Should you consider the copper coil for emergency contraception?
Peer reviewed by Dr Sarah Jarvis MBE, FRCGPLast updated by Milly EvansLast updated 11 Jul 2019
If you need emergency contraception, you should be aware of all of your options. The most effective method is also the least known: the copper coil, or intrauterine device (IUD).
In this article:
If you forgot to take your pill, the condom broke or you didn't use any contraception, you might be panicking about getting pregnant. That's when emergency contraception can come to the rescue.
Most people have heard of the so-called 'morning after pill', an emergency contraceptive tablet which can be taken up to three to five days (depending on the type of medication) after unprotected sex, delaying ovulation to prevent pregnancy. But although tablets such as Levonelle and EllaOne are good options, there is actually an even more effective emergency contraceptive which most people don't know about.
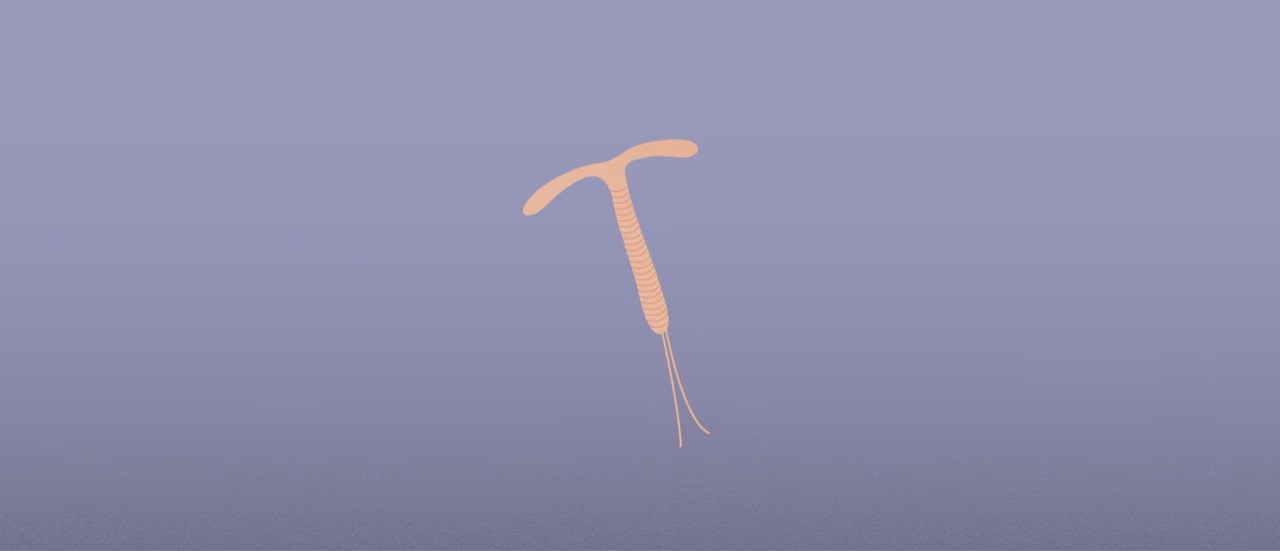
The copper coil, or IUD, is a form of long-acting reversible contraceptive which is not only the most effective form of emergency contraception but also keeps you protected against pregnancy for years after it's inserted. It is a small T-shaped copper and plastic device which is inserted into your uterus by a professional.
Research from the Faculty for Sexual and Reproductive Health (FSRH) has shown that only 13% of women aged 18-45 could identify the IUD as the most effective form of emergency contraception. In fact, only 15% of the women surveyed who had accessed emergency contraception had been offered the IUD.
Continue reading below
How effective is the copper coil?
Emergency contraception prevents pregnancy after potential exposure to semen. The IUD releases copper into the womb to stop the egg implanting or being fertilised.
Overall, emergency contraception is highly effective when used correctly. Following a single episode of unprotected sex, 6-8% would get pregnant if they did not use emergency contraception (this is an average across the cycle - clearly the risk is higher around ovulation and lower at other parts of the cycle).
By comparison, fewer than 0.1% of women will get pregnant after unprotected sex if an IUD is inserted within five days. Emergency contraceptive pills offer a lower level of protection. If the emergency contraceptive pill containing ulipristal acetate (marketed as EllaOne) is used within five days, 0.9-1.8% of women will get pregnant. With the progestogen-only emergency contraception, levonorgestrel (Levonelle), 1.1-2.6% of women will get pregnant. In addition this method is only licensed to be taken within three days of unprotected sex as it loses efficacy after this.
One of the drawbacks of using emergency contraceptive pills rather than the IUD is that they may not be effective if ovulation has already occurred in the cycle as they are designed to delay ovulation to prevent pregnancy. The IUD can be fitted at any point in the menstrual cycle, up to five days after unprotected sex or the earliest time that ovulation could have occurred. Implantation of a fertilised egg happens no earlier than five days after ovulation, which usually occurs mid-cycle (day 14 for someone with a 28-day menstrual cycle).
Patient picks for Birth control
How can you get an emergency IUD?
The IUD has a five-day window of very good protection against pregnancy. Like all emergency contraceptives, it is more effective the sooner you have it inserted after unprotected sex. It can also be fitted at any time in your menstrual cycle, as long as you are not pregnant, and is effective straightaway.
Unlike emergency contraceptive pills, you cannot get an IUD from your pharmacist but they should be able to signpost you to a service where you can, be that at your GP practice or a nearby sexual health service.
If you live near a sexual health clinic, that should be your first port of call for an emergency IUD, says Dr Jane Dickson, Vice President of the Faculty for Sexual and Reproductive Health. "Most walk-in sexual health clinics would be able to offer one, and there is more leeway as it can be fitted up to five days after unprotected sex (and sometimes even longer afterwards). As long as a coil fitter is available, most clinics would prioritise this and not turn a woman away." You should make the clinic aware that you need the IUD as emergency contraception so they are able to prioritise you.
Regardless of whether you are having an IUD fitted as emergency or regular contraception, the procedure is the same.
"We put a speculum (the same plastic instrument used for swab and smear tests) into the vagina. The IUD folds flat into an inserter which looks a bit like a straw. The inserter is put through the hole in the cervix to place the IUD in the uterus," explains Dickson. "Usually there is some period cramp-type pain which can be helped with a simple painkiller. There is no problem doing this on young women and we can do the procedure with a local anaesthetic gel or injection if needed." The procedure should only take around five minutes.
Continue reading below
Benefits and drawbacks
Many women are scared away from the IUD by horror stories of side effects and pain. It's certainly not for everyone but many women are very happy using the IUD as contraception. And long-acting reversible contraceptive (LARC) methods actually have a higher rate of satisfaction overall than the oral contraceptive pill.
There can be some pain during and after the IUD is inserted, but this can often be dealt with using painkillers. Some women find that their periods become longer, heavier and more painful and may experience spotting for the first 3-6 months. The majority of women who stop using the IUD do so because of vaginal bleeding and pain, although these are uncommon side effects.
There are small risks of getting a pelvic infection, the IUD being rejected, experiencing damage to the womb or having an ectopic pregnancy. Many centres will take swabs to exclude sexually transmitted infections before inserting an IUD, but clearly this can't be done in an emergency. As an alternative, you may be offered a single dose of antibiotics. Both swabs and antibiotics reduce the risk of getting a pelvic infection.
There are also many benefits. As well as being a long-term contraception solution, it is highly effective, partly because there is reduced risk of human error in using it. One of the reasons people like it is that it is non-hormonal and so doesn't cause side effects like acne, headaches and breast tenderness. It also does not affect your future fertility, or increase your risk of cervical cancer, womb cancer or ovarian cancer. It protects you from pregnancy immediately after insertion and does not interfere with sex.
According to Jackie Redding, head of operations at young people's sexual health charity Brook, there needs to be more awareness of LARC methods and their benefits, both as emergency and ordinary contraception. "We believe that all young people should be given the information they need to make informed decisions about their contraceptive choices, and we understand that it can take time to find the best method for every individual."
Sexual health awareness
Although emergency contraception is effective and the emergency contraceptive pill can be taken multiple times without impacting your health or fertility, a regular method of contraception is far more effective as it prevents pregnancy before unprotected sex occurs. Emergency contraception will not protect you against sexually transmitted infections (STIs) so you should get tested if you may have been exposed.
If you have had an IUD inserted, that can be used as your regular contraception for the months or years that you have it in. You should still protect yourself from STIs as only condoms protect you from both pregnancy and STIs.
Redding reflects that a lack of awareness is stopping women from accessing IUDs as emergency contraception. "The IUD can prevent pregnancy up to five days after unprotected sex and has the benefit of being used as a continuous method of contraception for between five and 10 years. At Brook we feel very passionately about raising awareness of the IUD as emergency contraception.
"Relationships and Sex Education are absolutely key to ensuring that young people know about all the methods of contraception and emergency contraception available to them. More also needs to be done to dispel the misconception that emergency contraception must be taken the morning after," she explains.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
11 Jul 2019 | Latest version

Feeling unwell?
Assess your symptoms online for free

