Rheumatoid arthritis
Peer reviewed by Dr Krishna Vakharia, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 19 May 2023
Meets Patient’s editorial guidelines
In this series:Disease-modifying antirheumatic drugsBiological medicines for rheumatoid arthritisJuvenile idiopathic arthritis
Rheumatoid arthritis causes inflammation, pain, and swelling of joints. Persistent inflammation over time can damage affected joints.
The severity can vary from mild to severe. Treatments include disease-modifying medicines to suppress inflammation, which can prevent or delay the progression of the disease, and medication to ease pain.
The earlier treatment is started, the less joint damage is likely to occur. Surgery is needed in some cases if a joint becomes badly damaged.
In this article:
Continue reading below
What is rheumatoid arthritis?
Arthritis means inflammation of joints. Rheumatoid arthritis (RA) is a fairly common form of arthritis. (There are various other causes of arthritis and RA is just one cause.) About 1 in 100 people develop RA at some stage in their lives.
It can happen to anyone. It doesn't usually run in families. It can develop at any age, but most commonly starts between the ages of 30 and 50. It can occur in children and teenagers but this is very rare. See the separate leaflet called Juvenile Idiopathic Arthritis.
RA is about three times more common in women than in men.
Understanding joints
Normal joint
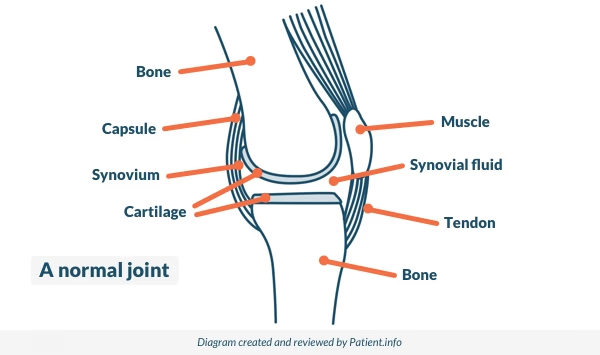
The place where two bones meet is called a joint. Joints allow movement and flexibility of various parts of the body. The movement of the bones is caused by muscles which pull on tendons that are attached to bone.
Cartilage covers the end of bones. Between the cartilage of two bones that form a joint there is a small amount of thick fluid called synovial fluid. This lubricates the joint, which allows smooth movement between the bones.
The synovium is the tissue that surrounds a joint. Synovial fluid is made by cells of the synovium. The outer part of the synovium is called the capsule. This is tough, gives the joint stability, and stops the bones from moving out of joint. Surrounding ligaments and muscles also help to give support and stability to joints.
What causes rheumatoid arthritis?
RA is thought to be an autoimmune disease - your own immune system, which usually fights off germs, accidentally attacks your body. It is not clear why this happens. Some people have a tendency to develop autoimmune diseases. In such people, something might trigger the immune system to attack the body's own tissues. The trigger is not known.
In people with rheumatoid arthritis, antibodies are formed against the tissue that surrounds each joint (the synovium). This causes inflammation in and around affected joints. Over time, the inflammation can damage the joint, the cartilage and parts of the bone near to the joint.
Continue reading below
Which joints are affected in rheumatoid arthritis?
The most commonly affected joints are the small joints of the fingers, thumbs, wrists, feet and ankles. However, any joint may be affected. The knees are quite commonly affected. Less commonly, the hips, shoulders, elbows and neck are involved.
It is often symmetrical. So, for example, if a joint is affected in a right arm, the same joint in the left arm is also often affected. In some people, just a few joints are affected. In others, many joints are involved.
Rheumatoid arthritis symptoms
Joint symptoms
The common main symptoms are pain and stiffness of affected joints. The stiffness is usually worse first thing in the morning, or after you have been resting. The inflammation causes swelling around the affected joints.
Other symptoms
These are known as extra-articular symptoms of RA (meaning outside of the joints). A variety of symptoms may occur. The cause of some of these is not fully understood:
Small painless lumps (nodules) develop in about 1 in 4 cases. These commonly occur on the skin over the elbows and forearms, but usually do no harm.
Inflammation around tendons may occur. This is because the tissue which covers tendons is similar to the synovium around the joints.
Anaemia and tiredness are common.
A high temperature (fever), feeling unwell, weight loss, and muscle aches and pains sometimes occur.
In a few cases, inflammation develops in other parts of the body, such as the lungs, heart, blood vessels, or eyes. This is uncommon but, if it occurs, can cause various symptoms and problems which are sometimes serious.
Continue reading below
How does rheumatoid arthritis develop and progress?
In most cases the symptoms develop gradually - over several weeks or so. Typically, you may first develop some stiffness in the hands, wrists, or soles of the feet in the morning, which eases by mid-day.
This may come and go for a while, but then becomes a regular occurence. You may then notice some pain and swelling in the same joints. More joints such as the knees may then become affected.
In a small number of cases, less common patterns are seen. For example:
In some cases pain and swelling develop quickly in many joints - over a few days.
Some people have bouts of symptoms which affect several joints. Each bout lasts a few days and then goes away. Several bouts may occur before persistent symptoms develop.
In some people, usually young women, the disease affects just one or two joints at first, often the knees.
The non-joint symptoms such as muscle pains, anaemia, weight loss, and high temperature (fever) are sometimes more obvious at first before joint symptoms develop.
The severity of RA can vary greatly from person to person. It is usually a chronic relapsing condition. Chronic means that it is persistent. Relapsing means that at times the disease flares up (relapses), and at other times it settles down. There is usually no apparent reason why the inflammation may flare up for a while, and then settle down.
If untreated, most people with RA have this pattern of flare-ups followed by better spells. In some people, months or even years may go by between flare-ups. Some damage may be done to affected joints during each flare-up.
The amount of disability which develops usually depends on how much damage is done over time to the affected joints. In a minority of cases the disease is constantly progressive, and severe joint damage and disability can develop quite quickly.
Joint damage
Inflammation can damage the cartilage which may become eroded or worn. The bone underneath may become thinned. The joint capsule and nearby ligaments and tissues around the joint may also become damaged.
Joint damage develops gradually, but the speed at which damage develops varies from person to person. Over time, joint damage can lead to deformities. It may become difficult to use the affected joints. For example, the fingers and wrists are commonly affected, so a good grip and other tasks using the hands may become difficult.
Most people with RA develop some damage to affected joints. The amount of damage can range from mild to severe. At the outset of the disease it is difficult to predict for an individual how badly the disease will progress. However, modern treatments can often limit or even stop the progression of the disease and limit the joint damage (see below).
How is rheumatoid arthritis diagnosed?
When you first develop joint pains, it may at first be difficult for a doctor to say that you definitely have RA. This is because there are many other causes of joint pains.
There is no single test which diagnoses early RA with 100% certainty. However, RA can usually be confidently diagnosed by a doctor, based on the following combination of factors:
Typical symptoms - as described above.
A blood test. The common test is to check for a protein in the blood, called rheumatoid factor. This is present in about 2 in 3 people with RA. However, about 1 in 20 of the normal population have rheumatoid factor. Also, some people with RA do not have rheumatoid factor, So, a positive rheumatoid factor is suggestive of RA, but not conclusive. A more recently developed test detects the presence of an antibody to a substance called cyclic citrullinated peptide (CCP) in a blood sample. This has been found to be more specific than rheumatoid factor in the diagnosis of RA. This blood test may become more commonly done to help diagnose RA.
X-rays of the hands or feet may be done. These may show the characteristic early damage to joints which is typical of RA.
You may also be advised to have a range of other blood tests to rule out other causes of joint pains.
Other associated diseases and possible complications
Associated conditions
The risk of developing certain other conditions is higher than average in people with rheumatoid arthritis. These include:
Cardiovascular disease (such as angina, heart attack and stroke).
Infections (joint infections and non-joint infections).
It is not clear why people with RA have a higher-than-average chance of developing these conditions. One possible reason is that, on average, people with RA tend to have more risk factors for developing some of these conditions. For example:
Lack of exercise and having high blood pressure are risk factors for developing cardiovascular diseases. People with RA may not be able to exercise very easily and some of the medicines used to treat RA may increase blood pressure.
Some of the medicines used to treat RA suppress the immune system. This may be a factor for the increased risk of developing infections.
Poor mobility and taking steroid medicines increase the risk of developing osteoporosis.
Other complications
Other complications which may develop include:
Carpal tunnel syndrome. This is relatively common. It causes pressure on the main nerve going into the hand. This can cause pain, tingling and numbness in parts of the hand. See the separate leaflet called Carpal Tunnel Syndrome for details.
Tendon rupture sometimes occurs (particularly the tendons on the back of the fingers).
Pressure on the spinal cord in the neck (cervical myelopathy). This is an uncommon but serious complication of severe, long-standing RA. It is caused by a dislocation of joints at the top of the spine.
The importance of early diagnosis and treatment
If your doctor suspects that you have RA, you will usually be referred to a joint specialist (a rheumatologist). This is to confirm the diagnosis and to advise on treatment.
It is very important to start treatment as early as possible after symptoms begin. This is because any joint damage done by the disease is permanent. Therefore, it is vital to start treatment as early as possible to minimise or even prevent any permanent joint damage.
Rheumatoid arthritis treatment
Standards of care you should expect
The National Institute for Health and Care Excellence (NICE) has published quality standards on the standard of care that should be offered to every adult over 16 who has RA. They state:
If you have symptoms suggestive of RA, you should be referred by your GP to a hospital specialist within three working days.
If you have active RA, you should be started on disease-modifying treatment within six weeks of being referred, and monitored every month until your treatment target is met.
You should be given regular opportunity to take part in activities which help you manage your condition.
If your symptoms flare or you have side-effects related to your treatment, you should be able to access advice from your specialist within one working day.
Your specialist should arrange and co-ordinate a yearly review of your condition.
There is no cure for rheumatoid arthritis. However, treatments can make a big difference to reduce symptoms and improve the outlook (prognosis). The main aims of treatment are:
To decrease the disease activity as much as possible so as to prevent joint damage as much as possible.
To reduce pain and stiffness in affected joints as much as possible.
To minimise any disability caused by pain, joint damage, or deformity.
To treat other symptoms of the disease if they develop.
To reduce the risk of developing associated conditions such as cardiovascular disease or 'thinning' of the bones (osteoporosis).
Treatment aim 1 - to decrease disease activity and prevent joint damage
Disease-modifying medicines
There are a number of medicines called disease-modifying antirheumatic drugs (DMARDs). See the separate leaflet called Disease-modifying Antirheumatic Drugs (DMARDs). These are medicines that ease symptoms but also reduce the damaging effect of the disease on the joints.
They work by blocking the way inflammation develops in the joints. They do this by blocking certain chemicals involved in the inflammation process. DMARDs include methotrexate, sulfasalazine, leflunomide and hydroxychloroquine. It is these medicines that have improved the outlook in recent years for many people with RA.
It is usual to start a DMARD as soon as possible after RA has been diagnosed. It is also common practice to use a combination of two or more DMARDs. This is commonly methotrexate plus at least one other DMARD. In general, the earlier you start DMARDs, the more effective they are likely to be.
DMARDs have no immediate effect on pains or inflammation. It can take several weeks, and sometimes several months, before you notice any effect. Therefore, it is important to keep taking DMARDs as prescribed, even if they do not seem to be working at first.
Whilst on treatment, you are likely to have a blood test called a C-reactive protein (CRP) test every now and then. This test detects inflammation in the body. As the disease activity reduces, so should the blood level of CRP.
The CRP test, in conjunction with assessing your symptoms, is a good way of monitoring disease activity and the effect of treatment in controlling the disease. If DMARDs work well, it is usual to take one or more DMARDs indefinitely. However, when a satisfactory level of disease control has been achieved, your doctor may advise a cautious reduction in doses, but not to a dose less than that required to continue to maintain disease control.
Each DMARD has different possible side-effects. If one does not suit, a different one may be fine. Some people try several DMARDs before one or more can be found to suit. Some side-effects can be serious. These are rare and include damage to the liver and blood-producing cells. Therefore, it is usual to have regular tests - usually blood tests - whilst you take DMARDs. The tests look for some possible side-effects before they become serious.
Biological medicines
Biological medicines have been introduced more recently and also have a disease-modifying effect against RA. See the separate leaflet called Biological Medicines for Rheumatoid Arthritis.
Treatment with a tumour necrosis factor (TNF) alpha inhibitor (adalimumab, certolizumab pegol, etanercept, golimumab, or infliximab), other biological DMARD (abatacept, sarilumab, or tocilizumab), or targeted synthetic DMARD (baricitinib, filgotinib, tofacitinib, or upadacitinib) is recommended if there has been an inadequate response to combination therapy with conventional DMARDs (as above).
They are called biological medicines because they mimic substances produced by the human body such as antibodies. Also, they are made by living organisms such as cloned human white blood cells. This is unlike most medicines that are made by chemical processes.
Biological medicines work in RA by blocking chemicals that are involved in inflammation. For example, some of these biological medicines block a chemical called TNF-alpha which plays an important role in causing inflammation in joints in RA.
One problem with biological medicines is that they need to be given by injection. They are also expensive. Guidelines state that two trials of six months of traditional DMARD treatments (at least one including methotrexate) should fail to control symptoms or prevent disease progression before one of these newer biological medicines may be recommended. Biological medicines may also be used in combination with methotrexate (a DMARD).
Maintaining good oral hygiene may help
There seems to be an association between gum disease and the activity of RA. (Gum disease is very common.) One recent research trial looked at 40 people with RA who also had gum disease.
The trial compared 20 people who had treatment for their gum disease with 20 people who did not. It found that the disease activity of RA seemed to decrease when gum disease was treated. The treatment for the gum disease was scaling/root planing and oral hygiene instructions. That is, basically, good dental care and oral hygiene such as tooth brushing and flossing.
Gum disease causes an ongoing inflammation in the gums. The theory is that this inflammation may in some way add to the immune mechanisms involved in the inflammation of RA.
Further research is needed to confirm this association. But, in the meantime, it seems sensible to make sure your oral hygiene is good, as it may have a beneficial effect. See the separate leaflet called Dental Plaque and Gum Disease for details.
Treatment aim 2 - to reduce pain and stiffness
DMARDs and biological medicines mentioned earlier control the activity of the disease and will ease symptoms when they take effect. However, whilst waiting for them to take effect, or if they do not work so well, you may need treatment to treat symptoms.
During a flare-up of inflammation, if you rest the affected joint(s) it helps to ease pain. Special wrist splints, footwear, gentle massage, or applying heat may also help. Medication is also helpful.
Medicines which may be advised by your doctor to ease pain and stiffness include the following:
Non-steroidal anti-inflammatory drugs (NSAIDs)
These are sometimes just called anti-inflammatories and are good at easing pain and stiffness, and also help to reduce inflammation.However they should be used at the lowest effective dose for the shortest time in order to reduce the risk of side effects.
There are many types and brands. Each is slightly different to the others, and side-effects may vary between brands. To decide on the right brand to use, a doctor has to balance how powerful the effect is against possible side-effects and other factors. Usually one can be found to suit. However, it is not unusual to try two or more brands before finding one that suits you best.
The leaflet which comes with the tablets gives a full list of possible side-effects. The most common side-effect is stomach pain (dyspepsia). An uncommon but serious side-effect is bleeding from the stomach. Therefore, your doctor will usually prescribe another medicine to protect the stomach from these possible problems. Stop taking the tablets and see a doctor urgently if you:
Develop stomach (abdominal) pains.
Pass blood or black stools (faeces).
Bring up (vomit) blood whilst taking an anti-inflammatory.
After starting a DMARD (discussed earlier), many people take an anti-inflammatory tablet for several weeks until the DMARD starts to work. Once a DMARD is found to help, the dose of the anti-inflammatory tablet can be reduced or even stopped.
Painkillers
Paracetamol often helps. This does not have any anti-inflammatory action, but can be useful for pain relief if you are unable to take an anti-inflammatory tablet. Codeine is another stronger painkiller that is sometimes used.
Note: NSAIDs and painkillers ease the symptoms of RA. However, they do not alter the progression of the disease or prevent joint damage. You do not need to take them if symptoms settle with the use of disease-modifying medicines.
Steroids
Steroids are good at reducing inflammation. It is common practice to advise a short course of steroids to damp down a flare-up of symptoms which has not been helped much by an NSAID. Also, when RA is first diagnosed, a short course of steroids is commonly used to control symptoms whilst waiting for DMARDs to take effect.
Sometimes a steroid is used for a longer period of time but only if other treatments (DMARDs and biological medicines) have been tried and either not fully effective or not tolerated because of side effects.
An injection of steroid directly into a joint is sometimes used to treat a bad flare-up in one particular joint.
The main side-effects from steroids occur when they are used for more than a few weeks. The higher the dose, the more likely that side-effects become a problem. Serious side-effects that may occur if you take steroids for more than a few weeks, or if you have injections frequently, include:
Thinning of the skin.
Weight gain.
Muscle wasting.
Increased risk of serious infection.
Treatment aim 3 - to minimise disability as much as possible
As far as possible, try to keep active. The muscles around the joints will become weak if they are not used. Regular exercise may also help to reduce pain and improve joint function. Swimming is a good way to exercise many muscles without straining joints too much. A physiotherapist can advise on exercises to keep muscles around joints as mobile and strong as possible. They may also advise on splints to help rest a joint if needed.
If such things as your grip or mobility become poor, an occupational therapist may advise on adaptations to the home to make daily tasks easier.
If you develop a joint deformity then surgery to correct it may be an option. If severe damage occurs to a joint, operations such as knee or hip replacements are an option.
Treatment aim 4 - to treat any other symptoms of the disease
As mentioned earlier, sometimes people with RA develop inflammation in other parts of the body such as the lungs, heart, blood vessels, or eyes. Also, anaemia may develop. Various treatments may be needed to treat these problems if they occur.
Treatment aim 5 - to reduce the risk of developing other diseases
As mentioned earlier, if you have RA you have an increased risk of developing cardiovascular diseases (for example, angina, heart attack, and stroke), osteoporosis and infections. Therefore, you should consider doing what you can to reduce the risk of these conditions by other means.
For example, if possible:
Do not smoke. (In addition to increasing the risk of cancer, heart disease and stroke, smoking may also make symptoms of RA worse.)
If you have high blood pressure, diabetes, or a high cholesterol level, they should be well controlled on treatment.
See the separate leaflets called Cardiovascular Disease (Atheroma) and Osteoporosis for more details.
Immunisations
To prevent certain infections, you should have:
An annual flu jab if you are over the age of 65 years, or are taking immunosuppressive medicines, or are taking steroids equivalent to 20 mg or more of prednisolone each day for more than a month.
A one-off pneumococcal immunisation if you are over the age of 65 years, or are taking immunosuppressive medicines, or are taking steroids equivalent to 20 mg or more of prednisolone each day for more than a month.
Other treatments
Some people try complementary therapies such as special diets, bracelets, acupuncture, etc. There is little research evidence to say how effective such treatments are for RA. In particular, beware of paying a lot of money to people who make extravagant claims of success. For advice on the value of any treatment it is best to consult a doctor.
What is the outlook for rheumatoid arthritis?
The outlook (prognosis) regarding joint damage has become much better with improved treatments, particularly the early use of DMARDs and biological medicines.
Another factor to bear in mind is the increased risk of developing associated diseases such as cardiovascular disease (see above). Because of this, the average life expectancy of people with RA is a little reduced compared with the general population. This is why it is important to tackle any factors that you can modify, such as smoking, diet, weight, etc.
Further reading and references
- 2016 update of the EULAR recommendations for the management of early arthritis; European League against Rheumatism (2017)
- EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs, 2016 update; EULAR (Mar 2017)
- Rheumatoid arthritis in adults: management; NICE Guideline (July 2018 - last updated October 2020)
- Management of rheumatoid arthritis in over 16s; NICE Quality Standard, 2013 - last updated January 2020
- Rheumatoid arthritis; NICE CKS, April 2020 (UK access only)
- Smolen JS, Landewe RBM, Bijlsma JWJ, et al; EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020 Jun;79(6):685-699. doi: 10.1136/annrheumdis-2019-216655. Epub 2020 Jan 22.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 12 May 2028
19 May 2023 | Latest version

Feeling unwell?
Assess your symptoms online for free