Hysteroscopy
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Pippa Vincent, MRCGPLast updated 3 Aug 2023
Meets Patient’s editorial guidelines
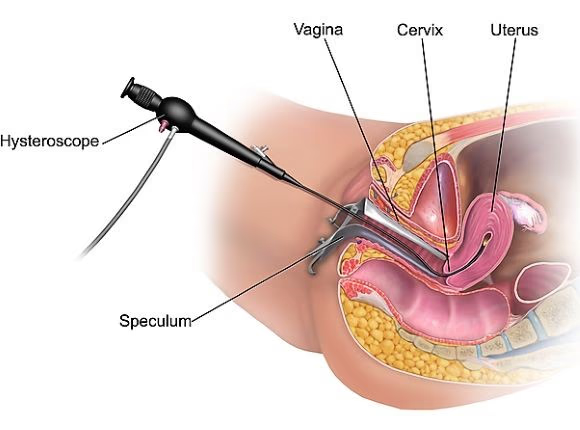
Hysteroscopy is a procedure which uses a thin tube-like telescope to see inside the womb (uterus). It can also allow doctors to do some minor operations to the uterus.
In this article:
Continue reading below
What is a hysteroscopy?
Hysteroscopy allows a doctor to look inside the womb (uterus). This is done using an instrument called a hysteroscope. The hysteroscope is very slim (about 3 to 5 millimetres in diameter). It's carefully passed through the vagina and neck of the womb (cervix) and into the uterus.
What happens during a hysteroscopy?
The hysteroscope is connected to a camera and a TV monitor which show the inside of the uterus. Some gas or fluid may be pumped into the uterus to make it swell a little. This makes it easier to see the lining of the uterus.
After this, the doctor may take a tiny piece of tissue (biopsy) from the uterus. This will be sent to the laboratory for examination under the microscope. Sometimes small fleshy lumps (polyps) are found. It may be possible to remove these during the test. After the procedure is completed the hysteroscope is gently removed.
A hysteroscopy takes between 5 and 30 minutes.
In some hospitals an ultrasound scan may be arranged before a hysteroscopy. See the separate leaflet called Ultrasound Scan for more details.
Continue reading below
What anaesthesia is used for hysteroscopy?
A hysteroscopy can be done under general or with local anaesthetic. A general anaesthetic means being put to sleep. Some women will not have either a general or a local anaesthetic. Occasionally, a sedative may be used, which won't cause sleep but may help to feel more relaxed.
A non-steroidal anti-inflammatory painkiller (for example, ibuprofen) might be advised around one hour before the appointment to help reduce pain immediately after the procedure. If no general anaesthetic is used, women may be asked if they wish to see the pictures coming from the hysteroscope. Some people do not wish to do this but others find it helpful.
The doctor may use a speculum (the same instrument used in a cervical screening test) so that they can see the neck of the womb. They then pass the hysteroscope through the cervix into the uterus. Sometimes the hysteroscope will be passed into the vagina without having to use a speculum.
Are there any preparations I should consider?
Local hospitals will give guidance on what to do before a hysteroscopy. If having a hysteroscopy with local anaesthetic, there will not usually be a need for any special preparation.
If having a general anaesthetic, it will be a requirement not to eat or drink for a number of hours before the procedure.
Hysteroscopy
By BruceBlaus (Own work) via Wikimedia Commons
Continue reading below
What can be found during a hysteroscopy?
A hysteroscopy may be used to find the cause of various problems such as:
Heavy or irregular bleeding that has not improved with medication.
Bleeding in between periods.
Bleeding after the menopause.
Irregular bleeding whilst taking hormone replacement therapy (HRT).
These are called diagnostic hysteroscopies.
As well as being used to investigate the cause of various problems, a hysteroscopy can also be used to:
Remove polyps - small lumps of tissue growing on the lining of the womb (uterus).
Remove scar tissue in the uterus.
Perform endometrial ablation - a procedure where the lining of the womb is made thinner in order to prevent heavy periods.
Remove adhesions (areas where the walls of the uterus are sticking together).
Locate a 'lost' or stuck contraceptive device, such as an intrauterine contraceptive device (IUCD) - also known as a 'coil'.
Perform certain types of sterilisation procedures.
Before having the procedure the gynaecologist will discuss the test. A number of different treatment options might be discussed. This is because it may be possible to treat the cause of symptoms immediately, using the hysteroscope. In order for this, agreement (consent) to the treatment will be needed in advance.
Is a hysteroscopy painful?
If awake, there may be a feeling like period cramps at some stages. A lot of women feel no discomfort or only minimal discomfort. For other women it is very painful and the procedure has to be stopped. In this case a hysteroscopy under general anaesthetic will be likely to be offered on another day. Many different things may influence how painful the procedure is. This includes:
Whether an anaesthetic is used.
Whether local or general anaesthetic is used and, if local, which type of local anaesthetic. (There are a number of options.)
Whether pain relief is used.
The size of hysteroscope used (the thinner ones tend to be less painful).
The type of hysteroscope used (flexible or rigid).
Whether a speculum is used.
The reason for having the test.
Whether babies have been delivered vaginally (vaginal delivery) in the past.
Whether the menopause has been reached/passed.
When asked to give consent to the procedure, these sorts of issues should be discussed. It is not possible to safely have a hysteroscopy whilst you are pregnant.
What can I expect after a hysteroscopy?
After a general anaesthetic or sedation, it is necessary to rest until the effects of these have passed. Driving is not permitted for the first 24 hours and it is usual to advise that a friend or relative should stay with the person for the first 24 hours.
After a local anaesthetic, it is usual to be able to go home as normal (walking, driving or travelling by public transport) after a short rest.
Period-like cramps and mild bleeding afterwards is common. The bleeding is usually mild and should settle within seven days. To reduce the risk of infection whilst bleeding it is best to:
Use sanitary towels rather than tampons.
Avoid vaginal sex for one week after the hysteroscopy and until the bleeding has stopped.
Take it easy for the first one or two days and take painkillers as needed.
Hysteroscopy side-effects
The most common side-effects after the procedure are bleeding and pain. Very rarely it is possible that a small hole may be made in the womb (uterus) by the hysteroscope. It is also possible, although not common, to develop an infection of the uterus as a result of hysteroscopy. Some women feel faint during the procedure, when the hysteroscope is passed through the cervix, but this is usually short-lived.
Medical advice should be sought if any problems develop, such as:
A temperature.
Increased unexplained pain not relieved with painkillers.
Increased discharge, which is smelly and unpleasant.
Heavy bleeding.
Further reading and references
- Tangsiriwatthana T, Sangkomkamhang US, Lumbiganon P, et al; Paracervical local anaesthesia for cervical dilatation and uterine intervention. Cochrane Database Syst Rev. 2013 Sep 30;9:CD005056. doi: 10.1002/14651858.CD005056.pub3.
- Ahmad G, Attarbashi S, O'Flynn H, et al; Pain relief in office gynaecology: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2011 Mar;155(1):3-13. doi: 10.1016/j.ejogrb.2010.11.018. Epub 2011 Jan 20.
- Centini G, Troia L, Lazzeri L, et al; Modern operative hysteroscopy. Minerva Ginecol. 2016 Apr;68(2):126-32. Epub 2016 Mar 1.
- Ahmad G, Saluja S, O'Flynn H, et al; Pain relief for outpatient hysteroscopy. Cochrane Database Syst Rev. 2017 Oct 5;(10)(10):CD007710. doi: 10.1002/14651858.CD007710.pub3.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 1 Aug 2028
3 Aug 2023 | Latest version

Feeling unwell?
Assess your symptoms online for free