation corresponds with the QRS complex of the ECG.
The T wave that follows the QRS complex represents the repolarisation of the ventricular myocardium, ready for the next heartbeat.
Atrioventricular conduction abnormalities
ECG nomenclature
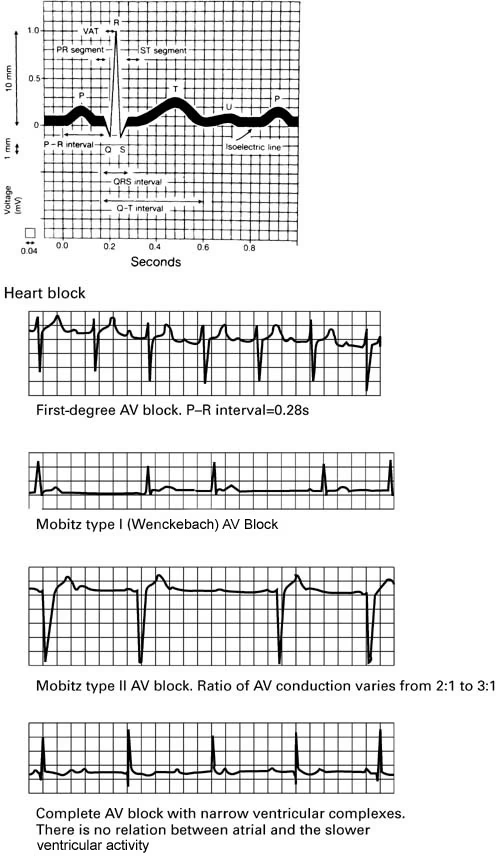
First-degree heart block
First-degree AV block is defined as a PR interval longer than 0.2 seconds1 . Each atrial activation leads to a ventricular activation with a 1:1 correspondence.
It can be due to anatomical or functional impairment in the conduction system and can produce a clinical condition similar to that of the pacemaker syndrome when the PR interval is greater than 0.3 seconds2 .
It is a relatively common condition with a prevalence of approximately 7%3 . It is also commonly found in highly trained athletes with supranormal cardiovagal tone. It is usually asymptomatic and often an incidental ECG finding. Possible pathological causes are listed below:
Following myocardial infarction.
Intrinsic congenital or acquired AV nodal disease.
Electrolyte derangement.
Medication-induced (particularly disopyramide, flecainide, propafenone, beta-blockers, calcium-channel blockers, digoxin and magnesium).
The condition does not usually require investigation or treatment if it is asymptomatic, particularly in young, healthy people. If there is reason to suspect metabolic disturbance then it might be worth checking U&Es. If the patient has experienced cardiac symptoms or there is reason to suspect occult coronary heart disease then cardiological referral may be appropriate. Follow-up ECGs on an annual basis can be used to monitor for progression of the heart block if a pathological cause is suspected, or the patient is on AV node blocking medication.
First-degree heart block is a relative contra-indication to the use of drugs that may delay AV nodal conduction (such as those listed above) and they must be used with caution in this scenario and preferably under specialised supervision.
Increased risks of atrial fibrillation, pacemaker implantation and all-cause mortality have been found6 .
Second-degree heart block
This is prolongation of the P-R interval with intermittent failure of conduction of atrial impulses to the ventricles, causing 'dropped' beats. It is usually associated with cardiac pathology. There are two types7 :
Mobitz type I AV block (also known as Wenckebach's block/phenomenon)
There is progressive prolongation of the P-R interval following each atrial impulse, until an atrial impulse fails to be conducted to the ventricles.
A ventricular impulse is 'dropped' and, following this, AV conduction recovers to its baseline optimal level and the cycle repeats itself.
The increments in AV nodal conduction are usually greatest at the start of Wenckebach's sequence, leading to the paradoxical finding that, as the sequence progresses towards the 'dropped' beat, the QRS complexes actually move closer together.
Sometimes the non-conducted P wave can be seen superimposed on the preceding beat's T wave, making it appear larger or biphasic.
The ECG trace will not necessarily start with the shortest P-R interval (as it does in most textbook illustrations of the phenomenon), so a long trace and careful interpretation may be needed to see the characteristic pattern8 .
The condition is usually due to impaired AV nodal conduction, so the QRS complexes tend to be of normal width.
Mobitz type II AV block
There is intermittent failure of conduction of atrial impulses to the ventricles without progressive lengthening of the P-R interval, thus the P-R interval of conducted beats is constant7 .
There may be a regular pattern to the number of atrial impulses that do actually lead to ventricular activation - eg, every second or third atrial impulse may 'get through', termed 2:1 and 3:1 block respectively.
Not all cases of Mobitz type II AV block have this regular relationship and the ratio between conducted and non-conducted impulses can vary.
The non-conducted P waves may be difficult to see if they are superimposed on the preceding T wave8 .
Usually due to impaired conduction in the bundle of His or bundle branches, so the QRS complexes tend to be wider than normal.
If type I block is due to AV nodal disease then it is usually relatively benign and non-progressive, with a good long-term prognosis.
Type I block caused by His-Purkinje abnormalities (an unusual subgroup) is likely to progress to complete heart block. Type II block often progresses to complete heart block and so has a poorer prognosis. Type II block may cause symptoms in the form of Stokes-Adams attacks, where episodes of syncope are caused by significant slowing of the ventricular rate.
Possible causes include9 :
Medication - digoxin, beta-blockers, calcium-channel blockers and other anti-arrhythmics.
Structural abnormalities of the heart - eg, congenital abnormalities (and their surgical correction) and valvular heart disease (especially aortic stenosis and following aortic valve replacement). Around 3% of patients with underlying structural heart disease develop some form of second-degree block.
Idiopathic age-related fibrosis of the cardiac matrix.
Coronary heart disease and myocardial infarction.
Inflammatory cardiac disease such as SLE, ankylosing spondylitis, reactive arthritis, dermatomyositis, rheumatoid arthritis, scleroderma, endocarditis, myocarditis, Lyme disease and rheumatic fever.
Cardiac infiltration caused by tumour, leukaemia, amyloidosis, haemochromatosis and sarcoidosis.
Endocrine and metabolic disorders such as hyperkalaemia, hypermagnesaemia and Addison's disease.
Disorders of the myocardium, caused by cardiomyopathies and muscular dystrophies.
Familial cases are usually inherited in an autosomal dominant fashion10 .
There are cases of second-degree block in highly trained athletes which improves with exercise; rarely it causes symptoms.
Patients with second-degree AV block should be referred for cardiological assessment (after adjusting the dose of or discontinuing any culprit medications), where more detailed investigations such as 24-hour ECG monitoring, electrophysiological studies, cardiac imaging and cardiac catheterisation may be carried out.
Acutely symptomatic patients with low ventricular rates can be treated with atropine and/or temporary pacemaker insertion. Treatment by insertion of a permanent cardiac pacemaker may be required, particularly for Mobitz type II AV block11 .
Third-degree or complete heart block (CHB)
This occurs when there is complete failure of transmission of atrial impulses to the ventricles. P waves will occur regularly, usually at a rate of around 75 beats per minute (bpm). They are completely unconnected to the rhythm of the QRS complexes9 . Congenital CHB is very strongly associated with anti-Ro antibodies found in SLE12 .
Third-degree AV block can occur at the AV node or infra-nodally in the His-Purkinje system.
In nodal block, the new, subsidiary distal pacemaker will arise above, or in the bundle of His:
Unless there is accompanying bundle branch block, the QRS complexes in such cases will be narrow.
These pacemakers normally fire reliably and at a reasonably rapid rate (approximately 45-60 bpm). They increase their rate in response to exercise and atropine.
Patients with this type of CHB may remain asymptomatic for appreciable periods of time and are usually haemodynamically stable. They may experience mild or nonspecific symptoms, such as fatigue, dizziness, reduced exercise tolerance, chest discomfort and palpitations.
AV blocks occurring in or below the bundle of His usually have a subsidiary pacemaker in the right or left bundle branches:
These pacemakers produce wide QRS complexes and are usually slow (<45 bpm).
Patients with this type of CHB are usually haemodynamically compromised and overtly symptomatic. Common symptoms include syncope, confusion, dyspnoea, severe chest pain or decompensation of pre-existing cardiac failure. Sudden death may occur.
Complete AV block can co-exist with cases of atrial fibrillation or flutter where there are no P waves. The term AV dissociation should be reserved for cases where the ventricular escape rate is faster than the atrial rate. It should be distinguished from the more common types of third-degree AV block. Sometimes in this scenario, the occasional atrial impulse will fire at just the right moment to 'capture' the ventricles via the AV node before the next escape pacemaker discharge, causing premature ventricular activation. This is termed AV dissociation with capture beats. It may occur during acute myocardial infarction or thrombolysis and does not usually require pacemaker insertion in a haemodynamically stable patient (which is the 'norm' for this situation)8 .
CHB may occur as a progression from second-degree heart block, or acutely, particularly after myocardial infarction; thus, its causative conditions are as listed above for second-degree heart block. It is treated acutely with atropine and temporary pacemaker insertion if required. CHB is the most common ECG indication for permanent pacemaker insertion13 .
Abnormally fast AV conduction
This occurs as part of the Wolff-Parkinson-White syndrome, one of the ventricular pre-excitation syndromes. Follow the link for detailed information.
Continue reading below
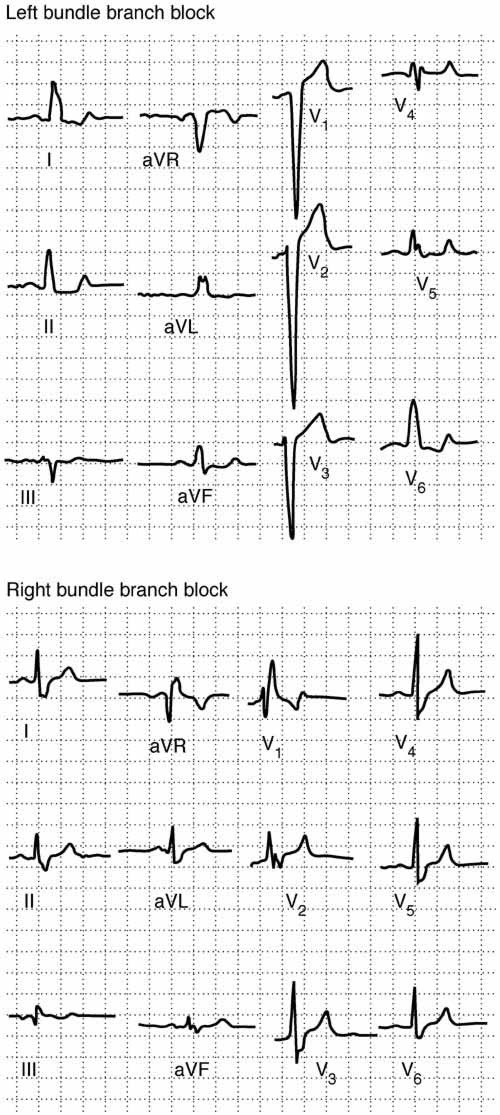
Bundle branch conduction abnormalities
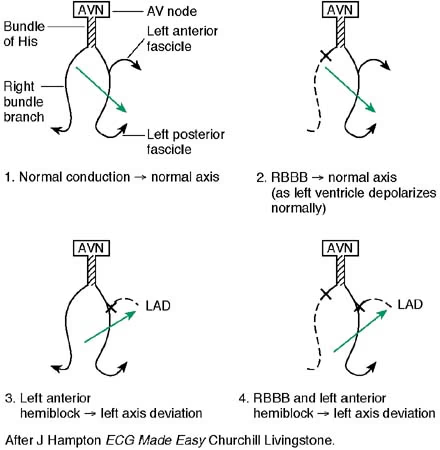
The bundle of His divides into left and right bundle branches. The left bundle branch subdivides further into the anterior and posterior hemi-fascicles. Abnormal conduction through the bundles or hemi-fascicles causes characteristic lengthening of the QRS complex and may cause abnormalities in the axes of the QRS complexes in the chest leads (V1-V6), or the limb leads (I, II, aVF, III, aVR and aVL).
Interpretation of the cardiac axis requires an understanding of the hexaxial reference system where activity in the various limb leads reflects the direction of the electrical impulse in the frontal plane (ie looking at the body from the front). See the diagram below for further information on understanding the axis of cardiac conduction.
In complete bundle branch block, the QRS complex is prolonged to >0.12 seconds (three small squares). In partial bundle branch block the QRS duration is 0.10-0.11 seconds but the characteristic axis deviations and wave-pattern abnormalities are still seen in the relevant leads.
The hexaxial reference system used to describe the mean cardiac axis in the frontal plane
The hexaxial reference system
By: MoodyGroove, User: Mysid, Public domain, via Wikimedia Commons
Left bundle branch block (LBBB) - see diagram below
The interventricular septum is normally activated by the left bundle branch. When its conduction is slowed, the septum is activated 'in reverse' by impulses from the right bundle branch. This has the following electrical consequences:
A prolonged QRS complex.
Replacement of the usual small Q wave in the left ventricular leads (V5, V6, I and aVL) by a large, prolonged positive R wave.
Secondary R waves in the left ventricular leads, causing an M-shaped pattern in leads I and V4, V5 or V6.
Left axis deviation may be seen.
Right bundle branch block (RBBB) - see diagram below
The activation of the right ventricle is delayed and slowed conduction from the left to right ventricles results in:
A prolonged QRS complex.
A secondary R wave in leads orientated to the right ventricle (V1 and V2) - giving an M-shaped ventricular complex in these leads.
T-wave inversion may be seen in leads V1 and V2.
A deep, slurred S wave is seen in leads I and V6.
Examples of LBBB and RBBB14
Right and left bundle branch block
Left anterior fascicular (or hemi) block - see diagram below
Left axis deviation (usually between −45° and −90°).
Small initial R wave in leads II and aVF.
No other cause for left axis deviation is identified.
Left posterior fascicular (or hemi) block
Right axis deviation (mean frontal plane axis clockwise to 90°).
No other cause of right axis deviation such as right ventricular hypertrophy/strain or young, thin-built patient is identified.
Bifascicular block - see diagram below
Bifascicular block is the combination of RBBB with either left anterior fascicular block or left posterior fascicular block.
RBBB with left anterior fascicular block is the more common of the two patterns.
The ECG will show features of RBBB plus either left or right axis deviation, depending on which of the fascicular blocks is present.
Schematic diagram to aid understanding of the axis deviations occurring in fascicular block
ECG AXIS AND CONDUCTION DEFECTS
Further reading and references
- ECG Image Index; ECG Learning Center
- ECG Library
- Easy ECG
- Carroz P, Delay D, Girod G; Pseudo-pacemaker syndrome in a young woman with first-degree atrio-ventricular Europace. 2010 Apr;12(4):594-6. Epub 2009 Nov 27.
- Barold SS, Ilercil A, Leonelli F, et al; First-degree atrioventricular block. Clinical manifestations, indications for pacing, pacemaker management & consequences during cardiac resynchronization. J Interv Card Electrophysiol. 2006 Nov;17(2):139-52. Epub 2007 Mar 2.
- Upshaw CB Jr; Comparison of the prevalence of first-degree atrioventricular block in African-American and in Caucasian patients: an electrocardiographic study III. J Natl Med Assoc. 2004 Jun;96(6):756-60.
- Costello JM, Alexander ME, Greco KM, et al; Lyme carditis in children: presentation, predictive factors, and clinical course. Pediatrics. 2009 May;123(5):e835-41.
- Makaryus JN, Catanzaro JN, Goldberg S, et al; Rapid progression of atrioventricular nodal blockade in a patient with systemic lupus erythematosus. Am J Emerg Med. 2008 Oct;26(8):967.e5-7.
- Cheng S, Keyes MJ, Larson MG, et al; Long-term outcomes in individuals with prolonged PR interval or first-degree atrioventricular block. JAMA. 2009 Jun 24;301(24):2571-7.
- Silverman ME, Upshaw CB Jr, Lange HW; Woldemar Mobitz and His 1924 classification of second-degree atrioventricular block. Circulation. 2004 Aug 31;110(9):1162-7.
- Cardiac Arrhythmias (8th ed) 2013
- Da Costa D et al; Bradycardias and atrioventricular conduction block. BMJ 2002 2 March;324:535-538 [Full Text]; Good overview with sample traces
- Progressive Familial Heart Block, Type II, PFHB2; Online Mendelian Inheritance in Man (OMIM)
- Dual-chamber pacemakers for the treatment of symptomatic bradycardia due to sick sinus syndrome and/or atrioventricular block; NICE Technology appraisal guidance, February 2005 - last updated November 2014
- Gordon PA; Congenital heart block: clinical features and therapeutic approaches. Lupus. 2007;16(8):642-6.
- Coma Samartin R, Sancho-Tello de Carranza MJ, Ruiz Mateas F, et al; Spanish Pacemaker Registry. Seventh official report of the Spanish Society of Cardiology Working Group on Cardiac Pacing (2009). Rev Esp Cardiol. 2010 Dec;63(12):1452-67.
- The ECG Made Easy (8th ed) 2013
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 20 Mar 2027
21 Mar 2022 | Latest version

Feeling unwell?
Assess your symptoms online for free