Juvenile idiopathic arthritis
Peer reviewed by Dr John Cox, MRCGPLast updated by Dr Mary Harding, MRCGPLast updated 22 Nov 2018
Meets Patient’s editorial guidelines
In this series:Rheumatoid arthritisDisease-modifying antirheumatic drugsBiological medicines for rheumatoid arthritis
This page has been archived.
It has not been reviewed recently and is not up to date. External links and references may no longer work.
Juvenile idiopathic arthritis is a condition in which persisting joint inflammation first occurs in children under the age of 16 years. Affected joints become painful and swollen, and can become damaged. Juvenile idiopathic arthritis cannot generally be cured but there are effective treatments. These help symptoms, prevent any long-standing joint problems, and can lead to remission.
In this article:
Continue reading below
What is juvenile idiopathic arthritis?
Juvenile means it affects young people. Idiopathic means the cause is not known. Arthritis means inflammation of one or more joints. The main symptoms of arthritis are pain and stiffness of affected joints. The stiffness is usually worse first thing in the morning, or after resting. The inflammation causes swelling around the affected joints.
So, juvenile idiopathic arthritis (JIA) is a condition in which this inflammation of one or more joints begins in children under the age of 16 years. It lasts for at least six weeks. In most people who get JIA, it is a long-term illness. It can be treated, but not usually cured - in other words, symptoms can be relieved, and joint damage can be prevented, but symptoms may return in future.
There are seven different types of JIA:
Oligoarticular JIA
This type accounts for at least half of all cases of JIA in Europe and the USA. Arthritis affects between 1 and 4 joints during the first six months after the arthritis begins. One of the blood tests taken may show a positive result for antinuclear antibodies. Antinuclear antibodies are a type of protein in the blood, called auto-antibodies. These proteins occur in people with some conditions and can be measured in the blood. See the separate leaflet called Antibody and Antigen Tests for more details.
If more than six joints are affected after six months, it is called extended oligoarthritis. If no more than four joints are affected after six months then it is called persistent oligoarthritis.
Polyarticular JIA - rheumatoid factor negative
This type accounts for another quarter of all cases of JIA. Arthritis affects five or more joints in the first six months. A blood test for a chemical called rheumatoid factor (RF) in the blood is negative.
Polyarticular JIA - RF positive
Arthritis affects five or more joints in the first six months. A blood test for RF in the blood is positive. This is the type in about 5 in 100 cases of JIA.
Systemic-onset JIA
This is the type in 5-10 out of every 100 cases of JIA. Arthritis develops with at least two weeks of daily high temperature (fever). The fever must be greater than 39ºC and return to less than 37ºC between the episodes of fever. There must be one or more of:
A rash which quickly fades and changes.
Increased size of lymph glands (nodes).
Increased size of the liver and/or spleen.
Inflammation of the lining of the heart (pericarditis), lungs (pleuritis) or the abdomen (peritonitis).
Juvenile psoriatic arthritis
This type is involved in 2-15 out of every 100 cases of JIA. Arthritis occurs with a skin condition called psoriasis or there is arthritis plus at least two of:
Inflammation of a finger or toe, causing pain and swelling.
Abnormality of one or more fingernails.
Psoriasis in a close relative.
Enthesitis-related arthritis
This is the type in 2-10 out of every 100 cases of JIA. Arthritis occurs with inflammation at the site of attachment of a tendon or ligament to a bone (called enthesitis), plus any two of:
Pain in the joints of the lower back (lumbosacral spine) and/or the pelvis (sacroiliac joints).
A blood test for a chemical marker of certain diseases - called HLA B27 - is positive in 90% of people who have enthesitis-related JIA.
A family history of illnesses associated with being HLA B27-positive, including ankylosing spondylitis, inflammation affecting the eye (uveitis), psoriatic arthritis and ulcerative colitis.
The child affected with enthesitis-related arthritis also has other illnesses associated with being positive for HLA B27.
The arthritis affects a boy and starts when the boy is over the age of 6 years.
Undifferentiated arthritis
Undifferentiated JIA is used to describe arthritis that doesn't fit into any of the other different groups of JIA. About 1-10 of every 100 cases fit into this category.
How common is juvenile idiopathic arthritis?
Juvenile idiopathic arthritis (JIA) is uncommon. Between 1 and 2 in every 1,000 children are affected at any one time. Between 1 and 2 in every 10,000 children develop JIA each year.
How common each type is varies in different parts of the world. For example, in the UK, oligoarticular JIA is the most common type. Polyarticular JIA is more common in countries such as India, New Zealand and South Africa. Systemic arthritis is more common in Asia than it is in Europe.
Continue reading below
Juvenile idiopathic arthritis symptoms
The main symptom of juvenile idiopathic arthritis (JIA) is pain and swelling of several joints (arthritis). Sometimes, other symptoms outside of joints (known as extra-articular symptoms) may also be present. These include conditions causing eye inflammation (uveitis) and inflammation of the lining of the heart (pericarditis), lungs (pleuritis) or abdomen (peritonitis). JIA may also in some cases be associated with high temperature (fever) or symptoms of anaemia (such as feeling tired all the time).
In very young children, it may be harder to know they have joint pain. They may cry more than usual or wake up crying. They may have delayed crawling or walking, or may become less mobile than they were before. They may lose weight or be just generally miserable and not right. You may notice that joints are hot or swollen or red. Older children may be able to describe the stiffness or pain they have in one or more joints.
The symptoms are slightly different depending on the type of JIA:
Oligoarticular JIA symptoms
This usually presents in children under 6 years old and is more common in girls. It often starts with one or two swollen joints causing stiffness and reduced movement but often not much pain. The knees and ankles are most often affected.
Polyarticular JIA (RF negative) symptoms
This most often presents in preschool children and in children aged 10-13 years. It is more common in girls.
Polyarticular JIA (RF positive) symptoms
This affects small joints, especially the joints of both hands and wrists, with swelling and stiffness.
Rheumatoid nodules may develop. These are small painless lumps which occur on the skin over the elbows and forearms but usually do no harm.
There may also be fever, an increase in the size of the liver, spleen and glands, and inflammation of the lining of the heart, lungs or abdomen.
Systemic JIA symptoms
This usually starts before the age of 5 years.
A high fever often occurs, most often in the afternoon or evening, with a rapid return of the temperature to normal.
A rash often appears with the fever. The rash is usually a light pink colour and quickly disappears.
Arthritis only occurs at the start of the disease in about one third of children but usually develops within a few months. The arthritis usually affects several joints.
Juvenile psoriatic arthritis symptoms
This affects girls twice as often as boys and tends to start at about 6 years of age. The arthritis affects both small and large joints. In over half of affected children, the arthritis starts before the psoriasis.
Enthesitis-related JIA symptoms
This affects boys much more often than girls and usually starts after 10 years of age. It often affects the legs and may cause pain in the heel. There is often swelling of a knee or foot. Psoriasis, eye inflammation and bowel inflammation may also occur with enthesitis-related JIA.
How is juvenile idiopathic arthritis diagnosed?
The diagnosis of juvenile idiopathic arthritis (JIA) is based on the symptoms and an examination by your doctor. Tests are important. They help to:
Find out what type of arthritis it is.
Make sure there are no other causes for the symptoms, such as infections, bone infection or a break (fracture) of a bone.
Blood tests include a test for anaemia (which may occur with JIA) and tests for inflammation (called ESR and CRP, which are often raised with JIA). Blood tests may also be useful to see whether any infection (virus or bacteria) has caused the arthritis and not JIA.
Other blood tests are used to see if there is a positive test for chemicals which are markers for different types of inflammation. Examples of these markers are called antinuclear antibodies, RF and HLA B27.
Other tests include the following:
X-rays, which are normal in the early stages of JIA but help to check for any other bone or joint problems such as infection or injury.
Ultrasound scans to see if there is any fluid in the joint and the extent of arthritis of the joint.
Magnetic resonance imaging (MRI) scans to show details of the damage to the joint and any changes of the bones surrounding the joints.
If there is any possibility of an infection in a joint then some fluid may be taken from the joint and sent to the laboratory for testing.
Continue reading below
What is the treatment for juvenile idiopathic arthritis?
The aims of treatment are to help the symptoms and reduce damage to joints. The other aim is to put the disease into remission. Doctors don't usually talk about 'curing' juvenile idiopathic arthritis (JIA), but they try to make the disease no longer active so there is no inflammation in any joint, and so there are no symptoms. This is called remission. It can last for months, for years, or in some cases can be lifelong.
Physical treatments
Physiotherapy and occupational therapy are used to help keep the affected joints working as normally as possible. They also reduce the risk of any permanent damage to the joints. Hydrotherapy (which involves different methods of treatment using water) can also be very helpful. Children should be encouraged to participate in as much physical activity as possible, including most sports and dancing. Moist heat can help to relieve pain, and in some cases shoe inserts (orthotics) can be useful.
Surgery may be needed in some cases where joint damage is severe, including joint replacement operations.
Medicines
Non-steroidal anti-inflammatory drugs (NSAIDs) can be used to help reduce pain and stiffness in the joints. Commonly used NSAIDs include ibuprofen, naproxen, indometacin and diclofenac. NSAIDs help to relieve symptoms but do not affect the progression of the disease.
Steroids help to settle inflammation and may be used in different ways:
Steroid tablets may be needed to improve the symptom relief and when the disease affects other parts of the body, such as the lining of the heart (pericarditis), lungs (pleuritis) and abdomen (peritonitis).
Steroid eye drops or creams may be needed for eye inflammation.
Disease-modifying antirheumatic drugs (DMARDs) may be used to help reduce the effects of the disease. These medicines can be very effective but also need very close supervision by your specialist doctor. DMARDs used for JIA include:
Biological medicines are another group of medicines used by specialists to help symptoms and reduce joint damage. These newer treatment options have improved outlook for people who don't respond to the other treatments. As they are relatively new medicines, there are still studies being done to establish whether there are any long-term health risks from taking them. Options include:
Tocilizumab
Infliximab
Abatacept
Adalimumab
Editor’s note
Dr Sarah Jarvis, 29th October 2021
NICE guidance on use of tofacitinib for active JIA
The National Institute for Health and Care Excellence (NICE) has recommended a medicine called tofacitinib as an option for treating JIA, as well as juvenile psoriatic arthritis, in people aged 2 years and older. It will only be offered if other medicines, such as DMARDs and some biological treatments, haven't controlled symptoms or aren't controlling them.
Tofacitinib can be used with methotrexate, or on its own if your child can't tolerate, or can't take, methotrexate.
What are the complications of juvenile idiopathic arthritis?
Without treatment, juvenile idiopathic arthritis (JIA) can lead to problems with growth, weakness of bones (osteoporosis) and a delay of puberty.
There may be long-term problems with the affected joints.
Some children who develop inflammation affecting the eye (uveitis) may have long-term reduced vision. They also have an increased risk of later developing cataracts or increased pressure in the eye (glaucoma).
Because they are unable to participate in all the usual physical activities with friends and at school, children with JIA may have emotional and behavioural difficulties and problems at school. This can be made worse because of having to deal with pain and the amount of time taken away from school in order to attend hospital appointments and admissions. Therefore, children with JIA and their families often need a lot of support.
What is the outlook (prognosis)?
With modern treatments, the outlook for most children with juvenile idiopathic arthritis (JIA) is now very good. However, the outlook is variable depending on the type and the severity of JIA. It is important for the diagnosis to be made early and treatment to be started early.
JIA is a serious disease because it can cause a lot of pain and can cause disability if joint damage is not prevented with early treatment. However, treatment can often stop disability and damage, and it is not life-threatening.
JIA is a long-term condition for most people who have it. Often the treatment results in remission, so that there are no symptoms and the joints have no inflammation. However, if symptoms return, further treatment may be needed. Remission can last for weeks, months, years or even be lifelong. Because it is not usually possible to predict for sure in advance how long remission will last, doctors don't usually use the word 'cured'. Instead they will usually talk about 'remission'. Depending on your type of JIA, however, your specialist may be able to give you a reasonable idea about your individual outlook and how long remission is likely to last.
Most children with JIA, having had treatment, have inactive disease within two years. That is, they have no symptoms and no inflamed joints. Many do not need to continue on treatment.
When children get too grown up for the children and adolescents' specialist (usually at age 16-18), they will be transferred to the care of an adult joint specialist (rheumatologist).
Understanding joints
The place where two bones meet is called a joint. Joints allow movement and flexibility of various parts of the body. The movement of the bones is caused by muscles which pull on tendons that are attached to bone. Cartilage covers the end of bones. Between the cartilage of two bones that form a joint there is a small amount of thick fluid called synovial fluid. This lubricates the joint, which allows smooth movement between the bones.
Normal joint
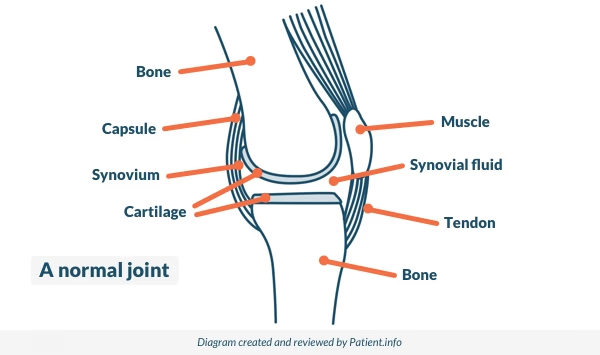
The synovium is the tissue that surrounds a joint. Synovial fluid is made by cells of the synovium. The outer part of the synovium is called the capsule. This is tough, gives the joint stability and stops the bones from moving out of joint. Surrounding ligaments and muscles also help to give support and stability to joints.
See the separate leaflet called Joint Pain for more general information about pain in joints. The separate leaflet on Arthritis may also be helpful.
Further reading and references
- Stoll ML, Cron RQ; Treatment of juvenile idiopathic arthritis: a revolution in care. Pediatr Rheumatol Online J. 2014 Apr 23;12:13. doi: 10.1186/1546-0096-12-13. eCollection 2014.
- Beukelman T; Treatment advances in systemic juvenile idiopathic arthritis. F1000Prime Rep. 2014 Apr 1;6:21. doi: 10.12703/P6-21. eCollection 2014.
- Abatacept, adalimumab, etanercept and tocilizumab for treating juvenile idiopathic arthritis; NICE Technology Appraisal Guidance, December 2015
- Giancane G, Consolaro A, Lanni S, et al; Juvenile Idiopathic Arthritis: Diagnosis and Treatment. Rheumatol Ther. 2016 Dec;3(2):187-207. doi: 10.1007/s40744-016-0040-4. Epub 2016 Aug 12.
- Davies K, Cleary G, Foster H, et al; BSPAR Standards of Care for children and young people with juvenile idiopathic arthritis. Rheumatology (Oxford). 2010 Jul;49(7):1406-8. doi: 10.1093/rheumatology/kep460. Epub 2010 Feb 19.
- What is Juvenile Idiopathic Arthritis?; JIA-at-NRAS - part of the National Rheumatoid Arthritis Society (NRAS)
- Tofacitinib for treating juvenile idiopathic arthritis; NICE Technology appraisal guidance, October 2021
Article History
The information on this page is written and peer reviewed by qualified clinicians.
22 Nov 2018 | Latest version

Feeling unwell?
Assess your symptoms online for free