Diplopia and III, IV and VI cranial nerve lesions
Peer reviewed by Dr Pippa Vincent, MRCGPLast updated by Dr Rosalyn Adleman, MRCGPLast updated 11 Dec 2023
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Continue reading below
What is diplopia?
Diplopia is a common complaint in medical practice. It may be monocular or binocular. An understanding of the anatomy of the eye, external ocular muscles and their innervation is essential to approach diagnosis of the cause.
Binocular double vision (89%):1 this occurs when the images produced by the two eyes do not absolutely match, so that the images produced are misaligned relative to one another. The diplopia disappears when one eye is covered.
Monocular double vision: this is much less common. It affects one eye only and continues when the unaffected eye is covered. It can be caused by abnormalities of the lens, cornea or retina, which result in splitting of the image.
In one study 70% of the cases were isolated nerve palsies, of which the majority were isolated sixth nerve palsies, followed by fourth nerve palsies and then third nerve palsies. 29% were caused by vasculopathy (diabetes, hypertension, migraine); 25% by trauma; 12% by decompensating heterophorias; the remainder included inflammatory causes, tumours and thyroid eye disease.2
Problems with eye movements can occur in children, where diplopia is not necessarily seen. See the separate Strabismus (Squint) article, dealing with eye movements and squint.
Causes by anatomical site
Cornea and lens problems: problems affecting the cornea or lens, leading to production of unequal (or non-matching) images. These include refractive errors, keratoconus, cataracts, corneal scarring, subluxation and herpes zoster. Dryness of the cornea can occasionally cause double vision.
Eye muscle disorders: these include primary disorders of muscle such as myasthenia gravis, Graves' disease and myotonic dystrophy. Muscles (particularly the inferior rectus) may be trapped during basal orbital fracture. Convergence insufficiency (inability to align the eyes when focusing on near objects) is a common benign cause of intermittent binocular diplopia which is worse when tired. It can often be treated with glasses, eye exercises or prisms.
Nerve problems: problems affecting the cranial nerves III, IV and VI controlling the eye muscles. These include multiple sclerosis, Guillain-Barré syndrome and diabetes mellitus. Temporary palsy of a single ocular nerve is not uncommon, and may be of unknown cause. It can also be associated with some infections (eg, Lyme disease) and with inflammatory conditions such as giant cell arteritis. However, it is most commonly seen with vasculopathies such as diabetes mellitus and hypertension. Isolated VI nerve palsy has been reported in children after ear, nose and throat infections. Nerves can also be trapped following traumatic fracture of the orbital bones.
Brain problems: there are many possible causes of double vision inside the skull. These include vascular conditions such as strokes or aneurysms, space-occupying lesions in the orbit or skull (neoplastic or vascular), migraine or any cause of raised intracranial pressure. Raised intracranial pressure disproportionately affects the VI cranial nerve (abducens), as this has the longest intracranial course. Temporary diplopia may be caused by alcohol intoxication, or by head injuries such as concussion. It may be a side-effect of some drugs, including phenytoin, lamotrigine, zolpidem, opioids and ketamine.
Continue reading below
Anatomy of eye movements
There are six external ocular muscles - two are supplied by nerves unique to them: the superior oblique is supplied by the trochlear nerve (IV), and the lateral rectus is supplied by the abducens nerve (VI). The other four external muscles, the internal muscles and the eyelid are supplied by the oculomotor nerve (III).
The four rectus muscles pull directly on the globe so that they move the eye in the direction of their name: superior, inferior, medial and lateral. The superior and inferior recti are not placed centrally so they have a tendency to move the eye medially but this is opposed by the two oblique muscles.
Normal eye with muscles
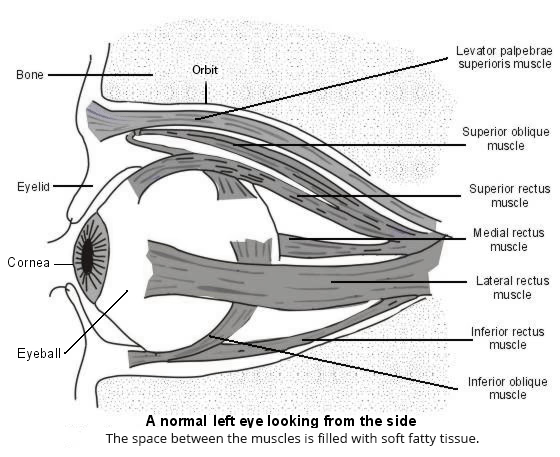
The oblique muscles move the eye outwards as well as up and down. Each hooks around a 'pulley' so that it moves the eye the opposite way to that which its name suggests. Hence, the superior oblique muscle moves the eye down and out (the tramp's muscle) and the inferior oblique muscle moves it up and out.
External Ocular Paralysis | |||
Muscle | Direction of pull | Result of paralysis | Cranial nerve |
Medial rectus | Medially | Lateral | III |
Superior rectus | Upwards | Downwards | III |
Lateral rectus | Laterally | Medial | VI |
Inferior rectus | Downwards | Upwards | III |
Superior oblique | Down and out | Up and in | IV |
Inferior oblique | Up and out | Down and in | III |
Presentation
Diplopia presents either with a complaint of double vision or the observation of squint. Paralysis of a muscle means that the eye will not move fully in the direction in which it pulls. At rest, when the other muscles are unopposed, the eye may therefore deviate in the opposite direction from the pull of the affected muscle.
Diplopia may occur alone or in conjunction with other symptoms such as pain on eye movement, pain around the eyes, ptosis, headache or nausea.
Continue reading below
Symptoms of diplopia
The patient will often complain of double vision. Images may overlap or be adjacent. It is helpful to ask about image alignment, whether they appear (or worsen) on particular direction of gaze, and whether they are intermittent or constant. It is also helpful to find out if the double vision disappears on closing one eye, and whether both images are in focus.
There may be associated symptoms such as ptosis, eye pain (with or without eye movement), headache and nausea.
Signs/examination
Check for ptosis, which is often the first sign of weakness. It suggests this is the affected side, as eyelid elevation is partly controlled by the oculomotor nerve (III).
Check the pupils and whether both are equal and react to light and accommodation. In Horner's syndrome, which also causes ptosis, the pupil on the affected side will be smaller because of reduced sympathetic tone. In Horner's syndrome there is loss of sweating and the finger may glide along the skin less easily.
Pupil abnormalities might otherwise signal that the cause lies inside the bony skull.
Visual acuity should be measured in each eye and may point to intraorbital problems, including retractive errors.
Fundoscopy should be performed to rule out papilloedema.
Check the other cranial nerves as described in the separate Neurological History and Examination article.
Attempt to identify which eye is affected and which direction of gaze is limited. This will allow determination of which structures are likely to be involved. Examine the alignment of the eyes in various head positions and on looking in every direction. Note whether one eye seems to be deviated. Isolated palsy of only one of the muscles supplied by the oculomotor nerve is unusual.
Hold the head still with one hand and hold up the index finger of the other hand about 40-50 cm from the eyes. Ask the patient to follow your finger to the left and the right and up and down, and to note when diplopia occurs.
If it is not clear that one eye is failing to move as far as the other, repeat the test but, instead of getting the patient to follow a finger, shine the light from a pen torch directly at their eyes. The light should be reflected in the centre of the pupil. When diplopia occurs the reflection will appear eccentric in the pupil on the affected side.
Children
In children, especially very small children, getting the child to follow a pen torch is much easier than asking the child to follow your finger and to report diplopia. The cover test may also be helpful. Ask the child to look at your face and then quickly cover one of their eyes. If there is a squint, the eye with the pathology will move to look directly at you only when the other is covered.3
Causes of diplopia
Determining the most likely cause of diplopia requires history and examination, with understanding of the anatomy. From the history and examination it should be possible to decide which muscle or muscles are affected, or whether the cause is within the globe. In primary disorders of muscle where fatiguability is the prime feature, examination may fail to show any abnormality.
Common causes
The intracranial course of the abducent nerve (VI) is long and so it is vulnerable at many sites. Hence, abducens nerve paralysis is important but it is a poor localising sign for a space-occupying lesion.
Isolated abducens nerve palsy is relatively common, occurring particularly in patients with vasculopathies such as diabetes.
Diplopia can be psychosomatic. This is suggested by inconsistency of history and unusual elements such as monocular double vision in both eyes, but it is nevertheless a diagnosis of exclusion. In particular, primary muscle disorders such as myasthenia gravis may cause 'inconsistent' diplopia.
Drug and alcohol intoxication may cause temporary diplopia. There will usually be other suggestive features.
Tiredness may cause abnormalities of eye muscle movement. Convergence insufficiency is more marked when a person is tired. Transient diplopia may occur with tiredness, particularly if reading glasses are needed but absent or inadequate. Diagnosis is usually on the history but it is important to exclude other causes of muscle fatiguability.
Between 40-50% of all patients with myasthenia gravis will present with ocular symptoms such as diplopia and 50-80% will progress to the full disease.4 This is, however, a condition of very low incidence. It may affect both eyes equally or unequally. Other rare conditions of muscle may also affect eye movements, including myotonic dystrophy.
Fluctuating weakness of external ocular muscles can occur in encephalopathy and sepsis. There will normally be confusion and other signs of severe illness.
Vertical gaze palsy is the inability to look up or down. It affects both eyes. Pupils are often unequal but fixed and there is usually no diplopia. Causes includeParkinson's disease and progressive supranuclear palsy. (Inability to look down can lead to falling down stairs.)
Multiple sclerosis (MS) often presents with optic neuritis in which there is pain on eye movement and alteration or loss of vision. Diplopia can occur.
Rare causes
Ophthalmoplegic migraine is a rare condition consisting of headaches accompanied by weakness of the external ocular muscles. The headaches are often followed by painful nerve palsy, usually of the oculomotor nerve (III), with accompanying Horner's syndrome. The condition may represent a variant of migraine, although clinical presentation and MRI findings have also suggested that it might be an inflammatory cranial neuropathy.
Giant cell arteritis (temporal arteritis), can present with diplopia. Visual symptoms are present in about a third of patients - amaurosis fugax and diplopia - and in about 30% of cases these effects are permanent.
Sarcoidosis can present with an isolated cranial nerve lesion. CXR may show bilateral hilar lymphadenopathy (BHL).
Diplopia may be a complication after refractive surgery.
Ocular lesions, including diplopia, can be amongst the presenting features of Creutzfeldt-Jakob disease (CJD), especially new variant CJD.5
Chronic progressive external ophthalmoplegia (CPEO) is a rare disorder of slowly progressive paralysis of the extraocular muscles.6 It is usually bilateral and symmetrical with progressive ptosis followed by external ocular paresis months to years later. Ciliary and iris muscles are spared.
Kearns-Sayre syndrome is a very rare mitochondrial myopathy related to CPEO but starting before the age of 20 and with pigmentary retinopathy.7
Five red flags
Pupil involvement with third nerve palsy: large poorly reactive pupil with diplopia is the most common presentation of an aneurysm of the posterior communicating artery.
Diplopia affecting two or more of lip, pupil and eye movement. This may suggest isolated third nerve palsy (as above), Horner's syndrome (small pupil and ptosis) due to carotid dissection, or inflammatory neuropathy (Guillain-Barré syndrome).
Multiple cranial nerve palsies: this suggests intracranial or meningeal tumour, polyneuropathy or cavernous sinus lesion.
Diplopia with weakness or fatigue: suggests myasthenia gravis.
Diplopia with new-onset headache and scalp tenderness: suggests giant cell arteritis.
Diagnosing diplopia
Diagnosing which muscles are affected is usually straightforward. A final diagnosis of the underlying cause is unlikely to be reached in primary care, so referral is usually required. Before referral, check for diabetes (if it is not already diagnosed) and check blood pressure in case of hypertension.
MRI scan may show a tumour, an area of infarction or even an arterial aneurysm pressing on a nerve. It can also show demyelination.
CXR may reveal malignancy or sarcoidosis.
Other specialist investigations may be offered depending on the suspected cause.
Isolated cranial nerve palsies in patients with diabetes and hypertension do not usually need investigation unless they progress or fail to resolve over time.
Multiple nerve palsies are usually imaged, as are isolated nerve palsies in patients aged under 50 years without a long history of vasculopathy.
Management of diplopia
Clinical management depends upon the cause.
In childhood strabismus, surgery may be required although this is not always the case. Treatment with botulinum toxin (which causes flaccid paralysis) is sometimes used. However, there is little clear evidence of its efficacy compared to surgical treatment, and complication rates (including ptosis and vertical deviation) can be high.8 9
Patients with unexplained binocular diplopia and those who progress or fail to recover within a few months should be investigated further to establish the aetiology.
Driving 10
People with diplopia must not drive. They may resume driving on confirmation to the licensing authority that the diplopia is controlled by glasses or by a patch which the licence holder undertakes to wear whilst driving. There will probably be permanent revocation of an LGV or PCV licence.
Exceptionally, a stable uncorrected diplopia of six months' duration or more may be compatible with driving if there is consultant support indicating satisfactory functional adaptation.
Prognosis
Prognosis is dependent on underlying cause. Most microvascular causes of diplopia resolve spontaneously within 6 months. 11 A VI nerve palsy of vascular cause typically resolves within 6-8 weeks. If resolution does not occur within months, the condition progresses or, if additional neurological signs or symptoms develop, imaging studies are required.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Alves M, Miranda A, Narciso MR, et al; Diplopia: a diagnostic challenge with common and rare etiologies. Am J Case Rep. 2015 Apr 13;16:220-3. doi: 10.12659/AJCR.893134.
- Kumar N, Kaur S, Raj S, et al; Causes and Outcomes of Patients Presenting with Diplopia: A Hospital-based Study. Neuroophthalmology. 2021 Mar 2;45(4):238-245. doi: 10.1080/01658107.2020.1860091. eCollection 2021.
- Helveston E, Moodley A; How to check eye alignment and movement. Community Eye Health. 2019;32(107):55. Epub 2019 Dec 17.
- Wang L, Zhang Y, He M; Clinical predictors for the prognosis of myasthenia gravis. BMC Neurol. 2017 Apr 19;17(1):77. doi: 10.1186/s12883-017-0857-7.
- Armstrong RA; Creutzfeldt-Jakob disease and vision. Clin Exp Optom. 2006 Jan;89(1):3-9.
- Murdock J, Thyparampil PJ, Yen MT; Late-Onset Development of Eyelid Ptosis in Chronic Progressive External Ophthalmoplegia: A 30-Year Follow-up. Neuroophthalmology. 2016 Feb 1;40(1):44-46. doi: 10.3109/01658107.2015.1122815. eCollection 2016 Feb.
- Shemesh A, Margolin E; Kearns Sayre Syndrome. StatPearls Publishing; 2019.
- Rowe FJ, Noonan CP; Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017 Mar 2;3:CD006499. doi: 10.1002/14651858.CD006499.pub4.
- Moorfields Eye Hospital: Botulinum Toxin Treatment for Squint in Children, August 2018
- Assessing fitness to drive, a guide for medical professionals; DVLA, September 2023
- Jain S; Diplopia: Diagnosis and management. Clin Med (Lond). 2022 Mar;22(2):104-106. doi: 10.7861/clinmed.2022-0045.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Dec 2028
11 Dec 2023 | Latest version

Feeling unwell?
Assess your symptoms online for free