Meniscal tears and other knee cartilage injuries
Peer reviewed by Dr Krishna Vakharia, MRCGPLast updated by Dr Colin Tidy, MRCGPLast updated 16 Aug 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Meniscal tears article more useful, or one of our other health articles.
In this article:
Continue reading below
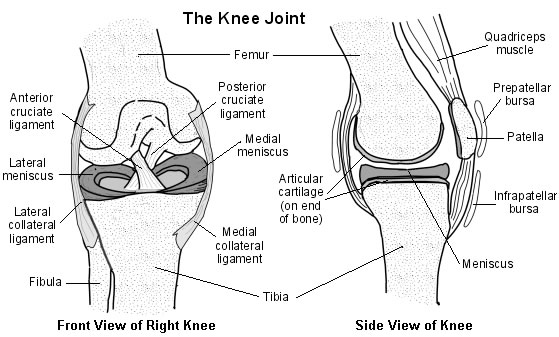
Anatomy of the knee
Cross-section diagram of the knee
Assessment
Back to contentsFor guidance on examination of the knee, see also the separate Knee Pain article.
Magnetic resonance imaging (MRI) is the technique of choice for evaluating internal derangement of the knee since even serious internal derangements of the knee may not be demonstrated on X-rays.1
The Ottawa Knee Rules can be used to decide whether an X-ray is indicated. An X-ray should be performed if any of the following are present:2
Inability to bear weight, both immediately and during the consultation, for four steps (inability to transfer weight twice on to each lower limb regardless of limping).
Inability to flex the knee to 90°.
Tenderness of the head of the fibula.
Isolated tenderness of the patella (no bone tenderness of the knee other than the patella).
Age 55 years or older.
Either offer an X-ray of the knee or offer referral to the A&E department for an X-ray (depending on availability of X-ray). In addition, offer an X-ray of the knee if knee swelling occurs following acute trauma.
Incidental meniscal findings on MRI scan of the knee are common in the general population and increase with increasing age: in one study of almost 1,000 people, 61% had meniscal tears on MRI but had no knee symptoms in the previous month.3
Delayed, gadolinium-enhanced MRI of cartilage (dGEMRIC) is useful for assessing cartilage health.4
Continue reading below
Meniscal tears
Back to contentsThe two menisci in each knee are crescent-shaped pads of cartilage tissue. The main functions of the menisci are tibiofemoral load transmission, shock absorption, lubrication of the knee joint and to improve the stability of the knee joint.
Meniscal root tears are radial tears located within 1 cm from the meniscal attachment or a bony root avulsion. This injury is biomechanically comparable to a total meniscectomy, resulting in decreased tibiofemoral contact area and increased contact pressures in the involved compartment.5
Epidemiology6
The incidence of meniscal injuries is increasing and this can be partly attributed to increased participation in sports as well as the recent advances and easy availability of imaging technology such as MRI.
A conservative estimate of the incidence of meniscal tears is 60 per 100,000, although the true incidence is likely to be grossly underestimated.
Mechanism of injury
The mechanism of injury is typically twisting or pivoting. Acute meniscal tears occur in young, active people. No or minimal force can be sufficient to cause a degenerative meniscal tear in middle-aged and older people.2
Meniscal tear symptoms and presentation
There may be acute pain, especially following obvious trauma or if a fragment of meniscus becomes trapped.
Often patients cannot remember the exact nature of an injury but complain of popping, catching, locking (usually in flexion) or buckling, along with joint line pain.7
There may be slow onset of swelling (over 2-36 hours) due to an effusion.2 Effusions can be recurrent.
If swelling is rapid in onset (0-2 hours) this may be due to a haemarthrosis or a large tense effusion when the tear is associated with a significant ligament injury.
Associated diseases
Meniscal tears are often associated with anterior cruciate ligament (ACL) injury (especially in younger patients) which should be identified.8 See the separate Knee Ligament Injuries article.
Meniscal tear treatment and management2
MRI continues to be the imaging modality of choice. Surgical management is the mainstay of treatment for meniscal tears.
Advise PRICER:
Protect from further injury.
Rest (crutches for the initial 24-48 hours).
Ice (application of ice on the injured region for 20 minutes of each waking hour during the initial 48 hours after injury).
Compression (with a knee brace or splint, if necessary).
Elevation (above the level of the heart).
Rehabilitation
An urgent referral to an orthopaedic surgeon is advised if the person has locking of the knee and a meniscal injury is suspected.
Refer to physiotherapy if there are mild-to-moderate symptoms. A physiotherapy regime will involve daily progressive exercises at home plus attendance at a physiotherapist.
Refer routinely to an orthopaedic surgeon if a meniscal injury is suspected, and symptoms interfere with the ability to work or persist, despite 6-8 weeks of rehabilitation by a physiotherapist.
Surgical options include repair or partial meniscectomy. Repair operations have better long-term outcomes, better activity levels and lower failure rates than meniscectomy (partial or total).9
Arthroscopic partial meniscectomy is currently the most performed orthopaedic procedure.6
However, although meniscectomy has long been considered the treatment of choice, a number of studies have reported no superiority of arthroscopy over non-operative treatment. Therefore non-operative treatment may be considered the first-line choice, with arthroscopic meniscectomy reserved for cases of failure of non-operative treatment, or earlier in the case of severe mechanical symptoms.10
For meniscal root tears, one systematic review found:11
In patients who experience meniscal root tears, meniscal repair may provide the greatest improvement in function and lowest risk of conversion to total knee arthroplasty when compared with partial meniscectomy or conservative methods.
Partial meniscectomy appeared to provide no benefit over conservative treatment, placing patients at a high risk of requiring total knee arthroplasty in the near future.
However it was also concluded that high-quality studies (comparative studies and randomised trials) are needed to draw further conclusions.
Meniscal allograft transplantation is a possible treatment option for patients with joint pain after meniscectomy.12
A novel treatment is the partial replacement of the meniscus using a biodegradable scaffold but it is uncertain whether this offers any long-term advantages over other options.13
Prognosis
Following partial or total meniscectomy, functional activities may be commenced on day 7-8 and running commenced from days 10-14, depending on the the underlying knee condition and health of the patient.
Rehabilitation protocols following meniscal repair vary.
Articular chondral and osteochondral injuries
Back to contentsThe articular surfaces of the femur and tibia are covered with hyaline cartilage. Damage to this hyaline cartilage is known as a chondral injury or, if the underlying bone is also fractured, an osteochondral injury.
Articular chondral and osteochondral injuries of the knee are much less common than meniscal injuries. They generally occur in people aged under 35 years, usually in combination with other ligamentous or meniscal injuries to the knee.
Mechanism of injury
Trauma is the most common mechanism; however, the repetitive stress associated with osteochondritis dissecans and with chondromalacia patellae is also the cause of symptomatic lesions.
Rotational force in direct trauma is the most common cause of injury to the articular cartilage. In most cases injury is in weight-bearing regions of articular cartilage and is usually in the medial compartment (four times more common that lateral injuries).14
Osteochondral lesions are most common in adolescents.
Articular cartilage has little capacity to repair itself or regenerate. Therefore, cartilage defects repair by forming scar tissue from the subchondral bone. This scar tissue is deficient in type II collagen and has lower load-bearing capacity. This later surface deterioration may progress to give chronic pain and poor function and may, in some cases, lead to early-onset osteoarthritis.
Presentation
Articular cartilage is avascular and aneural, so pain would not be expected; however, some patients do present with pain. It may be present at rest and is exacerbated by weight-bearing exercises.
The knee may give way if a long-standing injury results in substantial muscle wasting or there is associated ligamentous instability.
Locking is reported if a loose fragment impedes articular movement.
There may be an effusion.
Tenderness is found on palpation of the joint line, with pain induced both by passive and active movements.
Wasting of the quadriceps will be seen later on.
Crepitus is palpable on passive joint movement in a usually stable knee.
Associated diseases
Knee ligament injuries and fractures may also be present. Also meniscal injuries (see above).
Management
Lesions may not be diagnosed or may present late because patients will often give a history of an apparently insignificant trauma. Doctors may fail to understand the importance of an effusion in the knee joint, which always indicates joint disease.
Injuries that are new are given time to settle to see if the chondral lesion will become symptomatic or not. If pain fails to resolve after the initial acute phase, surgical treatment gives better outcomes if done sooner rather than later.
Conservative
Advise 'PRICER', as detailed under 'meniscal injuries', above.
After pain and inflammation subside, aim to increase strength and pain-free range of motion (ROM). Continuous passive motion enhances the healing potential of articular cartilage:15
It enables the movement of synovial fluid, allowing better diffusion of nutrients into the damaged cartilage and diffusion out of other materials (such as blood and metabolic waste products).
It reduces the formation of fibrous scar tissue in the joint; this tends to decrease ROM for a joint, which enhances the healing potential of articular cartilage.
Surgical
Treatment of larger and symptomatic lesions is surgical and techniques include arthroscopic debridement, marrow-stimulating techniques, such as microfracture, autologous chondrocyte transfers and implantation, and allografts.15 Microfracture is the most commonly used procedure and it is suggested that enhanced microfracture techniques may offer the best long-term outcomes; however, evidence is lacking.16
Return to the pre-injury level of sports has been found to be fastest after osteoarticular transplantation (OATS) and slowest after autologous chondrocyte implantation (ACI).17
Complications
If symptomatic lesions are untreated they may lead to chronic pain and disability and possible early osteoarthritis.
Significant soft tissue injuries of the knee and lower leg put the lower leg at risk for compartment syndrome.
Prognosis
Several factors have been associated with improved postoperative recovery:17
Defect size of less than 2 cm.
Pre-operative duration of symptoms of less than 18 months.
No previous surgical treatment.
Younger patient age.
Higher pre-injury level of sports.
However, no consensus exists on the most effective treatment and there are no long-term studies comparing the results of treatment with the natural history of the condition.18
In young adults, knee injury increases the risk of future diagnosed knee osteoarthritis about six-fold with highest risks found after cruciate ligament injury, meniscal tear and intra-articular fracture.19
Knees with known meniscal injury have accelerated cartilage wear, leading to early onset osteoarthritis. One study found that more than 75% of patients with symptomatic osteoarthritis have a meniscal injury.6
Further reading and references
- Sprains and strains; NICE CKS, April 2020 (UK access only)
- van de Graaf VA, Noorduyn JCA, Willigenburg NW, et al; Effect of Early Surgery vs Physical Therapy on Knee Function Among Patients With Nonobstructive Meniscal Tears: The ESCAPE Randomized Clinical Trial. JAMA. 2018 Oct 2;320(13):1328-1337. doi: 10.1001/jama.2018.13308.
- Beaufils P, Pujol N; Meniscal repair: Technique. Orthop Traumatol Surg Res. 2018 Feb;104(1S):S137-S145. doi: 10.1016/j.otsr.2017.04.016. Epub 2017 Nov 23.
- Teh J, Kambouroglou G, Newton J; Investigation of acute knee injury. BMJ 2012;344:e3167
- Knee pain - assessment; NICE CKS, Aug 2022 (UK access only)
- Englund M, Guermazi A, Gale D, et al; Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008 Sep 11;359(11):1108-15.
- Chang G, Sherman O, Madelin G, et al; MR imaging assessment of articular cartilage repair procedures. Magn Reson Imaging Clin N Am. 2011 May;19(2):323-37. doi: 10.1016/j.mric.2011.02.002.
- Pache S, Aman ZS, Kennedy M, et al; Meniscal Root Tears: Current Concepts Review. Arch Bone Jt Surg. 2018 Jul;6(4):250-259.
- Bhan K; Meniscal Tears: Current Understanding, Diagnosis, and Management. Cureus. 2020 Jun 13;12(6):e8590. doi: 10.7759/cureus.8590.
- Maffulli N, Longo UG, Campi S, et al; Meniscal tears. Open Access J Sports Med. 2010 Apr 26;1:45-54. eCollection 2010.
- Meniscii; Wheeless' Textbook of Orthopaedics
- Xu C, Zhao J; A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015 Jan;23(1):164-70. doi: 10.1007/s00167-013-2528-6. Epub 2013 May 14.
- Beaufils P, Pujol N; Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017 Dec;103(8S):S237-S244. doi: 10.1016/j.otsr.2017.08.003. Epub 2017 Sep 2.
- Stein JM, Yayac M, Conte EJ, et al; Treatment Outcomes of Meniscal Root Tears: A Systematic Review. Arthrosc Sports Med Rehabil. 2020 Apr 28;2(3):e251-e261. doi: 10.1016/j.asmr.2020.02.005. eCollection 2020 Jun.
- Young J, Tudor F, Mahmoud A, et al; Meniscal transplantation: procedures, outcomes, and rehabilitation. Orthop Res Rev. 2017 May 15;9:35-43. doi: 10.2147/ORR.S94378. eCollection 2017.
- Partial replacement of the meniscus of the knee using a biodegradable scaffold; NICE Interventional Procedure Guidance, July 2012
- Chondral and Osteochondral Injuries of the Knee; Wheeless' Textbook of Orthopaedics
- Macmull S, Skinner JA, Bentley G, et al; Treating articular cartilage injuries of the knee in young people. BMJ. 2010 Mar 5;340:c998. doi: 10.1136/bmj.c998.
- Bark S, Piontek T, Behrens P, et al; Enhanced microfracture techniques in cartilage knee surgery: Fact or fiction? World J Orthop. 2014 Sep 18;5(4):444-9. doi: 10.5312/wjo.v5.i4.444. eCollection 2014 Sep 18.
- Harris JD, Brophy RH, Siston RA, et al; Treatment of chondral defects in the athlete's knee. Arthroscopy. 2010 Jun;26(6):841-52.
- Vaquero J, Forriol F; Knee chondral injuries: clinical treatment strategies and experimental models. Injury. 2012 Jun;43(6):694-705. doi: 10.1016/j.injury.2011.06.033. Epub 2011 Jul 5.
- Snoeker B, Turkiewicz A, Magnusson K, et al; Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. Br J Sports Med. 2020 Jun;54(12):725-730. doi: 10.1136/bjsports-2019-100959. Epub 2019 Dec 11.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 15 Aug 2027
16 Aug 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free