Blepharitis
Peer reviewed by Dr Rachel Hudson, MRCGPLast updated by Dr Caroline Wiggins, MRCGP Last updated 20 Jul 2023
Meets Patient’s editorial guidelines
Blepharitis means inflammation of the eyelids. It causes the eyes to feel irritated and the eyelids may be puffy and red. It can be a troublesome and recurring condition with no one-off cure. However, once symptoms have improved, daily eyelid hygiene can usually keep symptoms to a minimum. Eyesight is rarely affected.
In this article:
Continue reading below
What is blepharitis?
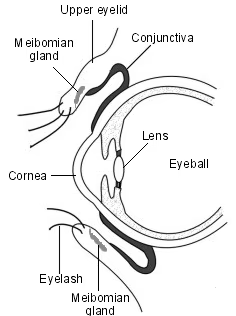
Eye with eyelid detail
Blepharitis is an inflammation reaction. The inflammation can be caused by infection, allergies or skin conditions. It usually affects the lid margins (edges of eyelids). Blepharitis is not usually serious but it may become an uncomfortable, irritating problem.
Blepharitis is typically persistent (chronic) and affects both eyes.
Patient picks for Eyelid problems
Blepharitis symptoms
The main symptom of blepharitis is sore eyelids. Both eyes are usually affected.
The eyes may feel gritty, itchy or as though they are burning.
The eyelids may look inflamed or greasy.
The eyes may become sticky with discharge. This is usually worse in the morning.
Sometimes tiny flakes or scales appear on the eyelids, which look like small flakes of dandruff. Crusts may develop at the base of your eyelashes.
One or more of the tiny glands of the eyelids (meibomian glands) may block and fill with fluid.
Blepharitis

By clubtable, Public domain, via Wikimedia Commons
Symptoms often come and go. Typically, symptoms flare up from time to time; however, you may have long periods without any symptoms.
Other conditions which affect the eyes, or skin around the eyes, are commonly associated with blepharitis. They are:
Dry eye syndrome (keratoconjunctivitis sicca).
Seborrhoeic dermatitis.
Rosacea.
See the separate leaflets called Seborrhoeic Dermatitis, Dry Eyes and Rosacea for further information.
Continue reading below
Blepharitis causes
There are three main types of blepharitis:
Staphylococcal blepharitis.
Seborrhoeic blepharitis.
Meibomian blepharitis.
All three types of blepharitis can cause similar symptoms.
Staphylococcal blepharitis
This type of blepharitis is thought to be caused by a germ (bacterium) called staphylococcus. This bacterium is all around us in our environment, and typically lives in low numbers on our skin.
Most often it does so without doing any harm; however, occasionally it can cause skin infections such as impetigo and inflamed acne. In some people this bacterium affects the skin at the edge of the eyelids, causing blepharitis.
Seborrhoeic blepharitis
Seborrhoeic blepharitis is closely associated with a skin condition called seborrhoeic dermatitis. In seborrhoeic dermatitis, the skin tends to be oily and can become scaly. It typically causes bad dandruff and sometimes a rash, commonly on the face and upper body.
The underlying cause of seborrhoeic dermatitis is not clear. A type of yeast called Malassezia furfur is thought to be involved in triggering the condition in some people.
This type of blepharitis may be a reaction to the yeast, which lives in the oil (sebum) of human skin in most adults and which usually does no harm. Seborrhoeic dermatitis is not contagious - it is the reaction to the yeast which seems to cause the condition, rather than the yeast itself.
Meibomian blepharitis
This is also known as meibomian gland dysfunction. The meibomian glands in the eyelids lie just behind the eyelashes. There are about 25-30 meibomian glands on each upper and lower eyelid. They make a small amount of oily fluid which comes out on the inside of the eyelids next to the eye. This oily fluid forms the outer layer of the tear film which lubricates the front of the eye.
People with meibomian blepharitis may have problems with the meibomian glands or the fluid they produce. People with meibomian blepharitis often have dry eyes, as the fluid they make may not have quite the right balance of oils needed to lubricate the eye.
Combinations of the above
In practice, it is often not possible to tell the difference between the different causes of blepharitis, and commonly more than one is present at the same time.
Complications of blepharitis
In most cases, blepharitis is uncomfortable but not serious or sight-threatening. Complications are uncommon. They include:
Chalazion (meibomian cyst). This is a painless swelling, most prominent on the inside of the eyelid. It is due to a blocked meibomian gland. Although it is painless, it may make the eyelid bulge and look a little unsightly. It can easily be treated. Sometimes a chalazion can become infected and painful. See the separate leaflet called Chalazion for further information.
Stye. This is a painful infected swelling most prominent on the outside of the eyelid. It is due to an infection of the root (follicle) of an eyelash. See the separate leaflet called Stye for more information.
Contact lens wearers may find that their lenses feel uncomfortable when they have a flare-up of blepharitis.
Changes to the eyelashes can occur in long-standing cases. These include:
Loss of eyelashes (madarosis).
Misdirection of eyelashes towards the eye (trichiasis).
Loss of the colour of the eyelashes (poliosis).
Inflammation of the front of the eye (conjunctivitis). This may cause a sore, red eye with discharge or watering. See the separate leaflet called Infective Conjunctivitis for more information.
Conjunctival phlyctenules. These are tiny (1-3 mm), hard, yellowish-white lumps (nodules) surrounded by tiny blood vessels. They tend to occur on the lower part of the eye just below the transparent front part of the eye (the cornea). They are clumps of white blood cells that are responding to the presence of germs (bacteria).
Inflammation of the cornea (keratitis). This complication is rare but serious as it can affect sight. See a doctor urgently if you develop eye pain (more than the irritation/grittiness of dry eye) or any loss of vision from the affected eye.
Eyelid ulceration (and later scarring) occur rarely. This can cause the eyelid to turn inwards against the eyeball (entropion) or outwards (ectropion). See the separate leaflet called Ectropion.
Continue reading below
Diagnosing blepharitis
There is no specific test for blepharitis but your doctor or optician may suspect it if you have many of the symptoms above.
Blepharitis treatment
Unfortunately there is no one-off cure for blepharitis as the inflammation tends to recur if you do not keep up with treatment.
The aim of treatment is to control or manage blepharitis. this can ease symptoms and reduce the frequency of flare-ups. Most of the treatment is done by you, rather than having prescriptions or treatments from your doctor or optician. The main treatment for blepharitis is regular eyelid hygiene (see below). Other treatment options that may be needed include antibiotics and artificial tear drops.
Regular eyelid hygiene
This is the most important part to treat and prevent blepharitis. The aim is to soothe the eyelids, unplug any blocked meibomian glands and clear out secretions from these glands. The eyelids are cleaned and debris is removed.
You should do the below routine - warmth, massage, clean - at least twice a day until symptoms settle. When the symptoms have eased, keep doing this routine once a day, every day, to prevent further flare-ups. If you are prone to blepharitis it is best to think of this as part of your daily routine - just like brushing your teeth. This is the best way to keep symptoms away, or to a minimum.
It is important to wash your hands before and after performing eyelid hygiene and use a freshly cleaned pad, flannel or new cotton bud each time. This is to reduce the chance of introducing an infection to the area. Remove your contact lenses for this routine.
Warmth
The purpose of warmth is to soften the skin and any crusts attached to the eyelids. It also makes the oily secretions made by the meibomian glands flow more freely. Therefore, warmth helps to unplug any blocked glands and allow the oily secretions to flow more readily. Warmth applied to the eyelids for five to ten minutes is sufficient to do this.
The traditional method is to soak a flannel in very warm water and gently place it against your eyelids for 5-10 minutes. The flannel usually cools quickly, when it does keep re-warming it in the warm water.
A popular alternative is to use a specially designed reusable heat bag which you place over your eyes for about five minutes. There are a number of such bags available, which you can buy from some opticians or online.
The advantage of a heat bag over a hot flannel is that the heat is retained for longer, keeping a constant warmth over the eyes. You can simply lie down and relax for five to ten minutes with the bag placed over your eyes.
Massage
Massaging helps to push out the oily fluid from the tiny meibomian glands. To massage the eyelids:
Massage immediately after applying warmth.
Massage along the length of the upper and lower eyelids towards the eye. That is, sweeping downwards when moving along the upper eyelid, and upwards when moving along the lower eyelid. The idea is that you are moving the oily secretions towards the edge of the eyelid so that they can come out of the glands.
Repeat this massage action 5 to 10 times over about 30 seconds.
Massaging should neither to be too gentle nor too firm. It should be relatively comfortable and you should not press hard enough to actually hurt your eyeball under the closed eyelids.
Always massage with the eyes shut.
Clean
After warmth and massage, clean your eyelids. Research suggests that all of the following methods were effective and could not identify which was the best. Most people preferred to use the cleansing fluid. This was thought to be because it was easy to use and convenient. You can use a cotton pad, cotton wool ball, clean finger or cotton bud with any of the following options:
Eyelid cleansing fluid that you can buy at some opticians/optometrists.
Cooled water that has recently been boiled (or preserved water for people who wear contact lenses).
Diluted baby shampoo.
Artificial tear drops
Blepharitis is often associated with dry eyes. This is because the tear film is produced by the meibomian glands. So if they are blocked or not working well, your eyes will not be as well lubricated. Therefore, artificial tear drops may help ease symptoms. These come as eye drops and gels. You can buy them at pharmacies or get them on prescription. Preservative-free eyedrops should be used if you use them more than four times daily.
Antibiotic treatments
If your blepharitis doesn't respond to regular cleaning, you may be prescribed a course of antibiotic ointments, creams or eye drops (topical antibiotics).
Antibiotic eye ointment or drops should be rubbed very gently along the edge of the eyelid (not the eye) after cleaning the eyelid in the way described above. Apply them with clean fingers or a cotton bud. They are usually used several times a day to start with, and eventually once a day, for about six weeks.
You should stop wearing contact lenses when using antibiotic eye drops, as they can affect the lenses, which can also trap drops behind them which can irritate your eye. If using more than one type of eye drop, leave at least five minutes between applying them.
Oral antibiotics (tablets), taken once or twice a day, are occasionally prescribed if other treatments fail. You will normally be advised to use these for three months, and sometimes for longer.
Doxycycline is most often used, although this antibiotic can cause a rash in some people if they are exposed to the sun, and it's also advisable to avoid sunbeds if taking it. Doxycycline and some similar antibiotics should not be taken if you are pregnant or breastfeeding, and is avoided in children aged under 12 years.
Steroid eye drops
These may be used to reduce inflammation where other treatments have failed. If you may require these you will usually be referred to a specialist.
Intense pulsed light
This is a new treatment. A review of the studies which treated people with this treatment have not shown it to be effective or safe. More research is needed on this treatment.
Tips and home remedies for blepharitis
Wearing eye make-up, particularly eyeliner and mascara, may make blepharitis symptoms worse. It is best for avoid these. It's also sensible to discard any liquid eye make-up you were using when the condition developed.
Rubbing the eyelids will often make inflammation worse..
One study suggested that omega-3 oils, found in oily fish, may improve symptoms for some people with dry eye syndrome and blepharitis but another study did not find any benefit. Omega-3 supplements can be purchased in health food shops.
Rather than taking the oil, you could increase your consumption of oily fish (although if you are pregnant, or trying to become pregnant, you should not eat more than two portions of oily fish per week. This is because it may contain substances such as mercury which can be harmful to your unborn baby).
If you also have seborrhoeic dermatitis, rosacea or dry eye syndrome, treating these conditions will also help to ease symptoms of blepharitis.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Lindsley K, Matsumura S, Hatef E, et al; Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012 May 16;5:CD005556. doi: 10.1002/14651858.CD005556.pub2.
- Blepharitis Preferred Practice Patterns; American Academy of Ophthalmology, 2018 - links to downloadable pdf file
- Blepharitis; NICE CKS, April 2023 (UK access only)
- Blepharitis guideline, The College of Optometrists. Published 06/07/2022
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 18 Jul 2028
20 Jul 2023 | Latest version
Last updated by
Dr Caroline Wiggins, MRCGP
Peer reviewed by
Dr Rachel Hudson, MRCGP

Feeling unwell?
Assess your symptoms online for free
