Regarding diagnosis of digestive disorder
Posted , 9 users are following.
I am 27 years old male.
I have been suffering from digestion related issues since last 3 years.
Some key points that I would like to mention about my daily routine:
1. I work on laptop from my home (highly inactive lifestyle).
2. Have to take rest (sleep) 2-3 times in daytime as I feel tired, sluggish & lethargic till the sun sets. I feel quite fresh, active & energetic in evening & night.
I consulted with 3 doctors (Allopathic, Homeopathic & Ayurvedic) regarding the issue & all of them told me that it is IBS. But I suspect that it isn’t IBS & might be something more serious.
So, I researched about digestive disorders/diseases, went through their symptoms & made a list of symptoms that I have, I don’t have & I have no idea about. One thing I have observed that most of these symptoms are short lived. They appear for few days or weeks, then disappear & some other symptoms appear in their place.
There are almost 50 digestive diseases/disorders, all have nearly same symptoms & I think that accurate diagnosis is must in order to get right treatment & that’s why I have made a detailed list of symptoms.
I HAVE FOLLOWING SYMPTOMS:
1.Usually I have to go to the loo 3-4 times in the morning. Mostly I don’t feel need to defecate after morning but sometimes have to go in afternoon, evening or night as well.
Stool types & consistency:-
First time in the morning:
The faeces are sausage shaped, smooth & soft. Mostly brownish-yellow in color. Since I drink lukewarm water before going to the loo, some mushy stool also appears.
Second time in the morning:
Mostly loose motions. Sometimes stools have some form & are not too loose but sometimes it is watery.
Third time in the morning:
Usually I have to sit for long as I don’t get pressure to empty the bowels. Sometimes I have to put pressure to get the stools passed or defecation happens on its own after sitting for long time. This time usually defecation happens in the form of blobs & sometimes mucus or candida (some white stuff) appears with stools. Sometimes when I feel that I have passed stools & when I look into the bowl only mucus appears over there.
After meal or in evening:
Brown colored sticky stools which doesn’t float on water
2 Feeling of incomplete evacuation after defecating in the morning. (Usually I have to go to the loo 2-3 times in the morning to get the bowels completely emptied. But sometimes even after passing stools for 3-4 times, I just can’t clear the bowels completely)
3 Difficult & painful bowel movements (sometimes I have to sit for long to empty the bowels & sometimes even after sitting for long time if I am unable to pass stools, I have to put pressure to empty the bowels forcefully & this causes pain while passing stools. This happens usually 3rd or 4th time I go to the loo in the morning)
4 Change in frequency (ranging from 2-7 times a day) & consistency (sometimes a little bit watery stools, sometimes solid etc.) of bowel movements
5 Sometimes stools are narrow (not pencil width though)
6 Bright red blood in the stools (sometimes; it is occult or hidden blood sometimes)
7 Fat in stools (Sometimes I get to see faeces floating on water. Sometimes they seem to be greasy & sometimes drops of oil also are seen in the water inside the bowl. Though the faeces aren’t that pale or foul smelling.)
8 Some symptoms are alleviated by defecation
9 Dark urine (rarely). Its usually white when I drink enough of water
10 Abdominal pain (I feel some mild pain very rarely in the upper left abdomen at the place of spleen, usually for few seconds.
Had extremely severe abdominal pain one morning a few months back where I had eaten more than my capacity last night. I feel it happened because of trapped gas.)
11 Abdominal swelling/bloating (only if the bowels don’t get emptied completely.
A few months back used to suffer from bloating after sunset without eating anything or even after drinking small amounts of water. It doesn’t appear anymore.)
12 Used to feel full even after eating a fruit or drinking a glass of water at evening, a few months back. The situation has improved much now. But still at night I feel full earlier than I should be.
13 Sometimes I feel my abdomen to be stiff (not sensitive at all) on the left side of lower abdomen. I think this is what is called as abdominal rigidity or abdominal guarding
14 Growling stomach (very rarely; mostly at afternoon after lunch)
15 Very mild burning in stomach (very rarely)
16 Belching (used to belch a lot a few days back, now since I have reduced my meals, the situation has come under control, I belch but not that much)
17 Wind/gas. (Used to pass a lot of gas for a period of few days, a few weeks back. Now the situation has become normal.)
18 Mild pain in the rectum while passing gas (very rarely)
19 Poor appetite (might be because of my inactive lifestyle & sometimes incomplete evacuation)
20 Enlarged spleen (I feel so because of some symptoms)
21 Fatigue, Sluggishness & Lethargy (I don’t feel the same though when I am outing or at a function etc.). I feel completely fresh only when I take a lot of rest, say 4-5 hours in daytime.
22 I feel hungry & the food consumed gets digested properly when I am travelling or am outdoors. Inactive lifestyle worsens the symptoms.
23 Weight loss (I have lost weight but I think it is because I have reduced my diet.)
24 Presence of excess saliva or some bitter liquid in mouth (this might be acid reflux), usually at daytime (I think that is what causes bad breath)
25 Heartburn or acidity (only when sometimes I get up at mid night at around 2-3 AM)
26 Regurgitation of food (very rarely)
27 Headaches (very rarely; usually when I am not able to empty the bowels completely)
28 Joint pain (very rarely get pain in the wrist. I feel it happens because of trapped gas.
Used to have feeling of uneasiness in the ankle joints for a long period, don’t have any more.)
29 Neck & back pain (rarely; I feel it happens because of trapped gas)
30 Cramping (had experienced only for a period of a couple of days, a few weeks back & that too I felt was happening because of trapped gas in scrotum or area between anus & scrotum. I used to feel pain in the scrotum & it was little difficult for me to sit)
31 Mouth sores (mild)
32 Mild chills (sometimes)
33 Low-grade fever (very rarely)
34 Mimicking heart attack (had a couple of attacks like this which were not that severe. Might have happened because of gas)
35 Itchy, red hives on skin (occur rarely; it seems like they occur because of biting from insects.)
36 Lactose intolerance (experience symptoms sometimes after consuming milk based products)
37 Stress & worries to some extent
38 Stress causes aggravation of symptoms
39 Sensitivity to light and sound (to some extent)
I “DON’T” HAVE FOLLOWING SYMPTOMS:
1 Clay colored or tarry stools
2 Bloody diarrhoea
3 Bleeding during or after bowel movements
4 Pus drainage near the anal opening
5 Urgent need to defecate
6 Itchiness in the anal area
7 Discomfort while sitting
8 Rectal spasm
9 Pain or discomfort near the anus or buttocks
10 Feeling a bulge after coughing, sneezing or lifting
11 Feeling pressure in the rectum
12 Rectal fullness
13 Rectal prolapse
14 Redness, soreness of the skin around the anal opening
15 Rectal tenderness
16 Swelling around anus
17 Lump or painful hardened tissue or mass protruding near the anus
18 Visible tear or cut in the anus area
19 Levator ani syndrome
20 Passing excessive amounts of gas
(Used to suffer from this a few days back for a period of few days. The condition is normal now.)
21 Trouble passing gas
22 Incontinence
23 Inability to pass wind (Used to suffer from this a few weeks back, where the gas was moving from here & there inside body but wasn’t getting out. Not anymore.)
24 Abdominal tenderness
25 Abdominal cramps
26 Abdominal bleeding
27 Abdominal discomfort
28 Full, round abdomen
29 Increased abdominal size.
30 Lump or protrusion in the abdomen
31 Mass in the belly
32 Changes to the belly button
33 Difficulty belching
34 Less urine than normal
35 Inability to urinate
36 Urinary tract Infections
37 Kidney stones
38 Malaise
39 Swelling on any other body part than abdomen
40 Dizziness
41 Migraine
42 Fainting
43 Light-headedness
44 Used to get itchy red small boils on hand fingers, every summer a few years back. No more have these symptoms.
45 Vomiting
46 Fever
47 Feeling sick
48 Jaundice
49 Muscle pain (pain used to be there in the lats muscles. But disappeared after getting massage & taking rest.)
50 Fibromyalgia
51 Arthritis
52 Chest or shoulder pain
53 Pelvic pain
54 Lump or protrusion in the groin or scrotum
55 Groin discomfort or pain
56 Pain while coughing, bending or lifting a heavy object
57 Sleep disturbance
58 Night sweats
59 Cough
60 Feeling that something is stuck in your throat or chest
61 Choking during swallowing
62 Pain in the throat or chest during swallowing
63 Coughing during or after the swallow
64 Difficulty swallowing (suffered from little bit difficulty while swallowing for a period of few of days, felt it happened because of swollen tonsils.)
65 Trouble forming food and liquid into a soft ball in the mouth
66 Trouble pushing food or liquid to the back of the mouth
67 Throat irritation
68 Sore throat
69 Throat clearing
70 Hoarseness
71 Nasal regurgitation
72 Runny nose
73 Hiccups
74 Swelling or puffiness of the tissue directly under skin, especially in legs or arms.
75 Bone pain
76 Dehydration
77 Dry mouth, nostrils or skin
78 Not urinating as often
79 Fast heart rate
80 Shortness of breath
81 Difficulty breathing
82 Anorexia
83 Spider-like blood vessels
84 Bruising
85 Pain aggravated or relieved by meals
86 Burning or gnawing feeling similar to hunger pains
87 Red, purple, dark or discolored bulge
88 Stretched skin (but do have some strechmarks on some parts of the body)
89 Shiny skin (Used to be oily at teenage but became normal after taking treatment)
90 Skin that retains a dimple (pits), after being pressed for several seconds.
91 Weight gain
92 Increased salivation
I DON'T HAVE IDEA ABOUT FOLLOWING SYMPTOMS:
1 Decrease in caliber of stool
2 Osteoporosis (I feel my bones to be weak though & my posture is usually little bit stooped.)
3 Bumps or lumps on bones of legs, arms, skull and jaw
4 Infertility
5 Colitic arthritis, an arthritis that migrates along the body and affects knees, ankles, hips, wrists and elbows
6 Low blood count (anaemia) that makes you feel tired
7 Low blood pressure
8 Pericholangitis, inflammation of the tissues around the bile ducts
9 Malnutrition
10 Severe air swallowing
11 An enlarged bubble of gas in the stomach following heavy meals
12 Water-electrolyte imbalance
13 Teeth changing color or losing their enamel (My teeth always seem to be a little bit yellowish, no matter how properly I brush them.)
I consulted with a doctor & he said that it could be IBS+Anal fissure/Hemorrhoid. He prescribed me a few blood tests like CBC, Vitamin D3 & B12, LFT, Creatinine etc. & Anal manometry.
So, should I continue with his advise or seek for second opinion?
0 likes, 32 replies
stoneoakgi Aryan111
Posted
The various ailments of the gastrointestinal (GI) tract affect food digestion and absorption. Diagnosing them is critical to effective treatment and prevention of complications. Here are 11 diagnostic tests that help diagnose various GI disorders.
1. Clinical examination
The symptoms present and a physical examination may help diagnose a few GI disorders like diarrhoea, constipation, acidity, etc. For diseases like haemorrhoids, physical rectal examination may be done wherein the doctor inserts a gloved finger into the rectum to feel for abnormalities.
2. Blood test
Blood tests like blood count, liver function test, lactose tolerance test, antibodies to H. pylori, pancreatic enzyme test, etc. can help diagnose certain GI conditions like bacterial or parasitic infection, celiac disease, lactose intolerance, exact cause of diarrhoea, etc. They may also be recommended to rule out other serious diseases. The laboratory tests to determine liver efficiency include CBC (complete blood count), liver function tests (SGOT, bilirubin, alkaline phosphatise, etc.), blood albumin and prothrombin time.
3. Stool analysis
Stool analysis can help assess the overall health of GIT. It helps analyse digestion, absorption, microbial balance, etc.
This gastrointestinal test profile may be advised in conditions like indigestion, constipation, diarrhoea, IBS, malabsorption, infection, etc.
For the analysis, a stool sample collected in a clean container is sent to the laboratory for microscopic examination and other tests.
Changes in colour, consistency and pH, and the presence of mucus, blood, white blood cells, bile, fat, sugars, etc. help diagnose GI conditions. A stool culture can help diagnose bacterial infection. Increased fat levels in the stool may be seen in celiac disease, pancreatitis, etc. High pH of the stool could indicate inflammation, cancer, etc. Some enzyme immunoassays are used to detect viral and bacterial antigen in stool sample.
4. Renal function test
Gadolinium containing contrast agents, most commonly used in MRI and CT scans, are avoided in patients with reduced kidney function or kidney failure. Hence, kidney function tests are done prior to MRI or CT scans of GIT.
5. Endoscopy
Long-standing acidity, heartburn, unexplained weight loss and changes in bowel pattern may need a detailed investigation of the intestine. Endoscopy is a non-surgical procedure that involves examination of the stomach or digestive tract with the help of an instrument called endoscope. Biopsies (small tissue sample) may also be taken during endoscopy to be examined under microscope. They can help detect presence of cancerous cells.
During colonoscopy, a tube is inserted through the anus to visualise the colon. It aids in detection for areas of inflammation or small ulcers in the colon. Proctoscopy can help visualise the rectum.
In case of a tumour in the intestine, an ultrasound followed by endoscopy, imaging, scans, etc. of the upper intestine is done to study the nature of the growth. An endoscopy ultrasound (EUS) can help make an accurate diagnosis without having the need to undergo several tests.
In endoscopic retrograde cholangiopancreatography (ERCP), the inside of the stomach and duodenum is seen through an endoscope, and radiographic contrast which can be seen on X-rays is injected into the ducts and pancreas. The test helps confirm gall stones.
In video capsule endoscopy, a swallowed capsule containing a tiny video camera travels through the small intestine and sends video images of the lining of the small intestine that are downloaded and studied on a computer. This test is superior in identifying the early stages of Crohn’s disease.
Narrow band imaging is a novel endoscopic technique which can be incorporated during gastroscopy especially if there is a lesion suspected to be malignant or pre-malignant. It uses special filters and magnifying methods to diagnose early cancerous or pre-cancerous lesions.
6. Abdominal ultrasound, CT scan and MRI
An ultrasound is a diagnostic medical procedure that uses high frequency sound waves to produce dynamic (or real-time) images of internal organs, tissue and blood vessels. Abdominal ultrasound is used to examine organs and their blood vessels in the abdomen like liver, pancreas, gallbladder, etc.
Computerized topography (CT) scan is a computerised X-ray technique that combines a large number of X-ray images taken in succession. These images then result in a cross sectional view of the internal organs which helps analyse the internal structures of the body. It can be used to examine the GIT for diagnosing traumatic injuries, tumours or an infection.
In magnetic resonance imaging (MRI), a beam of radio waves and magnetic fields is sent through the body to detect a defect in the organ of interest. It gives an accurate image of the organ and structures within, thus helping in getting a clear idea of cancerous cells and the extent of the growth.
7. Barium X-ray
In barium X-ray, a chalky liquid called barium is used which is visible on an X-ray. When ingested, the barium can help view the stomach and the small intestines on an X-ray. When administered rectally as enema, the colon and terminal ileum can be viewed on X-ray. This test helps diagnose gut narrowing, fistulae, ulcerations, etc.
8. Manometry
Manometry uses a device called a manometer to measure muscle pressure and movement. Oesophageal manometry measures the symmetrical contraction and relaxation (peristalsis) of oesophagus and relaxation of lower oesophagal sphincter in the evaluation of achalasia. The lack of oesophagal peristalsis and failure of the LES to relax during swallowing is disclosed during this test. Anorectal manometry is used to measure contractility of the anal sphincter to evaluate anal incompetence and faecal incontinence.
9. pH Monitoring
Esophageal pH monitoring measures the amount of stomach acid that enters the oesophagus during a 24-hour period. It is used to diagnose GERD. It also helps determine the effectiveness of the prescribed medications. During the test, a thin tube with a sensor is passed through the nose and positioned in the oesophagus just above the lower oesophageal sphincter that is present at the junction of the oesophagus and stomach. The acid level in the oesophagus is recorded on a monitor. The data gathered in 24 hours is downloaded into a computer and analysed. A wireless capsule that is placed using an endoscope may be used instead of the tube. It sends recordings through wireless transmission.
10. Breath Test
The hydrogen breath test measures hydrogen in the breath to diagnose GI conditions like lactose intolerance, etc. When ingested sugars are not completely absorbed by the small intestine, bacteria within the colon produce hydrogen gas. Bacterial overgrowth in the small intestine can also produce large amounts of hydrogen. Hydrogen gas absorbed into the blood travels to the lungs. The test analyses the breath at regular intervals to detect this hydrogen gas that is breathed out. The patient will be asked to breath before drinking milk and then samples are taken after fixed intervals to determine hydrogen levels in your breath. If you are lactose intolerant, breath levels of hydrogen will be high as compared to normal levels.
Urea breath test helps diagnose peptic ulcer. The test looks for presence of Helicobacter pylori bacteria in the stomach. Normally, the body produces urea from excess nitrogen-containing chemicals and eliminates it in the urine. H. pylori bacteria breaks down urea into ammonia and carbon dioxide. Carbon dioxide thus produced is absorbed from the stomach and exhaled. During the urea breath test a urea tablet containing radioactive carbon is swallowed. Presence of radioactive carbon dioxide in the exhaled air indicates the presence of H. pylori bacteria.
11. Transient Elastography
Diseased livers are stiffer than healthy ones. Transient elastography is a non-invasive test that records the elastic properties of liver and helps quantify liver fibrosis. During the test, a small transducer passes 50-MHz wave into the liver through a probe. The velocity of the shear wave (in meters/second) as it passes through the liver is measured. The measurement is then converted into liver stiffness (in kilopascals).
Aryan111 stoneoakgi
Posted
Aryan111
Posted
Hi guys! Received the biopsy report a few hours back. Have an appointment with Gastroenterologist after two days. Was eager to get to know what is mentioned in the report. I could not understand the meaning of "GROSS" & "MICROSCOPY" section of the report. If anybody understands it, please comment. Here is the report:
DIAGNOSIS :
Moderate colitis; likely infective origin.
CLINICAL DETAILS :
Increased stool frequency with fecal red blood cells.
Colonoscopy - Multiple patchy ulcers from rectum to hepatic flexure.
Impression : Infective colitis.
GROSS :
Received multiple grey-white mucosal tissue bits aggregating to 1.0 x 0.7 x 0.2 cm; Colonic ulcer biopsy.
Sections : A to D.
MICROSCOPY :
Sections show ulcerated colonic mucosa with presence of neutrophils in the lining epithelium. Lamina propria shows
moderate mixed inflammatory infiltrate consisting of neutrophils, lymphocytes, plasma cells, and a few eosinophils.
There is no cryptitis, crypt abscess or crypt distortion seen. There is no evidence of granulomas or dysplasia seen. No
parasites evident.
Aryan111
Posted
Hi guys! I consulted with the gastroenterologist yesterday. After reading the report he said that infection is most likely the reason for ulcerations seen in the colonic mucosa. He said that he can't tell how long will it take to get cured. He also thought depression or my too much of thinking might be the reason behind my stomach not getting emptied properly or the reason might be a component of IBS & prescribed me an anti-depressant. He told me to not even think about the issue I am suffering from. He advised me to continue with normal diet and also advised to do some Yoga & exercise. He told me not to have protein powder as well as mass gainer as of now.
I am thinking of taking second opinion. I request you to guide me whether I should continue with his advise or go for second opinion.
pippa58442 Aryan111
Posted
Aryan111 pippa58442
Posted
Now I also think that I should accept the diagnosis. BTW this doc doesn't like to spend much time with patients or take efforts to explain the report. He just prescribes the medicines & don't talk much. That's why I had to ask this over here on forums. Anyways, thanks once again for commenting
pippa58442 Aryan111
Posted
Aryan111
Posted
Guys, I got stool test done twice. First time I had given reddish sample for test but it didn't show presence of any blood in the report. So I got it done again. This time as well the report stated no presence of blood (though I still get to see bright red blood stuck to the stool sometimes). The only abnormal thing was that it showed the stool be acidic to which the doctor said that it doesn't matter much.
Mentioning my current symptoms below:
1. I don’t feel fresh & energetic when I wake up even though I sleep for 8+ hours.
2. I have to go to the loo at least 3 times a day & sometimes even after passing stools for 3-4 times in the morning itself, I don’t get the feeling of completion. It feels like I empty the bowels in parts (I mean it doesn’t get emptied in single attempt). Usually third time onwards, I have to sit for long as I don’t get pressure to empty the bowels. Sometimes I have to put pressure to get the stools passed or defecation happens on its own after sitting for long time.
3. The stool is mushy almost all the times. As far as I know mushy stool suggests mild diarrhoea & I think because of this dehydration happens which makes me feel exhausted (tired & sluggish). I have to sleep then as I don’t feel fresh & can’t concentrate on work. It takes me around 4 hours to get ready to kick start the day.
4. I get to see small amount of bright red blood stuck to the stool sometimes.
5. A lot of belching happens when I do simple exercise like warm up.
6. I have to go to the loo when I wake up if I sleep after lunch in afternoon.
7. I mostly feel full in the evening time even if I haven’t eaten/drunk anything or eat/drink only in small amounts. So I mostly skip snacks.
8. Have got 2 attacks of severe abdominal pain in the lower left abdomen till now.
9. Mouth sores (mild)
10. I feel hungry & the food consumed gets digested properly when I am travelling or am outdoors.
The doctor has prescribed me to get anal manometry done now. I would like to have your opinion on whether should I get manometry done or seek for second opinion.
Thanks in advance
pippa58442 Aryan111
Posted
Aryan111 pippa58442
Posted
pippa58442 Aryan111
Posted
👍
Aryan111
Posted
Hi guys! As advised by the gastroenterologist, I got anorectal manometry done. The doctor who did the procedure told me that I contract the anal muscles instead of relaxing while having bowel movement, this causes incomplete evacuation & that is why I have to pass the stools several (usually 4-5) times a day.
Below are the findings of the report:
Anal sphincter length is approximately 4 cm (shorter than the normal length I guess)
Rectoanal inhibitory reflex [RAIR] is present.
On bearing down he paradoxically contracts his anal sphincter instead of relaxing it and has poor rectal propulsive forces [<40mmHg] which is suggestive of "Dyssynergic defecation". He is unable to expel a 50cc balloon in 60 secs. Biofeedback sessions for anal sphincter relaxation exercises maybe beneficial.
(Attaching the report).
The doctor has advised me to go for biofeedback. I googled a bit & found that biofeedback is the most effective treatment method for dyssynergic defecation but from a survey on patientslikeme I found that this treatment method isn't that effective instead people got benefited from a method like physical therapy.
Have got a few questions now:
I. Is it only the dyssynergic defecation which causes me to have 4-5 bowel movements daily, poor apetite etc or something else like IBS as well is present?
II. What is the reason of blood being seen stuck to the stool (sometimes)? Is it Infectious colitis or dyssynergic defection or something mild like anal fissure?
III. Shall I go for biofeedback or try something else like physical therapy?
Kindly guide me. Thanks in advance.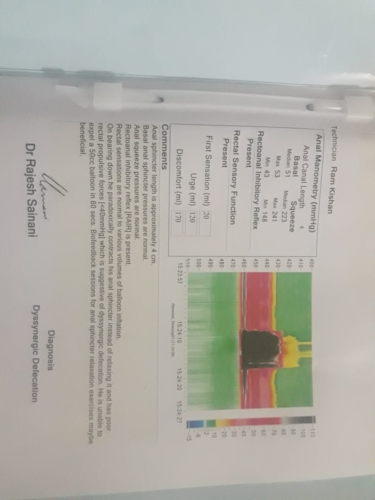
pippa58442 Aryan111
Posted
Accept your tests results and your doctor's advice and try biofeedback. The only way of knowing if it works for you is to try it. Everyone is different. Your experience may be different from others. Don't bog yourself down with too many options.