Fibroids
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 16 Mar 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Periods and period problemsMissed periodsHeavy periodsPremenstrual syndromeHow to delay a periodEndometrial biopsy
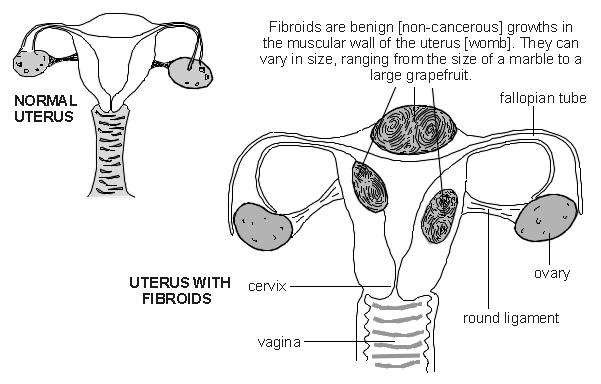
A fibroid is a non-cancerous (benign) growth of the womb (uterus). They are also called uterine myomas, fibromyomas or leiomyomas. Their size can vary. Some are the same size as a pea and some can be as big as a melon.
Fibroids are common and usually cause no symptoms. However, they can sometimes cause heavy periods, tummy (abdominal) swelling and urinary problems.
In this article:
Video picks for Uterine problems
What are fibroids?
Continue reading below
How common are fibroids?
Fibroids are common. It is difficult to know exactly how common they are as many women won't have any symptoms, and so may not know they have fibroids. Probably at least 1 in 2 women develop one or more fibroids in their lifetime, and probably more. They usually develop in women aged 30-50 and can sometimes run in families. It is common to have several fibroids of various sizes, although some women just have one.
Women from an Afro-Caribbean origin usually have a higher risk of developing fibroids. They also tend to be larger, occur at an earlier age and are more likely to cause symptoms in Afro-Caribbean women.
Fibroids are also more common in women who are overweight. This is thought to be due to the higher oestrogen levels that occur in obese and overweight women.
Fibroids can increase in size, decrease in size or even go away with time. They can occur anywhere in the womb and are named according to where they grow:
Intramural fibroids
These grow within the muscle tissue of the womb. This is the most common place for fibroids to form.
Subserous fibroids
These grow from the outside wall of the uterus (womb) into the pelvis.
Submucous fibroids
Subserosal fibroids grow from the inner wall into the cavity of the uterus.
Pedunculated fibroids
These grow from the wall of the uterus and are attached to it by a narrow stalk.
What do fibroids look like?
Back to contentsUterus showing fibroids
Continue reading below
Fibroid symptoms
Back to contentsMost women who have fibroids are not aware that they have them as they do not have any symptoms. Sometimes one is found during a routine examination (pelvic examination) by a doctor or by chance during a scan which you may have for another reason. Symptoms may include:
Heavy or more painful periods
Fibroids do not disturb the menstrual cycle but bleeding is often heavier than usual, sometimes with more pain. This can lead to low iron levels and to anaemia which will be diagnosed by a blood test. This is easily treated with iron tablets.
Bloating or swelling
If a fibroid is large you may have discomfort or swelling in the lower tummy (abdomen). Some women experience lower back pain due to their fibroids.
Bladder or bowel symptoms
Occasionally, a fibroid may press on the bladder which lies in front of the womb (uterus). You may then pass urine more often than usual. Rarely, pressure on the bowel (which lies behind the womb) may cause constipation.
Pain during sexual intercourse
If the fibroids grow near to the vagina or neck of the womb (cervix) then this can cause discomfort during sexual intercourse.
Miscarriage or infertility
If the fibroids grow into the cavity of the womb they can sometimes block the Fallopian tubes or interfere with implantation. This can cause problems conceiving, although this is not common. Very rarely, fibroids can be a cause of miscarriages.
Problems during pregnancy
Having one or more fibroids does not cause any problems in the vast majority of women when they are pregnant. Occasionally, you may have pain or discomfort from your fibroid. This may be caused by the fibroid growing too large for its blood supply or twisting, if the fibroid has a stalk (also called pedunculated).
However, fibroids can be associated with an increased risk of having a caesarean section, the baby lying bottom-first rather than head-first (breech) and early labour. Your doctor will advise you further if you are pregnant and have fibroids.
What causes fibroids?
Back to contentsA fibroid is an overgrowth of smooth muscle cells, and other cells from the lining of the womb (uterus). The womb is mainly made of smooth muscle. It is not clear why fibroids develop. Fibroids are sensitive to oestrogen and progesterone, the female hormones that are made in the ovary.
Fibroids tend to swell when levels of female hormones are high - for example, during pregnancy. They also shrink when levels are low - after the menopause. This shrinkage of the fibroids after the menopause may be delayed if you take hormone replacement therapy (HRT).
See the separate article called What's the link between hair relaxers and fibroids?
Do fibroids cause miscarriage?
Continue reading below
How are fibroids diagnosed?
Back to contentsSome fibroids can be felt during an internal (vaginal) examination by a doctor. Usually an ultrasound scan is done to confirm the diagnosis and to rule out other causes of any symptoms. If periods are heavy, a blood test would usually be done to check you are not anaemic.
Fibroid treatment
Back to contentsIf your fibroids are not causing any symptoms they do not usually require treatment. Many women choose not to have treatment if they have symptoms that are not too bad. After the menopause, fibroids often shrink and symptoms tend to go or ease. You can change your mind and consider treatment options if symptoms become worse. Your doctor may advise you to have a repeat scan to assess the growth and size of your fibroids.
Medication for fibroids
Back to contentsThe following medicines are used to treat heavy periods whatever the cause, including heavy periods that are caused by fibroids. Treating fibroids this way can help to ease symptoms. These medicines may not work so well if your fibroids are large. However, one or more of the following may be worth a try if your periods are heavy and the fibroids are small:
Tranexamic acid
This is taken 3-4 times a day, for the duration of each period. Tranexamic acid works by reducing the breakdown of blood clots in the womb (uterus).
Anti-inflammatory medicines
Medicines such as ibuprofen and mefenamic acid. Anti-inflammatory medicines also help to ease period pain. They are taken for a few days at the time of your period. They work by reducing the high level of a chemical (prostaglandin) in the lining of the womb. Prostaglandin seems to contribute to heavy and painful periods.
The combined oral contraceptive (COC) pill
The combined oral contraceptive (COC) pill may help you to have lighter periods and can often help with period pain too. If you are unable to take this, the progestogen-only contraceptive pill (POP) may help. Although there is little evidence for the POP, it seems to help, especially if it makes your periods lighter or stops them altogether.
The levonorgestrel intrauterine system (LNG-IUS)
This is a plastic device that sits inside the womb, originally used as a contraceptive. It is inserted into the womb and slowly releases a regular small amount of progestogen hormone called levonorgestrel. The levonorgestrel intrauterine system (LNG-IUS) works by making the lining of the womb very thin, so bleeding is lighter. However, it can sometimes be difficult to insert into the womb in women with fibroids.
Progestogen tablets
You can take progestogen tablets at certain times in your cycle or have the progestogen-only injection. The injection, usually used for contraception, tends to reduce or stop periods.
Medication to shrink the fibroids
Some women are given a gonadotrophin-releasing hormone (GnRH) analogue. This is a hormone medicine that causes you to have a very low level of oestrogen in your body. Fibroids shrink if the level of oestrogen falls. This can ease heavy periods and pressure symptoms due to fibroids.
However, a low oestrogen level can cause symptoms similar to going through the menopause (hot flushes, etc). It may also increase the risk factor of 'thinning' of the bones (osteoporosis). Therefore, this treatment is given for a maximum of six months.
GnRH analogues, such as goserelin or leuprorelin acetate, are often prescribed for three to four months before having an operation. This will make it easier to remove fibroids. Sometimes a low dose of HRT is also given to reduce the incidence of menopausal side-effects.
A medicine called ulipristal acetate (UPA) works by blocking the effects of the hormone progesterone. Progesterone is thought to play a role in fibroid development, so (by blocking progesterone) this medicine shrinks fibroids.
The National Institute for Health and Care Excellence (NICE) has recommended a combination drug called relugolix-estradiol-norethisterone acetate as an option for treating moderate to severe symptoms of uterine fibroids in adults of reproductive age.
Relugolix is a gonadotropin-releasing hormone (GnRH) receptor antagonist, so works like the medication above. This is then combined with the oestrogen, estradiol, to reduce symptoms related to lowered levels of oestrogen, and the progestogen, norethisterone, to counteract estradiol-induced thickening of the wall. This combination has been shown to work well in reducing bleeding. It also has other benefits such as:
Avoiding surgery. This preserves the uterus.
It can be taken orally.
It does not have many side-effects.
Other medication that work as GnRH antagonists, like the above, have recently been approved- it is best to talk to your specialist doctor about whether any of these are appropriate for you.
Surgery and other operative treatments
Back to contentsThere are several different operations available to remove and treat fibroids.
Hysterectomy
This is the traditional and most common type of treatment for fibroids which cause symptoms. Hysterectomy is the removal of the womb. This can be done by making a bikini line scar in the lower tummy (abdomen). Or, if the fibroids are small enough, the womb can be removed through keyhole (laparoscopic) surgery in the tummy, or through the vagina so there are no scars. A hysterectomy may be a good option for women who have completed their family.
Myomectomy
This is a possible alternative, especially in women who may wish to have children in the future. In this operation, the fibroids are removed and the womb is left. This procedure is not always possible. This operation can be done through a cut (incision) in the abdomen, via keyhole surgery (laparoscopically) or through the vagina (hysteroscopically).
The type of operation depends on the size, number and position of the fibroids. It is fairly common for a fibroid to occur again (recur) after a myomectomy. There is a risk of very heavy bleeding with this operation. Your surgeon should advise you that a hysterectomy may be needed if that situation arises.
Uterine artery embolisation
This procedure is done by a specially trained X-ray doctor (radiologist) rather than a surgeon. It involves putting a thin flexible tube (a catheter) into a blood vessel (artery) in the leg. It is guided, using X-ray pictures, to an artery in the womb that supplies the fibroid. Once there, a substance that blocks the artery is injected through the catheter. As the artery supplying the fibroid becomes blocked it means the fibroid loses its blood supply and so the fibroid shrinks.
The complete process of fibroid shrinkage takes about 6-9 months but most women notice a marked improvement in their symptoms within three months. There is a good chance of success with this procedure but nearly one in three women will need further treatment.
Myolysis
This means shrinking the fibroids in some way surgically. There are a number of ways of achieving this, including the following:
Endometrial ablation: this procedure involves removing the lining of the womb. This can be done by different methods - for example, using laser energy, a heated wire loop or by microwave heating. This method is usually only recommended for fibroids close to the inner lining of the womb. Treatment can be done either through a tube passed through the vagina, or can be guided through the skin by MRI scan.
MRI-guided focused ultrasound: this treatment sends pulses of high-power ultrasound through the skin of the lower abdomen. It is targeted at the fibroid, using the magnetic resonance (MRI) scanner. It is effective but there is no research yet on the long-term outcome for women trying to conceive.
Ultrasound-guided high-intensity focused ultrasound: this treatment is guided by ultrasound.
Morcellation for fibroids
Laparoscopic surgery with power morcellation allows uterine fibroids to be cut into smaller pieces. This allows them to be removed via keyhole surgery. Hysteroscopic morcellation aims to remove submucosal fibroids, using a telescopic instrument inserted into the womb through the vagina.
The National Institute for Health and Care Excellence (NICE) has looked at the risks and benefits of both procedures. They highlight the risk of possible serious complications with both procedures. Therefore they recommend that:
Power morcellation should not be used for women who are over 50 or postmenopausal.
For women under 50 or who have not gone through the menopause, power morcellation should not be carried out except in special circumstances.
Hysteroscopic morcellation should only be carried out in special circumstances.
You can read more about NICE's recommendations in the further reading section below.
See the separate leaflet called Menorrhagia Surgery for more information.
What are the complications of fibroids?
Back to contentsMany fibroids do not cause any health problems. However the possible complications of fibroids include:
Iron-deficiency anaemia due to heavy bleeding.
Large fibroids may push on the surrounding organs and pressure against the bladder may cause recurrent urinary tract infections (UTIs) or urinary retention.
Problems with fertility (this is rare).
Problems during pregnancy, including miscarriage or premature labour.
Twisting (torsion) of a fibroid may interfere with the blood supply to the fibroid and cause severe lower abdominal or pelvic pain.
What is the outcome (prognosis)?
Back to contentsThe outcome of fibroids is unpredictable. Fibroids tend to persist until the menopause when they usually shrink. Shrinkage may be limited by taking hormone replacement therapy (HRT). A few fibroids may shrink before the menopause.
Patient picks for Uterine problems

Women's health
Endometrial hyperplasia
Endometrial hyperplasia is a thickening of the womb (uterus) lining. The womb lining is called the endometrium. Hyperplasia means over ("hyper" in Latin) growth ("plasia" in Latin).
by Dr Philippa Vincent, MRCGP

Women's health
Endometriosis
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, usually in the pelvic area or lower tummy (abdomen). Its exact cause is unknown, but genetics, hormones, and the immune system may play a role. It affects those of the female sex, therefore, therefore the words woman/women and the pronouns she/her will be used throughout this leaflet. Endometriosis in trans men is discussed at the end of the leaflet.
by Dr Toni Hazell, MRCGP
Further reading and references
- Uterine artery embolisation for fibroids; NICE Interventional Procedures Guidance, November 2010
- Magnetic resonance image-guided transcutaneous focused ultrasound for uterine fibroids; NICE Interventional Procedures Guidance, November 2011
- Gupta JK, Sinha A, Lumsden MA, et al; Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database Syst Rev. 2014 Dec 26;12:CD005073. doi: 10.1002/14651858.CD005073.pub4.
- Lethaby A, Puscasiu L, Vollenhoven B; Preoperative medical therapy before surgery for uterine fibroids. Cochrane Database Syst Rev. 2017 Nov 15;11:CD000547. doi: 10.1002/14651858.CD000547.pub2.
- Murji A, Whitaker L, Chow TL, et al; Selective progesterone receptor modulators (SPRMs) for uterine fibroids. Cochrane Database Syst Rev. 2017 Apr 26;4:CD010770. doi: 10.1002/14651858.CD010770.pub2.
- Heavy menstrual bleeding: assessment and management; NICE Guideline (March 2018 - updated May 2021)
- Laparoscopic removal of uterine fibroids with power morcellation; NICE Interventional procedures guidance, August 2021
- Hysteroscopic mechanical tissue removal (hysteroscopic morcellation) for uterine fibroids; NICE Interventional procedures guidance, August 2021
- Relugolix–estradiol–norethisterone acetate for treating moderate to severe symptoms of uterine fibroids; NICE Technology appraisal guidance, October 2022
- Fibroids; NICE CKS, April 2023 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 7 Feb 2028
16 Mar 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.