Femoral Hernias Causes, Symptoms and Treatment
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Hernia article more useful, or one of our other health articles.
Treatment of almost all medical conditions has been affected by the COVID-19 pandemic. NICE has issued rapid update guidelines in relation to many of these. This guidance is changing frequently. Please visit https://www.nice.org.uk/covid-19 to see if there is temporary guidance issued by NICE in relation to the management of this condition, which may vary from the information given below.
What are femoral hernias?
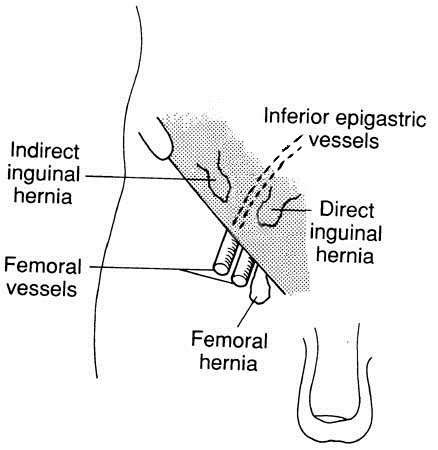
Hernias in the groin may be either inguinal or, less commonly, femoral in origin.
Inguinal hernia
The anatomy of the femoral canal is that the anterior border is the inguinal ligament, the posterior border is the pectineal ligament, the medial border is the lacunar ligament and the lateral border is the femoral vein.
Epidemiology
In 2020/21 there were 1,098 primary femoral hernia repairs in NHS hospitals in England, of which 1,036 were emergencies. This compares with a respective figure of 29,255 for primary inguinal hernia repair. These figures may have been artificially suppressed by the COVID-19 pandemic, during which routine surgery was stopped for a period of time.
Femoral hernias account for only around 5% of all abdominal hernias[1]:
- Femoral hernias are more common in women than in men.
- The incidence is highest in middle-aged and elderly women, especially if parous[2].
- They are rare in children. Sex incidence is equal. Diagnosis is often difficult[2].
- In elderly women the incidence of femoral hernia approaches that of inguinal hernia.
Femoral hernia symptoms (presentation)
- Presentation is as a lump in the groin, lateral and inferior to the pubic tubercle but a large hernia may bulge over the inguinal ligament and make differential diagnosis difficult.
- The femoral hernia often appears or swells on coughing or straining and reduces in size or disappears when relaxed or supine.
- There may be a cough impulse.
- It may be possible to reduce the hernia.
- There may be associated lower abdominal pain if incarceration occurs.
- According to findings, the hernia may be classified as reducible, irreducible, obstructed or strangulated.
Investigation
- Diagnosis is largely clinical but is often missed due to lack of examination of the groin as part of abdominal assessment.
- Imaging techniques are helpful, with ultrasound scanning as first-line followed by CT scanning and MRI scanning[3].
Differential diagnosis[4]
The differentiation between inguinal and femoral hernia is not easy and doctors often get it wrong. Surgeons, including those in training, tend to be better than GPs but they too are far from perfect and so alternative criteria have been suggested:
- Traditionally it is taught that an inguinal hernia will lie above and medially to the pubic tubercle whereas a femoral hernia lies laterally and below.
- This is not strictly true, as the internal ring is always lateral to the femoral canal and a small indirect inguinal hernia will therefore be lateral to the pubic tubercle.
- Also, a direct hernia will be lateral to or above the pubic tubercle.
- A better test might be to place the finger over the femoral canal for reducible hernias and then ask the patient to cough. This landmark is easily felt either by following the adductor longus tendon to below the inguinal ligament and then placing one's fingers anteriorly and laterally to the tendon or, alternatively, palpating the femoral artery and placing one's hand approximately a finger's breadth medially to it.
- When the patient coughs, a femoral hernia should remain reduced while an inguinal hernia will reappear as an obvious swelling.
Other causes of lumps in the groin include:
- Hydrocele (when differentiating from an inguinoscrotal hernia, note that it is possible to get above a hydrocele on examination).
- Spermatic cord hydrocele.
- Lymph node swelling.
- Psoas abscess or bursa.
- Saphena varix.
- Varicocele.
- Bleeding.
Femoral hernia complications
The main concern with a femoral hernia is strangulation.
- The risk of strangulation in a femoral hernia is 22% at 3 months and 45% at 21 months[2]. This is very much greater than for an inguinal hernia.
- Femoral hernias may not be noticed by the patient prior to strangulation, especially those who are obese[2].
- One study reported that 45.9% of patients present in the emergency situation[5].
Presentation
- If strangulation occurs, the lump will become red and tender as well as tense and irreducible.
- Other features include colicky abdominal pain, distension and vomiting, indicating a surgical emergency.
- Fluid and electrolyte imbalance must be corrected, followed swiftly by repair of the hernia.
- Failure to make a correct diagnosis is common.
- It is associated with a greater risk of needing bowel resection and a higher mortality[5].
Femoral hernia treatment and management[6, 7]
In view of the high risk of strangulation, all femoral hernias should be repaired as an elective procedure, but as soon as possible. There is no place for a truss for a femoral hernia.
- The International Guidelines for Groin Hernia Management advocate timely mesh repair by a laparo-endoscopic approach, provided expertise is available.
- Large-scale trials relating to femoral hernia repair are lacking, and many of the recommendations in the International Guidelines are based on evidence from inguinal hernia repairs. However, the evidence that is available such as studies from the Danish Hernia Database and the Swedish Hernia Registry all concluded that recurrence and re-operation rates after mesh repair are significantly lower than tissue repair and suturing.
- Furthermore, the International Guidelines report that a large database study showed no differences in postoperative pain between different mesh types and anatomical locations for the mesh devices. Three cohort studies from specialised hernia centres found that endoscopic repairs provide the opportunity to unerringly diagnose conditions which may have been obscure pre-operatively. Several other cohort studies of various sizes found significantly fewer recurrences after elective endoscopic femoral hernia repairs compared to open.
- In the absence of laparo-endoscopic expertise, however, open surgery should be performed. There are three surgical approaches that can be used to access the femoral sac, each named eponymously. There is a low approach (called Lockwood's), a trans-inguinal approach (called Lotheissen's) and a high approach (called McEvedy's).
- Each technique has the principle of dissection of the sac with reduction of its contents, followed by ligation of the sac and closure between the inguinal and pectineal ligaments.
- If a mesh is considered unacceptable, the abdominal wall can be reinforced with stitches. One study reported good results from a laparoscopic approach performed under spinal anaesthesia without using mesh.
Postoperative intestinal obstruction
A survey from Sweden examined the incidence of postoperative intestinal obstruction and found it low at 1.02 per 1,000[8]. The risk was higher with a transabdominal laparoscopic approach than with a totally extraperitoneal laparoscopic hernioplasty but other factors, such as previous abdominal surgery, were more important.
Prognosis
The mortality for elective hernia repair, both inguinal and femoral, is low - even at higher age. However, after emergency surgery, mortality is increased seven-fold[9].
Studies report that the overall operative mortality rate for strangulated hernias ranges from 1.4-13.4%[10].
- High age and the need to resect necrotic bowel increase the risk.
- The death rate from surgery for strangulated hernias has changed little over a 50-year period.
- Hence, femoral hernia must be repaired if at all possible, even in the elderly.
Further reading and references
Nikolopoulos I, Oderuth E, Ntakomyti E, et al; Intestinal Obstruction due to Bilateral Strangulated Femoral Hernias. Case Rep Surg. 20142014:195736. doi: 10.1155/2014/195736. Epub 2014 Jun 26.
Commissioning Guide, Groin Hernia; Royal College of Surgeons/British Hernia Society, 2016
Sucandy I, Kolff JW; Incarcerated femoral hernia in men: incidence, diagnosis, and surgical management. N Am J Med Sci. 2012 Nov4(11):617-8. doi: 10.4103/1947-2714.103343.
Kingsnorth A et al; Management of Abdominal Hernias, 2013.
Whalen HR, Kidd GA, O'Dwyer PJ; Femoral hernias. BMJ. 2011 Dec 8343:d7668. doi: 10.1136/bmj.d7668.
Yeo C et al; Shackelford's Surgery of the Alimentary Tract, 2012.
Humes DJ, Radcliffe RS, Camm C, et al; Population-based study of presentation and adverse outcomes after femoral hernia surgery. Br J Surg. 2013 Dec100(13):1827-32. doi: 10.1002/bjs.9336.
Sorelli PG, El-Masry NS, Garrett WV; Open femoral hernia repair: one skin incision for all. World J Emerg Surg. 2009 Nov 304:44. doi: 10.1186/1749-7922-4-44.
International guidelines for groin hernia management. Hernia. 2018 Feb;22(1):1-165. doi: 10.1007/s10029-017-1668-x. Epub 2018 Jan 12.
Bringman S, Blomqvist P; Intestinal obstruction after inguinal and femoral hernia repair: a study of 33,275 operations during 1992-2000 in Sweden. Hernia. 2005 May9(2):178-83. Epub 2004 Nov 26.
Nilsson H, Stylianidis G, Haapamaki M, et al; Mortality after groin hernia surgery. Ann Surg. 2007 Apr245(4):656-60.
Gul M, Aliosmanoglu I, Kapan M, et al; Factors affecting morbidity and mortality in patients who underwent emergency operation for incarcerated abdominal wall hernia. Int Surg. 2012 Oct-Dec97(4):305-9. doi: 10.9738/CC114.1.