Extradural haematoma
Peer reviewed by Dr Pippa Vincent, MRCGPLast updated by Dr Toni HazellLast updated 24 Oct 2023
Meets Patient’s editorial guidelines
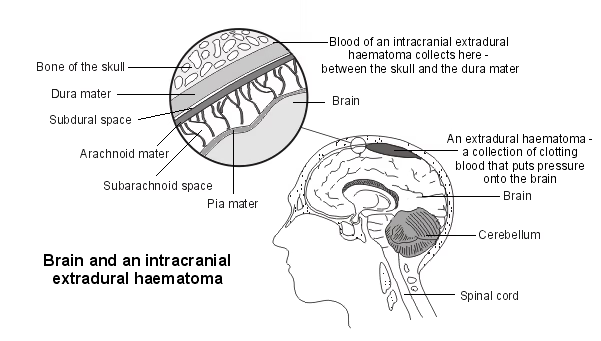
An extradural haematoma is a collection of blood in the 'potential' space between the skull and the outer protective lining that covers the brain (the dura mater). It usually occurs because of a head injury. It is a serious condition and emergency treatment is needed, often in the form of an operation to remove the haematoma.
In this article:
Continue reading below
What is an extradural haematoma?
An extradural haematoma is a collection of blood in the extradural space. 'Extradural' means outside the dura.
In the spine, the epidural space is the space between the backbone (vertebral column) and the outer protective lining that covers the brain (the dura mater). An extradural haematoma that occurs in the spine is called a spinal extradural haematoma.
In the head, the epidural space is the 'potential' space between the skull and the dura mater. (The dura mater is usually bound quite firmly to the inside of the skull.) An extradural haematoma that occurs in the head is called an intracranial extradural haematoma.
An extradural haematoma is sometimes called an epidural haematoma because the blood collects in the epidural space. It is also sometimes called an extradural haemorrhage (haemorrhage means that bleeding has occurred).
There is a similar condition called subdural haematoma where a collection of clotting blood forms in the subdural space.
See the end of this leaflet for more information about the coverings of the brain and spine.
What causes an extradural haematoma?
Spinal extradural haematoma
Sometimes a spinal extradural haematoma can occur after an injury around the spinal area. For example, it can (rarely) occur after a lumbar puncture (a procedure where a sample of fluid that surrounds the brain and spinal cord is taken with a needle to help diagnose conditions such as meningitis).
It may also (rarely) occur after an epidural anaesthetic (a common type of pain relief used during childbirth and for other reasons). However, this is not common.
Rarely, a spinal extradural haematoma can occur spontaneously in people who are, for example, taking anticoagulation medication to thin the blood or who have blood clotting problems.
Intracranial extradural haematoma
An extradural haematoma most commonly occurs after a fractured skull caused by a head injury. Typically, an extradural haematoma is caused by a severe head injury - for example, in a road traffic accident.
The blood from a damaged artery (often the middle meningeal artery) usually collects in the epidural space soon after a head injury and symptoms are usually noticed quickly. Occasionally, bleeding can occur more slowly and there are only minor symptoms (and so not noticed) until some days after a head injury.
The rest of this leaflet just discusses intracranial extradural haematoma.
Continue reading below
How common is an intracranial extradural haematoma?
Head injuries are often minor and not serious. Most people with a minor head injury will not get an intracranial extradural haematoma. One develops in about 2 in 100 people with a head injury. It usually occurs after a severe head injury, for example one that causes a fracture of the temporal bone.
The peak age range in children is between 11 and 16 years. It is less common over the age of 60. An intracranial extradural haematoma is also more common in men than in women.
Someone who drinks excessive amounts of alcohol may be more likely to develop an intracranial extradural haematoma.
Symptoms of an extradural haematoma
You may lose consciousness at the time of the head injury but this does not always happen. Loss of consciousness may occur at the time of the head injury, followed by a 'lucid interval' of a few hours when you appear relatively well and normal. Later, you may deteriorate and lose consciousness again as the haematoma forms. However, not everyone shows this classic pattern.
If you are conscious, other symptoms include:
Drowsiness.
Severe headache.
Feeling sick (nausea).
Vomiting.
Confusion.
Weakness of an arm and/or a leg.
Speech difficulties.
A fit (seizure).
Some people with an intracranial extradural haematoma can be talking one minute and appear relatively well and can then become very ill and lose consciousness the next.
Anyone who loses consciousness or has any of the symptoms listed above should be taken to hospital immediately.
Continue reading below
How is an intracranial extradural haematoma diagnosed?
Someone with a suspected intracranial extradural haematoma should be seen in a hospital. It is a serious condition and emergency treatment is needed. Investigations will include:
A CT scan of the head is good at detecting an intracranial extradural haematoma. It can also show any skull fracture that may be present.
You may need other scans or X-rays depending on whether any other injuries are suspected. For example, an X-ray of your neck may be taken to rule out any co-existing neck injury.
Treatment for an extradural haematoma
Stabilising your condition
The first priority is to stabilise your condition. You may need treatment to stabilise your blood pressure. If you have breathing difficulties or your consciousness level is affected, you may need help with your breathing using a ventilator. If there are signs of raised pressure inside your head, emergency treatment is needed.
Monitoring
A small intracranial extradural haematoma that is not producing any symptoms (or the symptoms are not severe) can sometimes be treated just by careful monitoring and observation. The blood clot may clear (re-absorb) by itself.
Surgery
However, surgery is generally needed to treat a large intracranial extradural haematoma and relieve pressure on the brain This involves removal of the haematoma. Most commonly, surgery either involves making 'burr holes' (small, in the skull) or an operation called a craniotomy.
Close follow-up is needed after the operation, usually in an intensive care unit, where your level of consciousness and other vital signs will be monitored.
What is the outlook (prognosis)?
Provided that quick treatment is carried out, the outlook is generally good. However, the outlook is not as good in those who are unconscious before they have surgery.
There is a risk of permanent brain injury even if an intracranial extradural haematoma is treated. This may lead to problems such as weakness on one side of the body, speech problems or fits (seizures).
Can an intracranial extradural haematoma be prevented?
If you or your children take part in sports such as cycling, roller-blading, skiing or skate-boarding, you should make sure that you wear a helmet/protective headgear so as to reduce the risk of serious head injury. The same applies for horse riding and riding a motorcycle.
Seat belts and child safety seats should always be used in cars and other vehicles.
Sensible alcohol consumption. Alcohol is often a contributing factor in serious head injury, whether this is drinking and driving or binge drinking followed by falls or fighting.
The coverings of the brain and spine
The meninges are the protective lining surrounding and enclosing the brain within the skull and the spinal cord. There are three layers of meninges:
The outermost layer which lies next to the skull or the vertebral column is called the dura mater.
The middle layer is called the arachnoid mater.
The inner layer which is closest to the brain or the spinal cord is called the pia mater.
There are also three spaces between the layers of meninges:
The epidural space is the space between the vertebral column and the dura mater. (There is only a 'potential' epidural space in the head between the skull and the dura mater.)
The subdural space is the space between the dura mater and the arachnoid mater.
The subarachnoid space is the space between the arachnoid mater and the pia mater.
extradural haematoma
Patient picks for Head Injuries
Further reading and references
- Zhong W, Sima X, Huang S, et al; Traumatic extradural hematoma in childhood. Childs Nerv Syst. 2012 Dec 13.
- Araujo JL, Aguiar Udo P, Todeschini AB, et al; Epidemiological analysis of 210 cases of surgically treated traumatic extradural hematoma. Rev Col Bras Cir. 2012 Jul-Aug;39(4):268-71.
- Nath PC, Mishra SS, Das S, et al; Supratentorial extradural hematoma in children: An institutional clinical experience of 65 cases. J Pediatr Neurosci. 2015 Apr-Jun;10(2):114-8. doi: 10.4103/1817-1745.159192.
- Zwayed ARH, Lucke-Wold B; Conservative management of extradural hematoma: A report of sixty-two cases. Neurol Clin Neurosci. 2018 Jun;2(2):5-9. Epub 2018 Apr 30.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 22 Oct 2028
24 Oct 2023 | Latest version

Feeling unwell?
Assess your symptoms online for free
