Mastitis and breast abscess
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 19 Jan 2023
Meets Patient’s editorial guidelines
In this series:Breastfeeding your baby Bottle-feeding your babyBaby-led weaning
Mastitis is a painful condition of the breast which becomes red, hot and sore (inflamed). It is usually caused by a build-up of milk within the breast.
In this article:
Mastitis is a painful condition of the breast which becomes red, hot and sore (inflamed). It is usually caused by a build-up of milk within the breast (a blocked duct or engorgement). Sometimes it can be caused by germs (bacteria) that get into the milk ducts of the breast. This is often through a crack or sore in the nipple.
Continue reading below
What is mastitis?
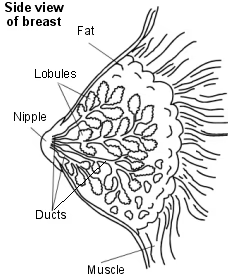
Cross-section view of breast
Mastitis is an inflammation of the breast, usually caused by a build-up of milk within the breast in women who are breastfeeding. It can be either:
Non-infectious - when the build-up of milk irritates the breast tissue, making it become red, hot and swollen (inflamed).
Infectious - when the build-up of milk becomes infected and the infection spreads to the breast tissue. The infection is caused by germs (bacteria) which may have come from the skin.
If non-infectious mastitis is not treated, it can become infectious mastitis. You can't tell which type of mastitis it is from looking at it, and the treatment is the same.
Anything which causes a build-up of milk in your breasts will make it more likely that you develop mastitis. Sometimes it occurs if you suddenly stop breast-feeding and the breasts become very swollen and sore because of the milk (engorged). This might happen if your baby starts to sleep through the night, or if you start using bottles for some feeds. If your baby is not feeding very well (for example, due to tongue-tie or illness) this might cause the milk to collect. Pressure on the breast due to a tight bra, or sleeping on your front, or wearing a seatbelt for a long time, may also be a cause. Breaks in the skin of the breast, such as cracked nipples due to your baby not latching on properly, can also make mastitis more likely. This is because the germs on the skin then have a route to the inside of the breast.
Patient picks for Pregnancy complications
Who gets mastitis?
You are most likely to get mastitis if you are a woman who is breastfeeding. It is sometimes called 'puerperal mastitis' or 'lactational mastitis'. It typically develops within the first few weeks of breastfeeding. At least 1 in every 10 breastfeeding women get mastitis, and it may be as many as 3 in every 10.
Mastitis sometimes occurs in women who are not breastfeeding (non-lactational mastitis). Germs (bacteria) get into the milk ducts of the breast to cause the infection. This may be through a crack or sore in the nipple or from a nipple piercing but it can happen when you don't have any problems with your nipples. Smoking can be a trigger because nicotine damages the ducts in your breasts.
Continue reading below
Mastitis symptoms
Mastitis causes an area of hardness, pain, redness and swelling in the breast and makes you feel generally unwell. It often starts in a wedge-shaped section of breast. It usually occurs in one breast only.
You also develop a high temperature (fever) and feel like you are coming down with flu. Other symptoms might include muscle pains, headaches and feeling tired and low.
Mastitis or blocked milk duct?
A blocked milk duct sometimes occurs in breastfeeding women. A blocked milk duct also causes a painful, swollen area in a breast. The overlying skin is sometimes red and inflamed, but it tends not to be as bad as mastitis and doesn't make you feel unwell.
When you feed your baby, the pain may increase due to the pressure of milk building up behind the blocked duct. A blocked milk duct will usually clear within 1-2 days and symptoms will then go. However, in some cases a blocked milk duct becomes infected and develops into mastitis. So, some cases of mastitis develop as a complication of a blocked milk duct, but some cases occur without a blockage happening first.
A blocked milk duct may clear more quickly if you feed your baby more often from the affected breast and gently massage your breast towards your nipple while you are breastfeeding.
Continue reading below
Mastitis treatment
Eat well and drink lots of fluids. Avoid tight-fitting bras.
Place a warm compress over your breast to help relieve the pain.
Regularly express milk from both breasts if you're breastfeeding.
See a midwife or doctor if you have any concerns
The quickest way to get rid of mastitis is to continue breastfeeding. Mastitis may need to be treated with a course of an antibiotic. However, a mild case may get better without any medical treatment. If you notice a tender swollen area in your breast when you're breastfeeding, it may be a blocked milk duct or mastitis developing. It may be reasonable to 'see how it goes' over a day or so.
Can mastitis be treated without antibiotics?
Continue to breastfeed. This will empty the affected breast and it keeps the milk flowing, and stops the breast from becoming engorged and making things worse.
Feeding from an infected breast does not harm your baby. If your baby swallows germs (bacteria) from an infected breast, the germs will be killed by the acid in your baby's stomach.
Feed on the affected side first, so it will empty well, for the next two or three feeds. (However, don't let the unaffected side become too full of milk.)
After feeding, consider expressing from the affected side as well. This is to make sure the breast is completely empty after a feed.
Before feeding, massage your breast gently. Or apply heat with a warm flannel, or a heat pack or by having a warm shower.
Ask your midwife or health visitor to check your breastfeeding technique and to check that your baby is latching on well.
If it is too painful to feed from the affected side, express the milk from that side with a breast pump.
Try to eat well and drink plenty of fluid.
However, if your symptoms become worse you should see a doctor. After talking to you and examining you, they may prescribe an antibiotic. They may suggest that you wait 24 hours before starting the antibiotics, if your symptoms are mild or have only just begun. The mastitis will usually clear within a few days of starting the antibiotic.
Mastitis complications
Occasionally, an abscess may form inside an infected section of breast. An abscess is a collection of pus that causes a firm, red, tender lump. This is thought to happen to between about 3 and 7 women with mastitis, out of every 100. If this happens to you, you will need to go to hospital for treatment. As well as the breast symptoms, you may feel flu-like or that you have a high temperature (are feverish). If you suspect an abscess, you should contact a doctor. The pus in a breast abscess needs draining with a needle and syringe, or even with a small operation (called incision and drainage).
The pus can be seen with an ultrasound scan. If the skin over the abscess is not broken, the pus can be drained with a needle and syringe by a doctor. If the skin is broken (or very thin) the doctor may need to make a small cut to let the pus drain out (called incision and drainage). You will probably need antibiotic medication as well.
If you have a breast abscess you should not feed from the affected side; however, you should express and discard the milk to stop your breast from becoming swollen with fluid (engorged).
Some other points about mastitis
Your doctor will choose an antibiotic that is safe to give to breastfeeding women and which will not harm your baby.
You can take simple painkillers (such as paracetamol or ibuprofen) to ease pain and reduce high temperature (fever). Cold packs can also be quite soothing when placed on the breast.
Your baby may refuse to feed from the affected breast, as the taste of the milk may change a little. If this happens, feed from the other breast. Do remember to express the milk (that your baby has refused to take) from the affected breast. This will stop the breast swelling and becoming more painful. It will also keep up the demand for milk, so production does not slow down.
Further reading and references
- The Baby Friendly Initiative; UNICEF UK
- Mastitis and breast abscess; NICE CKS, January 2021 (UK access only)
- Crepinsek MA, Taylor EA, Michener K, et al; Interventions for preventing mastitis after childbirth. Cochrane Database Syst Rev. 2020 Sep 29;9:CD007239. doi: 10.1002/14651858.CD007239.pub4.
- Pevzner M, Dahan A; Mastitis While Breastfeeding: Prevention, the Importance of Proper Treatment, and Potential Complications. J Clin Med. 2020 Jul 22;9(8):2328. doi: 10.3390/jcm9082328.
- Zakarija-Grkovic I, Stewart F; Treatments for breast engorgement during lactation. Cochrane Database Syst Rev. 2020 Sep 18;9(9):CD006946. doi: 10.1002/14651858.CD006946.pub4.
- Pileri P, Sartani A, Mazzocco MI, et al; Management of Breast Abscess during Breastfeeding. Int J Environ Res Public Health. 2022 May 9;19(9):5762. doi: 10.3390/ijerph19095762.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 22 Dec 2027
19 Jan 2023 | Latest version

Feeling unwell?
Assess your symptoms online for free

