Root canal treatments
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Ben Williams, MB ChBLast updated 9 Jul 2017
Meets Patient’s editorial guidelines
In this series:ToothacheTooth decayOral hygiene
This page has been archived.
It has not been reviewed recently and is not up to date. External links and references may no longer work.
A root canal treatment is performed if you have an infection in the centre of your tooth. Root canal treatment is not painful and can save a tooth that might otherwise have to be removed completely.
In this article:
Continue reading below
What is the root canal in a tooth?
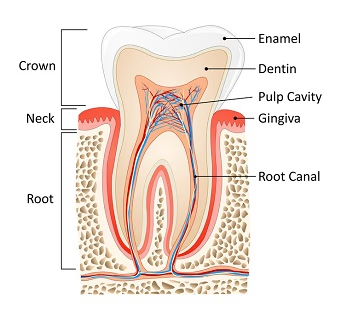
In the centre of each tooth, under the outer layers of enamel and dentine, is a collection of nerves and blood vessels called the dental pulp. The vessels of the pulp enter the tooth through a hole in the root tip, or root apex, and run along the root canal to a space in the centre of the tooth crown called the pulp cavity, or chamber.
Root canal
The function of the pulp is to:
Supply the cells that create dentine with oxygen and nutrients.
Detect stimuli such as pressure or temperature which could damage the tooth.
If the pulp dies it will decompose and leak out of the root causing the bone around the root apex to become inflamed, especially if the dead pulp is infected with germs (bacteria). The body's immune system will attempt to heal the bone but will not be able to cure it completely because the dead pulp will continue to leak out from the root canal and cause further damage.
The only way to effectively treat dead or dying pulp is to remove it. This can be achieved by:
Root canal treatment (RCT), or having a root filling: this procedure aims to remove the dead pulp and any infection from inside a tooth and then to place a filling within the root canal system that prevents future bacterial growth/spread within the space.
Tooth extraction: once the tooth containing the dead pulp has been removed, your body will itself be able to deal with any residual infection.
The main benefits of RCT over extraction are that your smile and ability to chew food will not be compromised by missing teeth.
What are the main causes of pulp damage?
Tooth decay (dental caries)
Deep dental cavities contain millions of germs. As they spread through the dentine they will cause pulp inflammation and toothache which if left untreated will eventually kill the pulp. The bacteria will continue to pass through the dentine until they have infected the dead pulp space.
Dental injury
This is usually due to an accident, sporting injury or assault:
Periodontal trauma (injury to the gum, bone and ligaments around a tooth): if a tooth receives a sudden blow, the root will be forced against the bone. Often this just results in minor tenderness when biting for a few days. However, in severe cases the vulnerable area where the nerves and blood vessels of the pulp enter the root apex may be crushed or severed. This will result in the death of the pulp inside the tooth because its blood supply has been stopped. Depending on the type and severity of injury the dead pulp space may remain free of bacteria or it might become infected.
Tooth fracture: moderate or large fractures can damage or expose the dental pulp, resulting in severe pulp inflammation, pulp infections and pulp death. Prompt dental treatment will improve the chances of preserving pulp vitality, keeping the pulp alive, but in severe cases tooth extraction or root canal treatment (RCT) will be necessary.
Front teeth are more vulnerable to both types of dental injury but back teeth with cavities or fillings can also fracture too. Custom-made mouth guards are the most effective way to protect your teeth if you participate in activities which pose a risk of dental injury.
Dental treatment
Many dental procedures will cause temporary pulp inflammation, which resolves after a few days. Occasionally, usually after extensive decay removal, the inflammation will be severe and result in the death of the pulp. Your dentist should advise you of this risk before commencing certain procedures - for example, when preparing a tooth for a crown or placing a very deep filling. Orthodontic treatment can also cause pulp death if braces are tightened too quickly.
Occasionally it may be necessary to remove a healthy tooth pulp in order to use the space within the root canal and pulp chamber to support a filling on worn or damaged teeth. Removing a healthy pulp is called elective devitalisation.
Continue reading below
What are the consequences of a dead pulp?
If a pulp dies without becoming infected by bacteria it will decompose yet might cause little or no bone damage at the root apex. The tooth may be tender to bite on to or it could be symptom-free. Often the only indication that your tooth might have a dead pulp is a change in colour from white to grey, usually over several months or years.
If the tooth is structurally sound then RCT is usually the treatment of choice. Occasionally, if there are no symptoms or signs of bone damage at the root tip, it may be acceptable simply to monitor the tooth with an X- ray every few years. If the review X-rays indicate any bone changes at the root apex then RCT will be necessary.
If a dead or dying pulp becomes infected with bacteria, they will multiply and spread via the root canal out into the bone. This will make the tooth painful to bite on to. As more bone is destroyed, the infection can pass through the bone to the soft tissues. Oddly, this might relieve the pressure under the tooth and possibly stop the pain on biting. If the infection passes from the bone to the gum it will form a localised infection called a dental abscess, or gum boil.
If these types of abscess are addressed promptly by a dentist they are not usually very serious. They do not require antibiotics and tend to heal well after RCT or extraction. However, if the infection passes through the bone below the level of the gums it can form a spreading soft tissue infection which is more serious. Usually a spreading dental infection is seen as a painful swelling of the cheek or under the lower jaw; however, in severe cases it can obstruct the airway, cause total loss of vision or even infect the brain.
All spreading dental infections should be assessed urgently by a dentist. They can develop in only a few hours, so if you think a dental infection may be the cause of a facial swelling that affects your ability to breathe or swallow, or is causing your eyelids to swell and close, you should seek urgent medical/dental advice.
What symptoms show that I might need root canal treatment ?
Your dentist may suspect that you have a dead or dying pulp if you have a combination of any of the following symptoms:
Discolouration: a front tooth with a dead pulp will often turn grey or brownish, possibly over the course of several years.
An abscess or a small persistent small hole on the gum: it may look like a pimple.
Signs or symptoms of a spreading dental infection: high temperature, tender or swollen lymph nodes under the lower jaw or upper neck area, or swelling of the soft tissues of the face and under the lower jaw.
Recent toothache: severe throbbing tooth pain of irreversible pulpitis and/or pain on biting. When the pulp has died the throbbing toothache may stop completely.
A history of trauma to the tooth: the dental pulp of front teeth is more likely to die from trauma while for back teeth, tooth decay or deep fillings are the more likely cause.
Pain which lasts more than three days after dental treatment: especially if it involved dental work close to the pulp.
Continue reading below
Will I need any tests before the root canal treatment?
To confirm whether the tooth pulp is alive, dead or inflamed your dentist will perform the following tests-
Percussion testing: tapping or pushing firmly on individual teeth to identify which ones feel tender.
Pulp vitality testing: this involves holding hot or cold pieces of cotton wool against individual teeth. Failure to feel the temperature change indicates that the pulp may be dead or has shrunk away inside the tooth. An electric pulp tester is a pen-shaped device that also tests the status of the pulp; a tingling sensation will indicate that the pulp is still alive.
Dental X-rays: these show the proximity of fillings to the pulp and the presence of inflammation or bone loss around the apex of the tooth.
Are there any other checks before you start the treatment?
If it is confirmed that you have a dead or dying pulp, your dentist will assess your general dental health to see if RCT is a viable option. There would be little benefit in spending hours performing RCT on a loose tooth that was likely to fall out within a year. Other factors that your dentist may discuss with you include:
Settling of symptoms: the pain related to an infection from a dead pulp may persist for several days after RCT or require several dental appointments before it resolves completely. You may prefer to have the tooth extracted rather than face the possibility of continued discomfort even for a short time.
Choice of final restoration: teeth with RCT are more vulnerable to fracturing than teeth with healthy pulps, especially back teeth. To reduce this risk, they should usually be restored with a crown or a filling that covers the whole biting surface. The different options will vary in terms of cost.
Your availability: some RCTs can be completed in half an hour whilst others may require multiple appointments. Reasons for the differences in treatment duration include:
Variations in root canal shape and location - incisor and canine teeth tend to have a single root canal which is usually straight, easy to locate and fairly easy to treat. Molar teeth on the other hand can have 3 to 6 canals which are smaller, are harder to access at the back of the mouth and can be curved or even 'S'-shaped. Some root canals can also be blocked by layers of dentine which makes treatment more difficult.
The cause of the pulp death/damage - a tooth that has been fractured in a sporting injury may have little or no pulp infection and might undergo RCT in a single appointment. Teeth with a lot of infection in the root canals and bone may require several cleaning appointments before the infection has resolved sufficiently to complete the RCT.
What is involved in root canal treatment?
The RCT procedure will usually involve the following stages:
Pre-operative X-ray: before starting RCT your dentist should always have a current X-ray to show:
The extent of any bone destruction at the root apex.
The shape, patency (whether the canals are open or blocked) and length of the roots.
The presence of any decay in the tooth.
Local anaesthetic (LA) and placing a rubber dam: the LA may not be necessary if your pulp is already dead or was removed at an earlier appointment. All RCT should be completed under rubber dam; this helps to ensure you don't swallow or inhale any of the small RCT instruments or cleaning solutions. It also prevents saliva and germs (bacteria) from re-contaminating the root canal after it has been disinfected.
Access the pulp chamber: this is achieved by drilling a hole in the top of the tooth, often through an existing filling to preserve tooth tissue. The dead or dying pulp remnants are removed and the small holes of the root canals are identified. The length of each root canal will be carefully calculated using an X-ray or an electrical measuring device.
Canal disinfection and preparation: bacteria are killed and infected debris is removed by repeatedly flushing the canal, usually with dilute solutions of sodium hypochlorite (bleach). It is not possible to remove 100% of the bacteria from an infected canal but the aim is to remove as many as possible. The canals are also prepared using specialised screw-shaped instruments called endodontic files. These may be handheld or used in a slow-speed dentist's drill. The purpose of shaping is to remove infected dentine and form the narrow canal into a cone shape which is easier to fill.
Assess level of infection: if your dentist suspects there is too much infection in the tooth or bone it may be necessary to place an antibacterial temporary filling for a few weeks. When the infection has healed, your RCT can continue. If there is little or no infection when the pulp was removed, your dentist might be able to complete the RCT in a single appointment.
Placing the root filling: the final stage of RCT involves packing the root canal space, usually with a rubbery filling material and cement. This is done as tightly as possible to ensure that any remaining bacteria in the root canal are unable to get to a food source or spread out inside the root. Without food they should die off over time.
Final X-ray and tooth filling: an X-ray is taken to assess whether the root filling material has been placed and packed correctly to the apex of the root canal. If necessary, adjustments can be made. A final tooth filling will then be placed to seal off the root filling and restore the tooth.
Possible crown placement: if it is necessary to place a crown on the tooth, your dentist will often wait for several months after the RCT was completed. This provides some reassurance that the RCT has been successful before commencing with the crown treatment.
Are there different types of root canal treatment?
As well as the standard RCT outlined above there are several other treatments which relate to the root canal and dental pulp.
Re-RCT
If a first attempt at performing RCT on a tooth has failed, it may be possible to remove the root filling material and attempt a retreatment. The success rate for re-RCT is slightly lower than for a first RCT on a tooth but there are many instances where they can be effective. For example, if an RCT failed because one of the root canals in a molar tooth was not identified and cleaned then a second attempt which filled all the canals might be more successful.
Apicectomy
If a tooth has been root filled to a high standard but there is still ongoing infection in the bone at the tip of the root it might not be possible to attempt a re-treatment without damaging the tooth. In these cases a dentist might raise a flap of gum and remove bone to expose the tooth root. The leaking root tip can be then be cut off and the root canal sealed directly to ensure that no bacteria can leak from within the remaining root canal. This procedure usually takes about an hour and is performed under local anaesthesia.
Pulp cap and pulpotomy
If decay removal or a tooth fracture results in a small part of a healthy pulp becoming exposed, your dentist may try to retain the pulp vitality, or keep the pulp alive. This is achieved by placing a special layer of material, which promotes the formation of new dentine, on top of the exposed pulp before placing a filling. This technique is called a direct pulp cap. Alternatively, if only the exposed part of the pulp appears to be infected or inflamed then just the top half of the pulp can be removed, from within the pulp chamber. This leaves the healthy pulp still alive in the root canals which can be sealed off and protected before the tooth is filled. Follow-up X-rays and vitality tests are necessary to monitor the success of these 'vital pulp' techniques.
How much does a root canal treatment cost?
This varies depending on the severity of the case, your personal circumstances and where you go for treatment. The more straightforward your tooth is to deal with, the less the procedure will cost. In some cases you could get treatment for a reduced cost or even for free - for instance, if you are pregnant or under the age of 18 years (on the NHS).
How successful will the root canal treatment be?
The success of RCT can only be judged over time. Dental abscesses and pain on biting will often resolve after RCT but they will return if the root canal was not cleaned or sealed properly. To monitor healing, a review X-ray should be taken one year after an RCT is completed.
If the tooth is symptom-free and the X-ray shows signs of bone healing around the root apex, this indicates that the RCT may be successful. A further review X-ray after 3 to 5 years is advisable.
If the review X-ray shows evidence of ongoing bone destruction around the root apex, the RCT has failed. The tooth may be painful to bite on to (or it might be symptom-free) and there may be evidence of soft tissue infection in the form of an abscess or draining sinus on the gum. The main treatment options for a failed RCT include re-RCT, tooth extraction or possibly apicectomy.
If the X-ray shows neither sign of healing nor increased damage to the bone at the root apex and the tooth is symptom-free, it is usually acceptable to monitor the tooth with X-rays intermittently for several years. Evidence of further bone damage or infection should be treated as for a failed RCT.
Studies indicate that approximately 90% to 95% of teeth that have undergone their first RCT will still be present after five years. Your dentist will discuss any factors that may affect the success of your RCT with you.
What are the possible complications of root canal treatment?
Complications and causes of RCT failure are outlined below.
Perforation: when cleaning and shaping the root canals, your dentist might accidentally pass the drill or endodontic files through the floor of the pulp chamber or the side of the root into the bone. Depending on the size and location of the hole it may be possible to repair it, otherwise it will be necessary to extract the tooth.
Fractured instrument: RCT files can occasionally fracture inside the root canal. If it is not possible to remove the broken piece then the chances of achieving a successful RCT can be significantly reduced. However, if the canal was disinfected properly prior to the fracture and the fragment of instrument was located in a favourable position within the root canal it may be possible for the RCT to be completed and successful.
Root filling material too long or short: an ideal root filling should fill the canal right up to the tip of the root. If the filling material is pushed through the root apex, out into the bone then the bone may become irritated and fail to heal properly. If the root filling material is not packed tightly or does not fill the canal properly then bacteria will multiply in the spaces and continue to infect the bone.
Disinfectant passed through root apex: the cleaning solution used to disinfect the root canal should only be used within the root canal. If it is accidentally squirted through the root apex into the bone it can cause severe inflammation, pain and damage to the bone and soft tissues.
Leaking restoration: on completion of RCT it is vital to have an effective tooth filling or crown to seal off the root filling. If this is not achieved then decay, food and bacterial leakage will cause the root filling to fail.
Tooth fracture: one function of the pulp is to detect biting forces and prevent tooth fractures caused by biting too hard. Thus back teeth that have been root filled or are midway through RCT are more vulnerable to fracturing than those with healthy pulps. Your dentist will advise you to have a soft diet until your RCT has been completed and a suitable crown or filling has been placed to reduce the risk of tooth fracture.
Your dentist will assess your tooth and warn you of any possible complications before starting treatment. For example, if you have very curved roots you should be told that the risk of perforation is higher than if the tooth had straight roots. If your tooth has features which indicate that the procedure might be too challenging or if your dentist encounters one of the complications outlined above, they may refer you to an RCT specialist. They are also called endodontists.
What if I don't have the treatment?
If you have an infected pulp but opt not to have a root canal treatment, you risk having to have the tooth taken out and, more seriously, the infection spreading inside your mouth or across your face and neck. It could also result in several tooth extractions.
Further reading and references
- Root canal treatment - site includes 'find a member' function; British Endodontic Society
Article History
The information on this page is written and peer reviewed by qualified clinicians.
9 Jul 2017 | Latest version

Feeling unwell?
Assess your symptoms online for free