Hepatitis B
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Laurence KnottLast updated 24 Mar 2022
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Hepatitis B article more useful, or one of our other health articles.
In this article:
This is a notifiable disease in the UK. See the Notifiable Diseases article for more detail.
Continue reading below
What is hepatitis B?
Hepatitis B is an infection of the liver caused by the hepatitis B virus (HBV), a double-stranded DNA virus which replicates by reverse transcription (Hepadnaviridae family).
Mutations of the surface coat protein, core and other proteins have been identified.1
How common is hepatitis B? (Epidemiology)
The World Health Organization (WHO) has estimated that over 296 million people worldwide were chronically infected with HBV in 2019.2
Worldwide, hepatitis B is the most common cause of hepatitis.
In many high-prevalence countries, 10% or more of the population have chronic hepatitis B infection.
High-prevalence regions include sub-Saharan Africa, most of Asia and the Pacific islands.
In the UK around 1 person in 350 is thought to have chronic hepatitis B infection.
The greatest decline has happened among children and adolescents, due to routine hepatitis B vaccination.
Note: most reports of acute infection in the UK occur as a result of injecting drug use or sexual exposure.
Continue reading below
Hepatitis B symptoms3
Many new infections with hepatitis B are subclinical or may have a flu-like illness.
The incubation period ranges from 40 to 160 days, with an average of 60 to 90 days.
Jaundice only occurs in about 10% of younger children and in 30-50% of adults.
Acute infection may occasionally lead to fulminant hepatic necrosis, which is often fatal.
The illness usually starts insidiously - with anorexia and nausea and an ache in the right upper abdomen.
Fever, when present, is usually mild.
Malaise may be profound, with disinclination to smoke or to drink alcohol.
As jaundice develops, there is progressive darkening of the urine and lightening of the faeces.
The presentation of decompensated liver disease include ascites, encephalopathy and gastrointestinal haemorrhage.
What is chronic hepatitis B?
Chronic hepatitis B is a spectrum of disease usually characterised by the presence of detectable hepatitis B surface antigen (HBsAg) in the blood or serum for longer than six months. Chronic hepatitis B may be inactive and cause no significant health problems but may progress to liver fibrosis, cirrhosis and hepatocellular carcinoma. The progression of liver disease is associated with HBV DNA levels in the blood.
Chronic hepatitis B can be divided into e antigen (HBeAg)-positive or HBeAg-negative disease based on the presence or absence of e antigen. The presence of HBeAg is associated with higher rates of viral replication and therefore increased infectivity.
Although many patients with chronic hepatitis B are healthy carriers, some patients do have symptoms. These include fatigue, anorexia and nausea and right upper quadrant pain.
The risk of developing chronic hepatitis B infection depends on the age at which infection is acquired; the risk is lowest in adults and >90% in neonates whose mothers are HBeAg-positive.4
Chronic infection is less frequent in those infected as children.
The risk of becoming chronically infected with hepatitis B is increased in those whose immunity is impaired.
Approximately 25% of adults who become chronically infected during childhood later die from HBV-related liver cancer or cirrhosis.
The risk of progression is related to the level of active viral replication in the liver.
People with chronic hepatitis B infection (particularly those with an active inflammation and/or cirrhosis, where there is rapid cell turnover) are at increased risk of developing hepatocellular carcinoma (HCC).
Chronic hepatitis B infection usually has a benign course in healthy non-drinkers with normal liver function.
Continue reading below
Route of hepatitis B transmission
The virus is transmitted by parenteral route via infected blood or body fluids. The following are the most common ways of transmitting infection:
Through vaginal or anal intercourse. As a result of blood-to-blood contact (eg, sharing of needles and other equipment by injecting drug users, or 'needlestick' injuries).
Transfusion-associated infection is now rare in the UK, as blood transfusions and donations are carefully screened. Viral inactivation of blood products has eliminated these as a source of infection in this country.
Vertical transmission (mother to infant) of infection occurs in 90% of pregnancies where the mother is HBeAg-positive and in about 10% of hepatitis B surface antigen (HBsAg)-positive, HBeAg-negative mothers.
Transmission has also followed bites from infected persons, although this is rare.
In areas of high prevalence, infection is acquired predominantly in childhood - by perinatal transmission or by horizontal transmission among young children.
In low-endemicity countries most infections are acquired in adulthood, where sexual transmission or sharing of blood-contaminated needles and equipment by injecting drug users accounts for a significant proportion of new infections.
Investigations5 6
The following investigations are usually performed under specialist care:
Investigations related to hepatitis B
HBsAg, HBeAg, anti-HBe, anti-HBs, anti-HB core.
Quantitative hepatitis B virus DNA.
HBV genotype (for those considered for interferon).
Hepatitis delta virus (HDV) serology.
General liver investigations
FBC.
Bilirubin.
Liver enzymes.
Clotting.
Ferritin.
Lipid profile.
Autoantibody screen.
Caeruloplasmin.
Tests for hepatitis C virus (HCV) and HIV
Screening for liver cancer.
Ultrasonography.
Alpha-fetoprotein.
Staging of disease in secondary care
This includes:
Transient elastography, which is non-invasive and has a high diagnostic accuracy for the detection of cirrhosis, although the results may be confounded by severe inflammation associated with high alanine aminotransferase (ALT) levels and the optimal cut-off of liver stiffness measurements varying among studies.7
Liver biopsy. This continues to play an important role in providing information on the aetiology and severity of liver disease.5
Serological markers
Hepatitis B
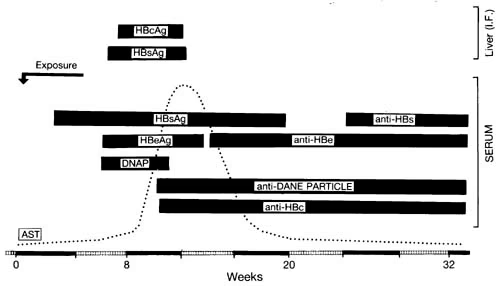
HBsAg is the only serological marker detected during the first 3-5 weeks after being infected.
The mean time from exposure to detection of HBsAg is 30 days.
The persistence of HBsAg for >6 months defines carrier status. This follows 5-10% of infections:
Among those who are HBsAg-positive, those in whom HBeAg is also detected in the serum are the most infectious.
Those who are HBsAg-positive and HBeAg-negative (usually anti-HBe-positive) are infectious but generally of lower infectivity.
The presence of HBeAg implies high infectivity. HBeAg is usually present for 1½-3 months after the acute illness.
Antibodies to hepatitis B core antigen (HBcAg) - ie anti-HBc - imply past infection.
Antibodies to HBsAg - ie anti-HBs - alone imply vaccination.
Dane particles are HBV virions. Anti-Dane particles are antibodies formed against them.
DNAP is DNA polymerase, which is present during viral replication.
HBV/HDV infection has a different natural history and different treatment to HBV mono-infection.
Patients with acute infection have raised levels of IgM to HBcAg (anti-HBc).
Patients with chronic hepatitis B are positive HBsAg for at least six months or positive HBsAg and negative IgM to HBcAg.
Hepatitis B treatment and management8
General advice regarding hepatitis B
To prevent infection, patients should be advised to avoid unprotected sexual intercourse, including oro-anal and orogenital contact until they have become non-infectious or their partners have received a full course of vaccination for protection against hepatitis B.
Patients should be given a detailed explanation of their condition with particular emphasis on the long-term implications for the health of themselves and their partner, and routes of transmission of infection, and should be advised not to donate blood.
Treatment of acute hepatitis B infection8
Arrange admission to hospital if seriously ill; otherwise, manage in primary care.
Notify the Health Protection Unit to facilitate appropriate surveillance.
Confirm the diagnosis with hepatitis serology (if not already confirmed).
If HBsAg is detected, refer the person promptly to the local appropriate specialist.
Treatment is mainly supportive with treatment of symptoms (fluids, antiemetics, rest).
Avoid alcohol until liver enzymes are normal.
Review the person's current medications. Stop any non-essential medication.
Itching can be difficult to treat. Advise simple measures (stay cool, wear loose clothing, avoid hot baths or showers). Chlorphenamine may help but should be avoided in severe liver impairment.
Treatment with antiviral agents is not usually indicated for acute hepatitis B except in cases of fulminant hepatitis.
National Institute for Health and Care Excellence (NICE) guidance on chronic infection management
Assessment
Arrange the following tests in primary care for adults who are HBsAg-positive:
HBeAg/anti-HBe status.
HBV DNA level.
lgM antibody to anti-HBc lgM.
HCV antibody (anti-HCV).
HDV antibody (anti-HDV).
HIV antibody (anti-HIV).
lgG antibody to hepatitis A virus (anti-HAV).
Additional laboratory tests include ALT or aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT), serum albumin, total bilirubin, total globulins, FBC and prothrombin time
Tests for HCC, including hepatic ultrasound and alpha-fetoprotein testing.
Referral
Refer all adults who are HBsAg-positive to a hepatologist or to a gastroenterologist or infectious disease specialist with an interest in hepatology.
Refer pregnant women who are HBsAg-positive to a hepatologist, or to a gastroenterologist or infectious disease specialist with an interest in hepatology, for assessment within six weeks of receiving the screening test result and to allow treatment in the third trimester.
Refer immediately adults who develop decompensated liver disease. Referral should be to a hepatologist or to a gastroenterologist with an interest in hepatology.
Refer all children and young people who are HBsAg-positive to a paediatric hepatologist or to a gastroenterologist or infectious disease specialist with an interest in hepatology.
Adults with HBeAg-positive chronic hepatitis B and compensated liver disease
Offer a 48-week course of peginterferon alfa-2a as first-line treatment in adults with HBeAg-positive chronic hepatitis B and compensated liver disease.
Offer tenofovir disoproxil as second-line treatment to people who do not undergo HBeAg seroconversion or who relapse (revert to being HBeAg-positive following seroconversion) after first-line treatment with peginterferon alfa-2a.
Offer entecavir as an alternative second-line treatment to people who cannot tolerate tenofovir disoproxil or if it is contra-indicated.
Avoid use of peginterferon alfa-2a in pregnancy unless the potential benefit outweighs risk. Women of childbearing potential must use effective contraception throughout therapy.
Adults with HBeAg-negative chronic hepatitis B and compensated liver disease
Offer a 48-week course of peginterferon alfa-2a as first-line treatment in adults with HBeAg-negative chronic hepatitis B and compensated liver disease.
Offer entecavir or tenofovir disoproxil as second-line treatment to people with detectable HBV DNA after first-line treatment with peginterferon alfa-2a.
Women who are pregnant or breastfeeding
Offer tenofovir disoproxil to women with HBV DNA greater than 107 IU/ml in the third trimester to reduce the risk of transmission of HBV to the baby.
Prophylactic treatment during immunosuppressive therapy
In people who are HBsAg-positive and have HBV DNA greater than 2000 IU/ml, offer prophylaxis with entecavir or tenofovir disoproxil:
Start prophylaxis before beginning immunosuppressive therapy and continue for a minimum of six months after HBeAg seroconversion and HBV DNA is undetectable.
In people who are HBsAg-positive and have HBV DNA less than 2000 IU/ml, offer prophylaxis.
Consider lamivudine if immunosuppressive therapy is expected to last for less than six months:
Monitor HBV DNA monthly in people treated with lamivudine and change to tenofovir disoproxil if HBV DNA remains detectable after three months
Consider entecavir or tenofovir disoproxil if immunosuppressive therapy is expected to last for longer than six months
Start prophylaxis before beginning immunosuppressive therapy and continue for a minimum of six months after stopping immunosuppressive therapy.
Monitoring of adults who do not meet the criteria for antiviral treatment
Monitor ALT levels every 24 weeks in adults with HBeAg-positive disease who are in the immune-tolerant phase (defined by active viral replication and normal ALT levels - less than 30 IU/ml in males and less than 19 IU/ml in females).
Monitor ALT every 12 weeks on at least three consecutive occasions if there is an increase in ALT levels.
Monitor ALT and HBV DNA levels every 48 weeks in adults with inactive chronic hepatitis B infection (defined as HBeAg-negative on two consecutive tests with normal ALT and HBV DNA less than 2000 IU/ml).
Consider monitoring more frequently in people with cirrhosis who have undetectable HBV DNA.
Hepatitis B infection and HIV infection9
Approximately 10% of those with HIV infection worldwide are also infected with hepatitis B.
Both viruses can be treated with a simplified combination of drugs.
Liver disease may progress more rapidly in those patients co-infected with HBV/HIV and could lead to serious liver disease complications such as cirrhosis and liver cancer at younger ages.
There is a higher risk of developing hepatotoxicity following the initiation of antiretroviral therapy in HIV patients co-infected with hepatitis B than there is in patients infected with HIV alone.
In patients infected with hepatitis B, HIV can lead to higher rates of chronicity, decreased rates of anti-HBe and anti-HBs seroconversion and increased viral replication, probably due to the impairment of the body's immune responses.
There is no evidence that hepatitis B affects HIV disease progression.
The choice of treatment of hepatitis B in patients with HIV infection depends on several factors, including the severity of liver disease and the patient's CD4 count.
Hepatitis B complications
Relapse.
Prolonged cholestasis.
Cirrhosis: patients with decompensated cirrhosis should be treated in specialised liver units, as treatment with antiviral therapy is complex and these patients may need liver transplantation.7
HCC - there is high risk of this in some non-cirrhotic patients, including African patients over the age of 20, Asian males over the age of 40, Asian females over the age of 50 and patients with a family history of HCC.
Concurrent hepatitis C infection can lead to fulminant hepatitis, more aggressive chronic hepatitis and increased risk of liver cancer.
Concurrent HIV infection increases the risk of progression to cirrhosis.
Surveillance testing for HCC in adults with chronic hepatitis B
Perform six-monthly surveillance for HCC by hepatic ultrasound and alfa-fetoprotein testing in people with significant fibrosis or cirrhosis.
In people without significant fibrosis or cirrhosis, consider six-monthly surveillance for HCC if the person is older than 40 years and has a family history of HCC and HBV DNA greater than or equal to 20,000 IU/ml.
Do not offer surveillance for HCC in people without significant fibrosis or cirrhosis who have HBV DNA less than 20,000 IU/ml and are younger than 40 years.
Prognosis
Without antiviral treatment, the five-year cumulative incidence of cirrhosis ranges from 8-20%.
People with cirrhosis face a significant risk of decompensated liver disease if they remain untreated.
Five-year survival rates among people with untreated decompensated cirrhosis can be as low as 15%.
Screening and prevention of hepatitis B
Hepatitis B testing in asymptomatic patients should be considered in:
Men who have sex with men.
Sex workers (of either sex).
Intravenous drug users.
HIV-positive patients.
Sexual assault victims.
People from countries where hepatitis B is common.
'Needlestick' victims.
Sexual partners of people who either have or who are at high risk of having hepatitis B.
Workers with occupational risk - eg, healthcare workers.
If non-immune, consider hepatitis B vaccination. If found to be chronic carriers, consider referral for therapy. See also the separate Hepatitis B Vaccination and Prevention article.
Vaccination may be universal or just for high-risk groups.
The current recombinant vaccine is one of the safest available but, being grown in yeast cells, it should not be given to those allergic to yeast.
Passive immunisation with specific hepatitis B immunoglobulin (HBIG) may be given to non-immune contacts after high-risk exposure.
Intimate contacts10
Partners should be notified and this documented at subsequent follow-up.
Contact tracing should include any sexual contact (penetrative vaginal or anal sex or oro-anal sex) or needle-sharing partners during the period in which the index case is thought to have been infectious.
The infectious period is from two weeks before the onset of jaundice until the patient becomes surface antigen-negative.
In cases of chronic infection, contacts should be traced as far back as any episode of jaundice, or to the time when infection is thought to have been acquired. This may be very difficult when looking back longer than two or three years.
Children who have been born to infectious women should be screened for hepatitis B, if the child was not vaccinated at birth.
Specific HBIG should be administered to a non-immune contact after a single unprotected sexual exposure or parenteral exposure (eg, 'needlestick' injury) if the contact is known to be infectious:
HBIG should be given as soon as possible, ideally within 48 hours, although it should still be considered up to a week after exposure.3
An accelerated course of vaccine (at 0, 1 and 2 months) should be given to those who receive HBIG, plus a booster dose at 12 months for those at continued risk.
Pregnancy
All babies born to infected mothers should receive a complete course of hepatitis B vaccine.
Babies born to highly infectious mothers should receive HBIG (preferably given within 24 hours of delivery) as well as active immunisation.
HBIG may be given simultaneously with vaccine but at a different site.
This reduces vertical transmission by 90%.
Further reading and references
- Guidelines on hepatitis B and C testing; World Health Organization (February 2017)
- Philips CA, Ahamed R, Abduljaleel JK, et al; Critical Updates on Chronic Hepatitis B Virus Infection in 2021. Cureus. 2021 Oct 30;13(10):e19152. doi: 10.7759/cureus.19152. eCollection 2021 Oct.
- Hepatitis B: guidance, data and analysis; Public Health England, July 2014
- Hepatitis B Fact sheet; World Health Organization, updated March 2015
- Immunisation against infectious disease - the Green Book (latest edition); UK Health Security Agency.
- Aspinall EJ, Hawkins G, Fraser A, et al; Hepatitis B prevention, diagnosis, treatment and care: a review. Occup Med (Lond). 2011 Dec;61(8):531-40.
- Cooke GS, Main J, Thursz MR; Treatment for hepatitis B. BMJ. 2010 Jan 5;340:b5429. doi: 10.1136/bmj.b5429.
- Tripathi N, Mousa OY; Hepatitis B
- EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection; European Association for the Study of the Liver (2017)
- Hepatitis B; NICE CKS, February 2022 (UK access only)
- Management of co-infection with HIV-1 and hepatitis B or C virus; British HIV Association (2010)
- United Kingdom National Guideline on the Management of the viral hepatitides A, B and C; British Association for Sexual Health and HIV (2015)
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 23 Mar 2027
24 Mar 2022 | Latest version

Feeling unwell?
Assess your symptoms online for free