Ill and feverish child
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Sarah Jarvis MBE, FRCGPLast updated 18 Feb 2020
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
This document is mainly based on the National Institute for Health and Care Excellence (NICE) guidelines 'Fever in under 5s', originally published in May 2007 and updated in 2013, 2017 and 20191 . It includes information on assessment and pre-hospital care by non-paediatric specialists.
Fever, or pyrexia, occurs when the body temperature rises above normal. The average normal body temperature taken in the mouth is 37°C but anywhere between 36.5°C and 37.2°C is deemed as normal. When temperatures are measured in the axilla they can be 0.2°C to 0.3°C lower than this. Aural (tympanic) thermometers may measure the temperature as higher. NICE guidelines define fever as "an elevation of body temperature above normal daily variation" but recognises that this is generally accepted as a temperature of 38°C or above.
Fever is one of the most common reasons for a child to be taken to see a doctor and is the second most common reason for a child to be admitted to hospital.
The cause of the fever can sometimes be hard to elicit and this can be a worry for healthcare professionals. It is usually due to a viral infection that is self-limiting but it can also be a sign of serious bacterial infection, including meningitis or septicaemia. Early diagnosis of serious infections in general practice is difficult as incidence is low, the child may present early in the disease process and diagnostic tools are more or less limited to history and examination2 .
Continue reading below
History from the parent or guardian
History should include asking:
How long has the fever been present?
Has the parent/carer been measuring temperature and, if so, by what method?
Is there a rash? If so, is it blanching or non-blanching?
Are there any respiratory symptoms - eg, cough, runny nose, wheeze?
Has the child been clutching at their ears?
Has there been excessive or abnormal crying?
Are there any new lumps or swellings?
Are there any limb or joint problems?
Is there any history of vomiting or diarrhoea? Is the vomiting bile-stained or is there any blood in the stool?
Has there been any recent travel abroad?
Has there been any contact with other people who have infective diseases?
Is the child feeding normally (fluids and solids as appropriate)?
What is the urine output? Have nappies been dry?
How is the child handling? Normal self/drowsy/clingy and so forth?
Have there been any convulsions or rigors?
Is there any significant past medical history/regular medication/allergy?
Is there a history of recent foreign travel, putting the child at increased risk of imported infection?
Other points to consider from the history:
Level of parental anxiety and instinct (they know their child best).
Social and family circumstances.
Other illnesses affecting the child or other family members. Has there been a previous serious illness or death due to febrile illness in the family?
Has the child been seen before in the same illness episode?
Examination of the child
Identify any immediately life-threatening features: assess airway, breathing, circulation and consciousness.
Consider sepsis. Always consider the possibility of sepsis and refer as an emergency if sepsis is suspected. See also the separate Sepsis (Septicaemia) article and the NICE guidelines 'Sepsis: recognition, diagnosis and early management'3 .
Editor's note |
|---|
Dr Sarah Jarvis, November 2021 Addition of definition of sepsis to NICE guidance A definition of sepsis: "Sepsis is a condition of life-threatening organ dysfunction due to a dysregulated host response to infection." A link to the risk stratification tool for children aged under 5 years with suspected sepsis (table 3 in the NICE guideline on sepsis)3 . |
Measure body temperature:
Infants <4 weeks: measure with an electronic thermometer in the axilla.
A child aged 4 weeks to 5 years: measure with either an electronic thermometer in the axilla, a chemical dot thermometer in the axilla or an infrared tympanic thermometer.
Take parental reported fever seriously.
Temperature ≥38°C in an infant aged 0-3 months is a red-light sign. (See table under 'Assessment of the Child using the NICE traffic light system', below.)
Temperature ≥39°C in a child aged 3-6 months should be considered at least an amber-light sign. (See 'Assessment of the Child using the NICE traffic light system' table, below).
Do not rely on the decrease in temperature (or lack of it) following anti-pyretic agents in distinguishing serious from non-serious illness.
Do not take the height of the temperature alone as a sign of serious disease in a child older than 6 months.
Do not use the duration of fever to predict the likelihood of serious disease except when considering Kawasaki disease. (See 'Signs of specific illnesses', below).
Look at the skin, lips and tongue colour: normal/pallor/mottled/ashen/blue?
Look at the activity level of the child: responsive/content and smiling/awake or easily rousable/normal cry?
Examine the respiratory system:
Measure the respiratory rate. There is tachypnoea if the respiratory rate is:
>60 breaths per minute at age 0-5 months.
>50 breaths per minute at age 6-12 months.
>40 breaths per minute at age older than 12 months.
Look for nasal flaring/grunting/chest indrawing.
Auscultate the chest for crackles or wheeze.
Measure oxygen saturation, if possible.
Examine the cardiovascular system:
Auscultate the heart. Is the pulse volume normal or weak? Blood pressure should be measured if the heart rate or capillary refill time is abnormal and there are the facilities to measure it.
Measure the heart rate.The presence of tachycardia indicates that the child should be put in at least the intermediate-group risk for serious illness.Tachycardia can be defined as:
More than 160 beats per minute in a child less than 12 months old.
More than 150 beats per minute in a child 12-24 months old.
More than 140 beats per minute in a child 2-4 years old.
Assess the level of hydration: do the eyes and skin look normal? Is there reduced skin turgor? Are the mucous membranes moist? What is the capillary refill time? (NB: a capillary refill time ≥3 seconds should be considered an intermediate-risk group marker for serious disease ('amber' sign). Are the extremities warm or cool? Is the child feeding normally? Is the urine output reduced?
Examine for other features:
Rash: if there is a rash, is it blanching or non-blanching?
Are there any new lumps?
Is there limb or joint swelling or any problem with weight-bearing?
Is the fontanelle sunken, normal or bulging?
Is there neck stiffness?
Are there focal neurological signs/convulsions?
Continue reading below
Signs of specific illnesses
After history and examination have been performed, specific illnesses should be considered.
Meningococcal disease: this should be considered in any child with a fever and a non-blanching rash, especially if the child looks ill, there are purpura present (non-blanching lesions >2 mm in diameter), capillary refill time is ≥3 seconds or there is neck stiffness.
Meningitis: consider this if there is fever plus any neck stiffness, bulging fontanelle, decreased consciousness or convulsive status epilepticus. Classical signs of meningitis may be absent in infants.
Herpes simplex encephalitis: consider if there is fever plus focal neurological signs, if there are focal seizures or if there is a reduced level of consciousness.
Pneumonia: consider if there is fever plus increased respiratory rate (see above), if there are chest crackles, nasal flaring or chest indrawing, and cyanosis or oxygen saturation ≤95% on air.
Urinary tract infection: consider in any child <3 months with fever. In children older than 3 months, consider if there is associated vomiting, poor feeding, lethargy, irritability, abdominal pain or tenderness, urinary frequency or dysuria or offensive urine or haematuria.
Septic arthritis and osteomyelitis: consider if there is limb or joint swelling or non-use or non-weight-bearing of an extremity.
Kawasaki disease: consider this if there is fever that has lasted >5 days. Enquire about additional features below, as these may have resolved by the time of assessment. Be aware that children under 1 year may present with fewer of the features below than older children. Additional features may include:
Bilateral conjunctival injection without exudate.
Erythema of lips or oral and pharyngeal mucosa.
Dry cracked lips or strawberry tongue.
Change in the extremities (oedema, erythema, desquamation).
Polymorphous rash.
Cervical lymphadenopathy.
Fever without an obvious focus
This is a common scenario, and most often will be due to a viral infection. The NICE traffic light system below helps the primary care practitioner determine which cases are more likely to be due to a serious or life-threatening bacterial infection and should therefore be referred to secondary care for further assessment and management.
In primary care, history and examination are the mainstays of assessing fever without an obvious focus to establish severity and to try to ascertain the cause, and urine should be tested In all children with an unexplained fever ≥38°C4 . In a significant number of cases of children with a fever, no specific cause will be established. Antibiotics should not be used empirically for children with fever without an apparent cause1 .
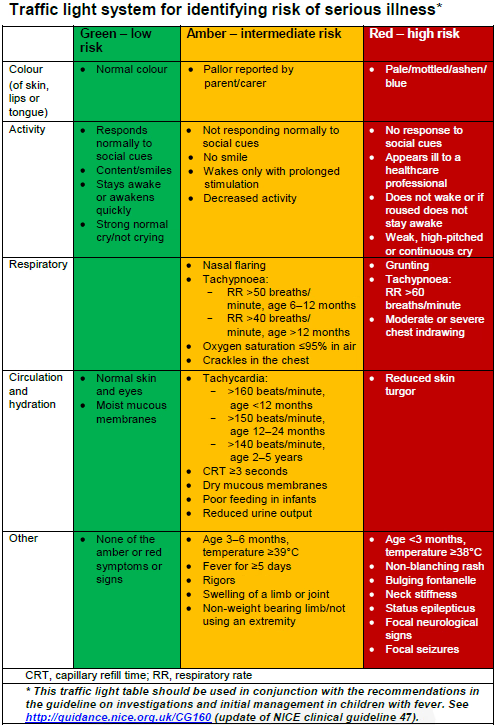
Assessment of the child using the National Institute for Health and Care Excellence traffic light system
NICE recommends that a traffic light system should be used to predict the risk of serious illness when the symptoms and signs have been elicited from the history and examination. Allowance should be made for individual disabilities when assessing learning-disabled children.The following table summarises this system. If the child has any of the symptoms or signs in the amber column, they are at intermediate risk of serious illness. If they have any of the symptoms or signs in the red column they are at high risk of serious illness. Children with symptoms or signs in the green column and none in the red or amber column are at low risk of serious illness. Management of fever should be guided by the level of risk.
NICE Traffic light chart 2013
Important information |
|---|
National Institute for Health and Care Excellence (2007) CG160 Feverish illness in children. London: NICE. Available from www.nice.org.uk/guidance/CG1607[now www.nice.org.uk/guidance/ng143] |
Continue reading below
Management
Management by remote assessment - eg, by telephone
The history should be elicited from the parent/carer as outlined above. The parent/carer should be questioned as to any signs that they may be able to recognise.
If immediate life-threatening illness is suspected due to obvious difficulty of the airway, breathing, circulation or conscious level, 999/112/911 should be called and the child should be referred for emergency medical care.
Children with any red features not considered to have an immediate life-threatening illness should be seen within two hours by a healthcare professional.
Children with any amber features should be seen by a healthcare professional but the assessment of urgency of the appointment is left to the clinical judgement of the assessor.
Children with only green features can be managed at home with advice for parents and carers, including advice on when to seek further help.
Management by the non-paediatric practitioner
This includes professionals working in primary care and also those working in general accident and emergency departments.
If immediate life-threatening illness is suspected due to obvious difficulty of the airway, breathing, circulation or conscious level and the child is not already in hospital, 999/112/911 should be called and the child should be referred for emergency hospital care. If the child is in hospital, the paediatric team should be called. Basic life support measures should be undertaken by the practitioner.
Otherwise, clinical assessment, including history taking and examination, should be carried out and any symptoms and signs of serious illness and specific diseases should be elicited.
Assessment using the traffic light system should be performed.
Children with any red features should be referred for urgent assessment by a paediatrician.
Children with any amber features in whom a specific diagnosis has not been made, should either be referred to urgent paediatric care or the carers of the child should be given a 'safety net', either detailing exactly when to seek further help (ie specific warning symptoms or signs) or arranging a further follow-up assessment.
Children with only green features can be managed at home with advice for parents and carers, including advice on when to seek further help.
Oral antibiotics should not be prescribed if there is no identifiable source of the fever.
Management of specific diseases
If there is no obvious source of infection, urine should be tested in children presenting with fever.
If meningococcal disease is suspected, antibiotics should be given at the earliest opportunity.
Advice to parents or carers for home care of the child
Antipyretic treatment: tepid sponging is not recommended. Do not underdress or over-wrap children. Give either paracetamol or ibuprofen for discomfort or distress but not for the sole reason of reducing the temperature. One agent can be changed for the other if the child does not respond. If distress persists or recurs before the next dose is due, the agents can be alternated. Do not use both agents simultaneously. Advise parents that antipyretic agents do not prevent febrile convulsions and should not be used specifically for this purpose.
Give regular fluids: breast milk if the child is breastfed.
Monitor for signs of dehydration: sunken fontanelle or eyes, dry mouth, absence of tears, poor appearance, reduced urinary output.
Monitor for appearance of rash: advise on how to assess if a rash is non-blanching.
Get up in the night to monitor the child.
Keep the child away from school or nursery while they have a fever and notify them.
When to seek further help: if the child has a seizure, develops a non-blanching rash, appears less well than when they were last assessed by a healthcare professional, the parent or carer is worried, the fever lasts >5 days, the parent or carer is distressed or feels they cannot look after the child.
Provide written information: give the parent or carer an appropriate advice sheet (such as the Patient.info patient advice on fever in children).
Further reading and references
- Feverish illness in children: discharge advice template; NICE, March 2013
- Fever in under 5s; NICE Quality Standards, July 2014
- Fever in under 5s: assessment and initial management; NICE Guidance (last updated November 2021)
- Thompson M, Van den Bruel A, Verbakel J, et al; Systematic review and validation of prediction rules for identifying children Health Technol Assess. 2012 Mar;16(15):1-100.
- Sepsis - recognition, diagnosis and early management; NICE Guideline (July 2016 - updated January 2024)
- Urinary tract infection in under 16s: diagnosis and management; NICE Clinical guideline (August 2007, updated October 2018)
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Feb 2025
18 Feb 2020 | Latest version

Feeling unwell?
Assess your symptoms online for free