Zygomatic arch and orbital fractures
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Laurence KnottLast updated 17 Aug 2021
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Continue reading below
Overview
The orbit and zygomatic arch1
The orbit is a pear-shaped cavity, with an apex directed posteriorly, medially and slightly upwards. The upper and lower walls of the cavity are described as the roof and the floor. It is also bound by the medial and lateral walls. The orbital margin (rim) is strong and, superiorly, it contains the supraorbital notch/foramen which transmits vessels and nerves.
The zygoma forms part of the floor and lateral wall of the orbit and the zygomatic arch is an important feature in the structure and appearance of the face. The malar complex refers to the zygoma and maxillary bones (and therefore forms part of the orbital floor and lateral orbital wall). This plays a key role in the structure and function of the facial skeleton. In addition to providing support for the globe, it is the insertion site for the masseter muscle and protects the temporalis muscle and the coronoid process.
Zygomatic arch
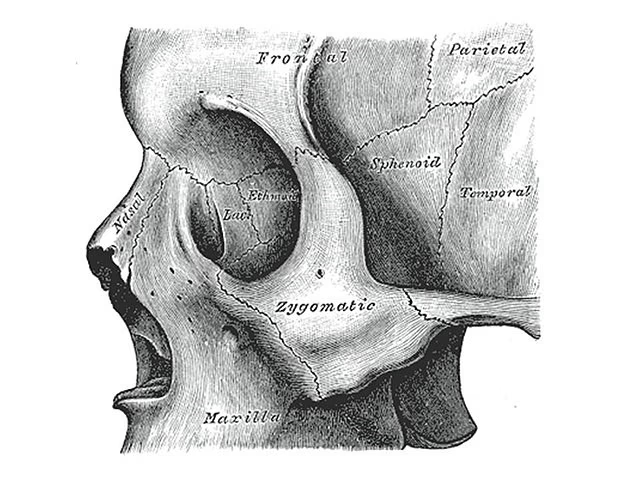
By Henry Vandyke Carter, Public domain, via Wikimedia Commons
Fractures
The most common orbital injury is a 'blowout' fracture, usually involving the orbital floor ± the medial wall. The malar complex is also commonly fractured in isolation by a blow to that area. The bones are either fractured or dislocated. The strong central part of the bone usually remains intact and the force is transmitted to the three buttresses, individually or simultaneously (a 'tripod' fracture) resulting in:
An infraorbital fracture.
Displacement of the zygomatico-frontal suture.
Fracture of the zygomatic arch.
Epidemiology
Maxillofacial fractures can have various causes, including traffic accidents, falls, assaults and sports injuries2 3 .
The incidence and causes of maxillofacial trauma and facial fractures vary widely in different regions of the world due to social, economic and cultural consequences, awareness of traffic regulations and alcohol consumption4 .
Facial fractures are rare before the age of 5 years. Children are more likely to sustain skull fractures and brain injuries than facial fractures5 .
Orbital fractures
Males are at higher risk than women of most kinds of trauma, including orbital injuries6 . The incidence of orbital fractures peaks in a bimodal fashion, at 10-40 years and again at 70 years.
Zygomatic arch fractures
After the nasal bone, the zygoma is the second most common bone of the face to be fractured. The group at highest risk is young males6 . Aetiology is usually blunt trauma to the cheek, such as involved in:
Assault
Road traffic accidents
Contact sports (less common)
Continue reading below
Assessment of potential fractures
History
Visual symptoms - diplopia can occur due to entrapment of a muscle, neural injury or a haematoma in an external ocular muscle.
Other symptoms - trismus is spasm of the masseter and it makes chewing difficult and painful. Ask about dental malocclusion. The mucosa of the maxillary sinus may be lacerated and cause epistaxis on that side. Severe pain may indicate retrobulbar haemorrhage - especially if associated with visual loss or ophthalmoplegia.
NB: if this is an alleged assault or an injury at the workplace, make detailed notes documenting timing and circumstances of injury. Where possible, take photographs.
Examination
Important information |
|---|
If this is part of a multiple trauma picture, go through the usual trauma pathway first before focusing on the area of injury(ies). Orbital injuries are often missed or misdiagnosed. The underlying bony injury and or globe injury are often more serious than initial examination suggests . |
When examining these patients, you need to look for direct damage, associated damage (eg, to structures immediately adjacent to the area, such as the eye) and more peripheral damage (eg, head injury as a result of falling backwards following a blow).
General points - look at the contour, note areas of bruising and obvious abrasions or lacerations. Look for points of tenderness on gentle palpation. Note any surgical emphysema, oedema or haemorrhage.
Ocular injury - eye injury is very common in midface trauma. Examine the lids (not forgetting the tear drainage ducts) and the globe as well as the function of the eye - see the separate Examination of the Eye article. Particular points to note (in both eyes) include:
Extent of any subconjunctival haemorrhage.
Visual acuity.
Visual fields.
Pupillary light reflex.
Colour vision/saturation.
Extraocular motility/ophthalmoplegia.
Diplopia.
Hypoglobus (lowered pupillary level).
Enopthalmos (sunken eye).
Proptosis.
Where the eye is closed by swelling, check for the integrity of the optic nerve by asking the patient to confirm presence/absence of light over the closed lid. Check also for impairment of sensation below the eye.Other injury - look for and exclude potential cervical or head injury8 .
Note that extraocular muscle entrapment can cause an oculo-cardiac reflex leading to collapse9 . Muscle entrapment can also cause nausea and vomiting.
Investigations
A plain X-ray of the skull is basic - standard views are facial, occipitomental and submento-vertical. Interpretation may be difficult - systematically check for10 :
The orbital outline - the droplet sign shows soft tissue prolapsing into the maxillary sinus in an orbital floor fracture.
The sinus outline - any opacification or fluid level in the maxillary sinus is suggestive of a fracture.
An 'elephant's trunk' - follow the zygomatic line laterally and the maxillary line medially.
The coronoid processes which should be equidistant from the maxillary line bilaterally.
CT scanning is the gold standard imaging modality. 3D reconstruction is helpful if surgical treatment is planned11 .
Orbital floor fracture
Features
This usually follows a blow from an object >5 cm (eg, a tennis ball). The force may be transmitted along the orbital rim or through the orbit, compressing the globe, which pushes into the orbital floor ('blowout' fracture). Clinical features vary with the severity of the trauma and the time between trauma and presentation. Look for:
Periorbital bruising, oedema, surgical emphysema.
Vertical diplopia (double vision, especially on looking up) with restriction of upgaze.
Enophthalmos (the eye is sunken).
Infraorbital anaesthesia (lower lid, cheek, side of nose, upper lip, upper teeth and gums).
It is worth noting that children may have a 'greenstick' fracture with significant muscle entrapment but minimal bruising (a 'white-eye blowout'). They may have nausea and vomiting, especially on upgaze.
Management
Tell the patient not to blow their nose for 10 days.
Arrange imaging as above; CT is particularly helpful. Liaise with ophthalmologists and maxillofacial surgeons (depending on local protocol).
Some cases are managed conservatively with prophylactic broad-spectrum antibiotics (eg, co-amoxiclav) and outpatient monitoring.
Surgery is required if:
This is a white-eye blowout in a child - surgery must be performed within 48-72 hours, as there is a high risk of necrosis of the entrapped ocular muscle.
There is symptomatic enophthalmos of >2 mm (this can easily be measured in the eye clinic).
There is greater than 50% of the orbital floor involved.
Diplopia fails to resolve after 2-3 weeks.
Complications
Globe injury.
Persistent diplopia requiring delayed surgery.
Optic nerve damage.
Continue reading below
Medial orbital wall fracture
Features
These are rare in isolation but may accompany orbital floor fractures. They are characterised by subcutaneous emphysema, variable ecchymoses and medial rectus dysfunction (difficulty in rotating the eye towards the nose, associated with diplopia). There may also be enophthalmos or proptosis.
Management
Similar to orbital floor fractures (see above). Surgical repair is considered if there is significant pain or diplopia secondary to muscle entrapment.
Complications
As for orbital roof fractures (see below).
Orbital roof fracture
Isolated orbital roof fractures are rare and can be encountered by minor trauma - eg, falling on a sharp object (eg, umbrella tip) or a blow to the brow or the forehead. They are most common in young children. Complicated fractures involving major trauma are more common in adults.
Features
Haematoma of the upper lid and periocular ecchymoses which may spread to the other side over a few hours.
The globe may be inferiorly displaced and larger fractures may be associated with a pulsation of the globe.
Look for a superior subconjunctival haemorrhage with no distinct posterior limit.
Management
Although small fractures may be managed conservatively, the patient needs to be monitored closely for possible cerebrospinal fluid (CSF) leak. Larger fractures are usually managed surgically.
Complications
Meningitis can occur following a CSF leak.
Lateral orbital wall and zygomatic arch fracture
An isolated lateral wall fracture of the orbit is rare, as this is the strongest of the orbital walls. Lateral wall fractures are therefore more commonly seen following significant maxillofacial trauma involving the malar complex too. High-impact, blunt trauma to the cheek causes zygomatic fractures; they are easy to overlook and, if displaced, require treating within 10 days10 . Usually, a displaced fracture involves the orbitozygomatic complex6 :
The inferior orbital rim and orbital floor.
The zygomatico-frontal suture.
The zygomaticomaxillary buttress.
The zygomatic arch.
Occasionally, a direct blow can produce an isolated depressed fracture of the arch only.
Features
Suspect a malar fracture where there is10 :
Periorbital oedema.
Ecchymosis of the lower lid.
Lateral subconjunctival haemorrhage.
Even without a true orbital 'blowout' fracture, entrapment of orbital contents, enophthalmos, and diplopia with restriction of eye movement may occur because of the contributions of the zygomatic bone to the orbital floor. Periorbital and subconjunctival haemorrhage occur in around 50% of cases. Other features to note:
Fracture of the zygoma may or may not be painful to palpation and running a finger along the zygomatic arch may give a feel of a depressed fracture or a small dimple. The cheek may appear flattened: compare symmetry with the opposite side from behind the patient's head - this is most obvious immediately following trauma or several days later once swelling has subsided.
Posterior displacement of the fractured fragment may impair movement of the mandible, causing difficulty with chewing. Look for decreased range of mouth opening (normal should be >30 mm).
Forceful nose blowing can produce subcutaneous emphysema as shown by crepitation or proptosis and visual loss from orbital emphysema.
Management
A conservative approach is normal where there is no displacement of the fracture or minimal displacement without other complications.
Where a patient has multiple injuries or is severely unwell, surgery is often delayed. Damage to the globe takes precedence for repair.
Closed reduction techniques may be used but open reduction is often required12 .
If displacement is more than minimal or if other structures are involved, an open technique is used, possibly involving plates to stabilise bone. The precise approach will depend upon the injuries seen on the CT film and open surgical reconstruction may also have to be undertaken.
A multidisciplinary approach may be required in complex cases, using expertise from plastic surgery, facio-maxillary surgery, ear, nose and throat (ENT) and neurosurgery, depending upon other associated injuries.
A soft diet is usually required.
Attention should be payed to providing good analgesia. Antibiotics are normally prescribed with complex fractures and a short course of steroids may be used to reduce inflammation.
Careful follow-up is required to ascertain that there is good functional recovery, including the ability to eat and chew, eye position and normal facial anatomy.
Complications
Globe injury.
Injury to other orbital walls.
Failure to treat: risks cosmetic deformity or limited mandibular movement.
Prognosis
Good prognosis is suggested by:
Union of bones.
Lack of any deformity.
Full range of mandibular movement.
Prevention
Seat belts are important in reducing injuries in road traffic accidents13 . It is possible that seat belts appear to increase facial injuries because those who do not wear them suffer more severe injuries and die. A Brazilian study looking at the relationship between facial injuries and seat belt wearing suggested that14 :
The driver position shows the highest incidence of facial fractures and was not effectively protected against this by the use of a seat belt.
The wearing of seat belts seems to protect against facial fractures in front-seat passengers.
There was a high incidence of facial fractures among rear-seat passengers but it was not possible to evaluate the effect of seat belt use in this group.
Alcohol and binge-drinking are major contributory factors to assaults and facial injury. Many argue for harm-reduction measures such as the use, in licensed premises, of glasses and bottles made of plastic, controlling drink prices and targeted policing15 . Other measures include the introduction of minimum price per unit and modifying marketing and availability16 .
There is evidence that eye protection, mouth guards, helmets, and face guards help to reduce the risk of facial injury17 . Consider a fracture even if the person was not directly involved in the sport - a recent study found that 26% of maxillofacial fractures sustained by unmounted equestrians were caused by head-butts18 .
Further reading and references
- Ji SY, Kim SS, Kim MH, et al; Surgical Methods of Zygomaticomaxillary Complex Fracture. Arch Craniofac Surg. 2016 Dec;17(4):206-210. doi: 10.7181/acfs.2016.17.4.206. Epub 2016 Dec 23.
- Whittaker J; Zygomatic Complex and Nasal Injury, RCEM Learning, 2021
- Yamamoto K, Matsusue Y, Horita S, et al; Maxillofacial fractures of pedestrians injured in a motor vehicle accident. Craniomaxillofac Trauma Reconstr. 2013 Mar;6(1):37-42. doi: 10.1055/s-0033-1333881. Epub 2013 Jan 31.
- Adam AA, Zhi L, Bing LZ, et al; Evaluation of treatment of zygomatic bone and zygomatic arch fractures: a retrospective study of 10 years. J Maxillofac Oral Surg. 2012 Jun;11(2):171-6. doi: 10.1007/s12663-011-0294-x. Epub 2011 Dec 28.
- Arslan ED, Solakoglu AG, Komut E, et al; Assessment of maxillofacial trauma in emergency department. World J Emerg Surg. 2014 Jan 31;9(1):13. doi: 10.1186/1749-7922-9-13.
- Oppenheimer AJ, Monson LA, Buchman SR; Pediatric orbital fractures. Craniomaxillofac Trauma Reconstr. 2013 Mar;6(1):9-20. doi: 10.1055/s-0032-1332213. Epub 2013 Jan 16.
- Hwang K, You SH; Analysis of facial bone fractures: An 11-year study of 2,094 patients. Indian J Plast Surg. 2010 Jan;43(1):42-8.
- Ceallaigh PO, Ekanaykaee K, Beirne CJ, et al; Diagnosis and management of common maxillofacial injuries in the emergency department. Part 4: orbital floor and midface fractures. Emerg Med J. 2007 Apr;24(4):292-3.
- Yamamoto K, Matsusue Y, Horita S, et al; Clinical analysis of midfacial fractures. Mater Sociomed. 2014 Feb;26(1):21-5. doi: 10.5455/msm.2014.26.21-25. Epub 2014 Feb 20.
- Lubbers HT, Zweifel D, Gratz KW, et al; Classification of potential risk factors for trigeminocardiac reflex in craniomaxillofacial surgery. J Oral Maxillofac Surg. 2010 Jun;68(6):1317-21. Epub 2010 Mar 29.
- Ceallaigh PO, Ekanaykaee K, Beirne CJ, et al; Diagnosis and management of common maxillofacial injuries in the emergency department. Part 3: Orbitozygomatic complex and zygomatic arch fractures. Emerg Med J. 2007 Feb;24(2):120-2.
- Bergeron JM, Raggio BS; Zygomatic Arch Fracture
- Hwang K, Kim DH; Analysis of zygomatic fractures. J Craniofac Surg. 2011 Jul;22(4):1416-21. doi: 10.1097/SCS.0b013e31821cc28d.
- Fouda Mbarga N, Abubakari AR, Aminde LN, et al; Seatbelt use and risk of major injuries sustained by vehicle occupants during motor-vehicle crashes: a systematic review and meta-analysis of cohort studies. BMC Public Health. 2018 Dec 29;18(1):1413. doi: 10.1186/s12889-018-6280-1.
- Fonseca AS, Goldenberg D, Alonso N, et al; Seating position, seat belt wearing, and the consequences in facial fractures in car occupants. Clinics. 2007 Jun;62(3):289-94.
- Cusens B, Shepherd J; Prevention of alcohol-related assault and injury. Hosp Med. 2005 Jun;66(6):346-8.
- Alcohol-use disorders - preventing harmful drinking; NICE Public Health Guidance, June 2010
- Black AM, Patton DA, Eliason PH, et al; Prevention of Sport-related Facial Injuries. Clin Sports Med. 2017 Apr;36(2):257-278. doi: 10.1016/j.csm.2016.11.002. Epub 2017 Jan 11.
- Antoun JS, Steenberg LJ, Lee KH; Maxillofacial fractures sustained by unmounted equestrians. Br J Oral Maxillofac Surg. 2010 Apr 23.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Aug 2026
17 Aug 2021 | Latest version

Feeling unwell?
Assess your symptoms online for free