Trauma triage and scoring
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Laurence KnottLast updated 17 Aug 2021
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
For advanced adult trauma life support (ATLS), see the separate Trauma Assessment article.
Continue reading below
Trauma triage1
Trauma triage is the use of trauma assessment for prioritising of patients for treatment or transport according to their severity of injury. Primary triage is carried out at the scene of an accident and secondary triage at the casualty clearing station at the site of a major incident. Triage is repeated prior to transport away from the scene and again at the receiving hospital.
The primary survey aims to identify and immediately treat life-threatening injuries and is based on the 'ABCDE' resuscitation system:
Airway control with stabilisation of the cervical spine*.
Breathing.
Circulation (including the control of external haemorrhage).
Disability or neurological status.
Exposure or undressing of the patient while also protecting the patient from hypothermia.
*A growing body of evidence indicates the need to reconsider the routine use of cervical collars and rigid backboards in pre-hospital trauma care2 .
Priority is then given to patients most likely to deteriorate clinically and triage takes account of vital signs, pre-hospital clinical course, mechanism of injury and other medical conditions.Triage is a dynamic process and patients should be reassessed frequently. The following is one example of triage sieve which is used in the UK3 :
Priority 1 (P1) or Triage 1 (T1): immediate care needed - requires immediate life-saving intervention. Colour code red.
P2 or T2: intermediate or urgent care needed - requires significant intervention within two to four hours. Colour code yellow.
P3 or T3: delayed care - needs medical treatment but this can safely be delayed. Colour code green.
Dead is a fourth classification and is important to prevent the expenditure of limited resources on those who are beyond help. Colour code black.
The 'P' prefix is used by civilian services and the 'T' prefix by the military.
The cABCDE system has been used in the military for a number of years - the initial 'c' standing for catastrophic haemorrhage. This arose from the finding that many lives could be saved by giving the control of haemorrhage and correction of hypovolaemia pre-eminence over airways control and other resuscitative measures4 .
Triage systems are most often used following trauma incidents but may be required in other situations, such as an influenza epidemic5 . The need for effective triage systems to inform the use of intensive care resources was particularly highlighted during the COVID-19 pandemic6 . Once further resources are available to hand, the patients will undergo a further, more detailed triage based on vital signs - eg, respiratory rate. One such score is called the Revised Trauma Score (see below).
Additional patient triage
Following the initial triage, there is usually a further detailed pre-hospital triage of patients. The following is one example:
Triage sieve
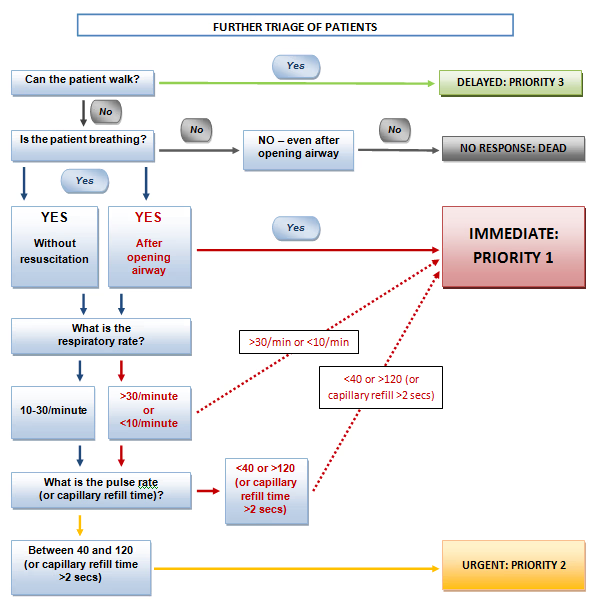
Modified sieve systems are available for use in children.
Trauma scoring
Trauma scores are often audit and research tools used to study the outcomes of trauma and trauma care, rather than predicting the outcome for individual patients. Many different scoring systems have been developed; some are based on physiological scores (eg, Glasgow Coma Scale (GCS)) and other systems rely on anatomical description (eg, Abbreviated Injury Scale (AIS)). There is, however, no universally accepted scoring system and each system has its own limitations.
The triage sort or Revised Trauma Score (RTS)7
Used as a triage tool in a pre-hospital setting.
It is a common physiological scoring system based on the first data sets of three specific physiological parameters obtained from the patient.
The three parameters are: the GCS, systemic blood pressure (SBP), and the respiratory rate (RR).
Limitations
These include the inability to accurately score patients who are intubated and mechanically ventilated.
Physiological variable | Value | Score |
Respiratory rate | 10-29 | 4 |
| >29 | 3 |
| 6-9 | 2 |
| 1-5 | 1 |
| 0 | 0 |
Systolic blood pressure | >90 | 4 |
| 76-89 | 3 |
| 50-75 | 2 |
| 1-49 | 1 |
| 0 | 0 |
Glasgow Coma Scale (GCS) | 13-15 | 4 |
| 9-12 | 3 |
| 6-8 | 2 |
| 4-5 | 1 |
| 3 | 0 |
A total score of 1-10 indicates priority T1, 11 indicates T2, and 12 indicates T3. A score of 0 means dead.
A comparison of the Modified Early Warning Score (MEWS) and RTS showed that MEWS had a better predictive efficacy.
Continue reading below
Anatomical scoring systems
Abbreviated Injury Scale (AIS)8
Since its introduction as an anatomical scoring system in 1969, the AIS has been revised and updated many times.
The AIS scale is similar to the Organ Injury Scale (OIS) introduced by the Organ Injury Scaling Committee of the American Association for the Surgery of Trauma; however, AIS is designed to reflect the impact of a particular organ injury on patient outcome.
The Association for the Advancement of Automotive Medicine monitors the scale.
Injury Threat | AIS Score |
Minor | 1 |
Moderate | 2 |
Serious | 3 |
Severe | 4 |
Critical | 5 |
Unsurvivable | 6 |
Limitations
The AIS scale does not provide a comprehensive measure of severity.
The AIS scale does not represent a linear scale, ie the difference between AIS1 and AIS2 is not the same as the difference between AIS4 and AIS5.
When used alone, the current AIS version is not useful for predicting patient outcomes or mortality; instead, it forms the basis of the Injury Severity Score (ISS) and the Trauma and Injury Severity Score (TRISS).
Injury Severity Score (ISS) and New Injury Severity Score (NISS)8
The ISS was introduced in 1974 as a method for describing patients with multiple injuries and evaluating emergency care. It has since been classed as the 'gold standard' of severity scoring.
Each injury is initially assigned an AIS score and one of six body regions (head, face, chest, abdomen, extremities, external).
The highest three AIS scores (only one from each body region may be included) are squared and the ISS is the sum of these scores.
Limitations
Inaccurate AIS scores are carried forward.
Many different injury patterns can yield similar ISS scores.
It is not useful as a triage tool9 .
It only considers one injury per body region and therefore may underestimate the severity in trauma victims with multiple injuries affecting one body part10 .
The NISS is a modified version of the ISS developed in 1997. The NISS sums the severity score for the top three AIS injuries regardless of the body region; hence, NISS scores greater than ISS values indicate multiple injuries in at least one body region11 .
Organ Injury Scale (OIS)
This scale provides a classification of injury severity scores for individual organs.
The OIS is based on injury description scaled by values from 1 to 5, representing the least to the most severe injury.
The Organ Injury Scaling Committee of the American Association for the Surgery of Trauma (AAST) developed the OIS in 1987; the scoring system has been updated and modified since that time12 .
Physiological scoring systems
Glasgow Coma Scale (GCS) and Glasgow Paediatric Coma Scale (GPCS)
The GCS and the GPCS are simple and common methods for quantifying the level of consciousness following traumatic brain injury.
The scale is the sum of three parameters:
Best Eye Response
Best Verbal Response
Best Motor Response
Scales are based on values ranging between 3 (worst) to 15 (best)1 .
The Acute Physiology and Chronic Health Evaluation (APACHE)
APACHE was first introduced in 1981. APACHE IV is an updated version introduced in 2006.
This evaluation system is used widely for the assessment of illness severity in intensive care units (ICUs)13 .
Continue reading below
Combination scoring systems
Trauma and Injury Severity Score (TRISS)8
This score determines the probability of patient survival (Ps) from the combination of both anatomical and physiological (Injury Severity Score (ISS) and Revised Trauma Score (RTS), respectively) scores. A logarithmic regression equation is used:
Ps = 1/(1+e-b), where b = bo + b1 (RTS) + b2 (ISS) + b3 (Age Score)14
RTS and ISS are calculated as above and Age Score is either 0 if the patient is <55 years old or 1 if aged 55 and over. The coefficients b0-b3 depend on the type of trauma (NB: there is some variation in the published values for these). A TRISS calculator is available on the internet15 .
Coefficient | Blunt trauma or age <15 years | Penetrating trauma |
b0 | -0.4499 | -2.5355 |
b1 | 0.8085 | 0.9934 |
b2 | -0.0835 | -0.0651 |
b3 | -1.7430 | -1.1360 |
Future directions
Trauma triage and scoring is an ongoing development in process and new systems are being optimised on a daily basis.
Lactate measures may become more important in future. It is a better predictor of blood transfusion need and mortality16 .
Further reading and references
- Planas JH, Waseem M, Sigmon DF; Trauma Primary Survey
- Zileli M, Osorio-Fonseca E, Konovalov N, et al; Early Management of Cervical Spine Trauma: WFNS Spine Committee Recommendations. Neurospine. 2020 Dec;17(4):710-722. doi: 10.14245/ns.2040282.141. Epub 2020 Dec 31.
- Triage in Mass Casualty Situations; Royal College of Emergency Medicine, 2020
- Reed RC, Bourn S; Prehospital emergency medicine - UK military experience. BJA Educ. 2018 Jun;18(6):185-190. doi: 10.1016/j.bjae.2018.03.003. Epub 2018 Mar 28.
- Talmor D, Jones AE, Rubinson L, et al; Simple triage scoring system predicting death and the need for critical care resources for use during epidemics. Crit Care Med. 2007 May;35(5):1251-6.
- Fiest KM, Krewulak KD, Plotnikoff KM, et al; Allocation of intensive care resources during an infectious disease outbreak: a rapid review to inform practice. BMC Med. 2020 Dec 18;18(1):404. doi: 10.1186/s12916-020-01871-9.
- Yu Z, Xu F, Chen D; Predictive value of Modified Early Warning Score (MEWS) and Revised Trauma Score (RTS) for the short-term prognosis of emergency trauma patients: a retrospective study. BMJ Open. 2021 Mar 15;11(3):e041882. doi: 10.1136/bmjopen-2020-041882.
- The Trauma Audit and Research Network: Procedures manual England & Wales; TARN, January 2021
- Paffrath T, Lefering R, Flohe S; How to define severely injured patients?-An Injury Severity Score (ISS) based approach alone is not sufficient. Injury. 2014 Oct;45 Suppl 3:S64-9. doi: 10.1016/j.injury.2014.08.020.
- Husum H, Strada G; Injury Severity Score versus New Injury Severity Score for penetrating injuries. Prehosp Disaster Med. 2002 Jan-Mar;17(1):27-32.
- Eid HO, Abu-Zidan FM; New Injury Severity Score Is a Better Predictor of Mortality for Blunt Trauma Patients Than the Injury Severity Score. World J Surg. 2014 Sep 5.
- The American Association for the Surgery of Trauma; Injury Scoring Scale, A Resource for Trauma Care Professionals, 2021.
- Salluh JI, Soares M; ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care. 2014 Oct;20(5):557-65. doi: 10.1097/MCC.0000000000000135.
- Honarpisheh H; A comprehensive model for trauma research design. Arch Trauma Res. 2012 Spring;1(1):3-13. doi: 10.5812/atr.5288. Epub 2012 Jun 1.
- TRISS: Trauma Injury Severity Score; Trauma Service, 2021
- Lewis CT, Naumann DN, Crombie N, et al; Prehospital point-of-care lactate following trauma: A systematic review. J Trauma Acute Care Surg. 2016 Oct;81(4):748-55. doi: 10.1097/TA.0000000000001192.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 5 Aug 2026
17 Aug 2021 | Latest version

Feeling unwell?
Assess your symptoms online for free