Ectopic pregnancy
Peer reviewed by Dr Rosalyn Adleman, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 8 Jul 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
An ectopic pregnancy is a pregnancy which is not in the womb - the normal place. Ectopic means 'misplaced'. It occurs in about 11 in 1,000 pregnancies. Although many ectopic pregnancies are now treated without the need for an operation, you should always see a doctor urgently if you think you have an ectopic pregnancy symptoms. Symptoms include lower tummy (abdominal) pain which can become severe. A ruptured ectopic pregnancy is life-threatening, needing emergency surgery.
In this article:
Video picks for Bleeding in pregnancy
Playlist: Ectopic Pregnancy
4 videos
What is an ectopic pregnancy?
Dr Sarah Jarvis MBE, FRCGP
What is an ectopic pregnancy?
Dr. Sarah Jarvis MBE, FRCGP

What is the cause of an ectopic pregnancy?
Dr. Sarah Jarvis MBE, FRCGP

Is an ectopic pregnancy hereditary?
Dr. Sarah Jarvis MBE, FRCGP

What does an ectopic pregnancy feel like?
Dr. Sarah Jarvis MBE, FRCGP
Continue reading below
What is an ectopic pregnancy?
An ectopic pregnancy is when a fertilised egg implants and matures outside the womb (uterine cavity). Most ectopic pregnancies occur in one of the fallopian tubes.
How common are ectopic pregnancies?
Back to contentsEctopic pregnancy can occur in any sexually active woman. In the UK there are nearly 12,000 women with ectopic pregnancies seen in hospitals each year.
Continue reading below
Ectopic pregnancy symptoms
Back to contentsEctopic pregnancy symptoms typically develop around the sixth week of pregnancy. This is about two weeks after a missed period if you have regular periods. However, symptoms may develop at any time between 4 and 10 weeks of pregnancy, and if your periods are irregular, then it may not be clearly related to a missed period.
You may not be aware that you are pregnant. For example, your periods may not be regular, or you may be using contraception and not realise it has failed. Ectopic pregnancy symptoms can also start about the time a period is due. At first you may think the symptoms are just a late period, or due to some other cause of lower tummy (abdomen) pain.
Ectopic pregnancy symptoms include one or more of the following:
Pain on one side of the lower tummy (abdomen). It may develop sharply, or may slowly get worse over several days. It can become severe.
Vaginal bleeding often occurs but not always. It is often different to the bleeding of a period. For example, the bleeding may be heavier or lighter than a normal period. The blood may look darker. However, you may think the bleeding is a late period.
Other symptoms may occur such as diarrhoea, feeling faint, or pain on passing poo (a stool).
Shoulder-tip pain may develop. This is due to some blood leaking into the abdomen and irritating the muscle used to breathe (the diaphragm).
You may feel dizzy or faint.
If the fallopian tube ruptures and causes internal bleeding, you may develop severe pain or 'collapse'. This is an emergency as the bleeding is heavy.
Sometimes there are no warning symptoms (such as pain) before the tube ruptures. Therefore, collapse due to sudden heavy internal bleeding is occasionally the first sign of an ectopic pregnancy.
What causes an ectopic pregnancy?
Back to contentsMost ectopic pregnancies occur when a fertilised egg (ovum) attaches to the inside lining of a fallopian tube (a tubal ectopic pregnancy). Rarely, an ectopic pregnancy occurs in other places such as in the ovary, the neck of the womb (cervix) or inside the tummy (abdomen).
Also rarely, a pregnancy can develop in the womb at the same time as an ectopic pregnancy outside the womb (a heterotopic pregnancy). The rest of this leaflet deals only with tubal ectopic pregnancy.
Continue reading below
What increases the risk of an ectopic pregnancy?
Back to contentsThe chance is higher than average in the following at-risk groups:
If you have already had an ectopic pregnancy you have a slightly higher chance that a future pregnancy will be ectopic. If you have had two or more previous ectopic pregnancies then your chances of another ectopic pregnancy are even greater.
If you have damage to, or other abnormality of a fallopian tube. This is because a fertilised egg (ovum) may become stuck in the tube more easily. For example:
If you have had a previous infection of the womb (uterus) or fallopian tube (pelvic inflammatory disease). This is most commonly due to either chlamydia or gonorrhoea. These infections can lead to some scarring of the fallopian tubes.
Previous sterilisation operation (also known as tubal ligation). Sterilisation is a very effective method of contraception. However, in the rare event that a pregnancy does occur, it has a higher risk of being ectopic.
Any previous surgery on your fallopian tubes or nearby structures.
If you have a condition causing inflammation of the uterus and surrounding area (endometriosis).
If you get pregnant while using an intrauterine contraceptive device (IUD). Pregnancy is rare as this is a very effective method of contraception and so the absolute number of ectopic pregnancies is greatly reduced if you are using an IUD. However, if you become pregnant while using an IUD, the pregnancy has a higher chance of being ectopic than if you did not have the IUD and so you must seek medical help as soon as you see a positive pregnancy test.
Many women with an ectopic pregnancy do not have any of these risk factors.
Understanding normal early pregnancy
Back to contentsAn egg (ovum) is released from an ovary into a fallopian tube. This is called ovulation and usually occurs once a month about halfway between periods. Sperm can survive in the fallopian tubes for up to five days after you have had sex.
A sperm may then combine with the ovum (fertilisation) to make an embryo. The tiny embryo is swept along a fallopian tube to the womb (uterus) by tiny hairs (cilia). It normally attaches to the inside lining of the uterus and develops into a baby.
Female reproductive system
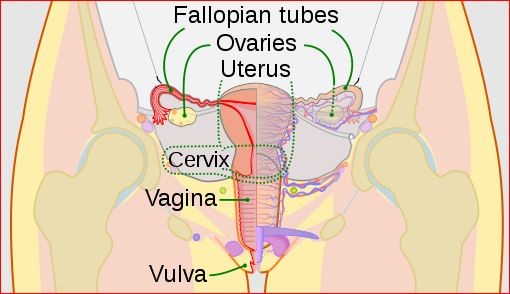
© CDC, Mysid, Public domain, via Wikimedia Commons
By CDC, Mysid, Public domain, via Wikimedia Commons
What are the complications of an ectopic pregnancy?
Back to contentsA tubal ectopic pregnancy never survives and cannot be moved into the womb (uterus). Possible outcomes include the following:
The pregnancy often dies after a few days. About half of ectopic pregnancies probably end like this. You may have no symptoms and you may never have known that you were pregnant. Sometimes there is slight pain and some vaginal bleeding similar to a miscarriage. Nothing further needs to be done if this occurs.
The pregnancy may grow for a while in the narrow fallopian tube. This can stretch the tube and cause symptoms. This is when an ectopic pregnancy is commonly diagnosed. If the pregnancy grows further it will normally split (rupture) the fallopian tube. This can cause heavy internal bleeding and pain and is a medical emergency, because the woman can lose a lot of blood very quickly.
How are ectopic pregnancies diagnosed?
Back to contentsIf you have symptoms that may indicate an ectopic pregnancy you will usually be seen in the hospital immediately.
A urine sample shows a positive pregnancy test to confirm that you are pregnant.
An ultrasound scan may confirm an ectopic pregnancy, but more usually it will show that the uterus is empty despite a positive pregnancy test, indicating that the pregnancy is likely to be ectopic. This is usually an internal (transvaginal) scan which is not painful. However, the scan may not be clear if the pregnancy is very early. If this is the case then a repeat scan a few days later is often done.
Blood tests that show changes in the level of a pregnancy hormone called human chorionic gonadotrophin (hCG) are also usually done. In a pregnancy which is developing, the hCG levels double every 48 hours - in an ectopic pregnancy they will usually increase more slowly.
Ectopic pregnancy treatment
Back to contentsRuptured ectopic pregnancy
Emergency surgery is needed if a fallopian tube splits (ruptures) with heavy bleeding. The main aim is to stop the bleeding. The ruptured fallopian tube and remnant of the early pregnancy are then removed. The operation is often life-saving.
Early ectopic pregnancy - before rupture
Ectopic pregnancy is most often diagnosed before rupture. Your doctor will discuss the treatment options with you and, in many cases, you are able to decide which treatment is best for you. These may include the following:
Surgery.
Removal of the tube (either the whole tube or part of it) and the ectopic pregnancy is most commonly performed by keyhole surgery (a laparoscopic operation). Removal of the fallopian tube containing the ectopic pregnancy (salpingectomy) is usually performed if the other tube is healthy. Removal of only a section of the tube with the ectopic pregnancy in it (salpingotomy) is usually performed if the other tube is already damaged.
Medical treatment.
Medical treatment of ectopic pregnancies is now an option in many cases and avoids the need for surgery. A medicine called methotrexate is often given, usually as an injection. It works by killing the cells of the pregnancy growing in the fallopian tube. It is normally only advised if the pregnancy is very early. The advantage is that you do not need an operation. The disadvantage is that you will need close observation for several weeks with repeated blood tests and scans to check it has worked. You will need to have a blood test for hCG every 2-3 days until your levels are low. Scans are usually repeated weekly. Methotrexate can cause side-effects which include feeling sick (nausea) and being sick (vomiting) in some women. It can be common for some tummy (abdominal) pains to develop 3-7 days after having methotrexate.
Wait and see.
Not all ectopic pregnancies are life-threatening or lead to a risk to the mother. In many cases the ectopic pregnancy resolves by itself with no future problems. The pregnancy often dies in a way similar to a miscarriage. A possible option is to see how things go if you have mild or no ectopic pregnancy symptoms. You would need to have treatment if symptoms become worse. You will need close observation by your gynaecologist and repeated scans and blood tests to check on how things are developing.
If your blood group is rhesus negative then you will need an injection of anti-D immunoglobulin if you have an operation for your ectopic pregnancy or if you have had a lot of bleeding. You are rhesus positive if you have the rhesus factor, which is a protein on the surface of your red blood cells. If the protein is not present, you are rhesus negative.
All pregnant women have a blood test to determine whether they are rhesus positive or negative. The injection of anti-D immunoglobulin simply prevents you from producing antibodies, which can be harmful in future pregnancies, if you are rhesus negative. You do not need this injection though if you receive medical treatment.
The above is a brief description of treatment options. A gynaecologist (consultant specialist in women's health) will advise on the pros and cons of each treatment with you. This will include any complications or side-effects which could occur with each option.
What if I have a pregnancy in the womb at the same time as an ectopic pregnancy?
Back to contentsThis is called a heterotopic pregnancy and is unusual, happening in around 1 in 30,000 pregnancies. It is more common if you have become pregnant with in vitro fertilisation (IVF) treatment. If the pregnancy in the womb is healthy and developing normally then it will not be possible to have methotrexate treatment. This is because it would damage the baby in the right place as well as the tissue growing in the wrong place.
You may need an operation or injection to remove or destroy the pregnancy in the wrong place, so that the normal pregnancy can continue safely. In some cases no treatment is needed, and the pregnancy in the wrong place will resolve itself, leaving you only with the normal pregnancy. Again, your specialist will advise you.
Is ectopic pregnancy dangerous?
Back to contentsIn the event of the ectopic pregnancy rupturing, there may be severe consequences. Heavy bleeding can cause serious medical problems and even death. However, most women are now diagnosed in the early stages, before this happens. In this scenario, most women recover very well.
There are some rare complications after surgery, which your gynaecologist would discuss with you before the operation. As discussed, there are often some side-effects from taking the medical treatment option.
Women often want to know if they will be able to have a normal pregnancy in the future after an ectopic pregnancy. If you had no past history of problems conceiving or diseases involving your fallopian tubes before your ectopic pregnancy, and a fallopian tube is not removed as part of treatment, your fertility will not be affected and you should have no more chance of having an ectopic pregnancy than a woman who has not had an ectopic pregnancy.
If you had one of the risk factors above, however, you may be more at risk of problems in the future. If you had to have an operation, you are more likely to have fertility problems and problems with future ectopic pregnancies than if you had medical treatment or no treatment was needed.
Even if one fallopian tube is completely removed, you have about a 6 in 10 chance of having a future normal pregnancy. (The other fallopian tube will still usually work.) However, 1-2 in 10 future pregnancies may lead to another ectopic pregnancy. It is therefore important that if you have had an ectopic pregnancy in the past you should go to see your doctor early in future pregnancies.
It is common to feel anxious or depressed for a while after treatment. Worries about possible future ectopic pregnancy, the effect on fertility, and sadness over the loss of the pregnancy are normal. Do talk with a doctor about these and any other concerns following treatment. You should not get pregnant for three months after having an ectopic pregnancy treated with methotrexate. This is because methotrexate is teratogenic (can damage a developing foetus) and so it is important that you leave time for it to fully leave your body.
Can an ectopic pregnancy be prevented?
Back to contentsIt is not possible to fully prevent an ectopic pregnancy, as some women have one with no risk factors. You can reduce the risk by not acquiring any risk factors eg, always using condoms and having regular tests to ensure that you don't catch a sexually transmitted infection, or that if you do catch one, it is treated early.
In summary
Back to contentsEctopic pregnancy is common. The pregnancy never survives.
The typical first symptom is pain in the lower tummy (abdomen) after a recent missed period.
As the pregnancy grows it may tear (rupture) the fallopian tube, requiring emergency surgery.
Planned treatment before rupture occurs is best.
Many women with ectopic pregnancies do not need surgery.
Patient picks for Bleeding in pregnancy

Pregnancy
Molar pregnancy
A molar pregnancy (hydatidiform mole) is when a mass of tissue grows inside your womb (uterus) that will not develop into a baby. It is the result of abnormal conception. It may cause bleeding or severe vomiting in early pregnancy and is usually picked up in an early pregnancy ultrasound scan. It needs to be removed and most women can expect a full recovery.
by Dr Doug McKechnie, MRCGP

Pregnancy
Recurrent miscarriage
The loss of a much-wanted pregnancy can be devastating, and even more so if it happens again. This leaflet explains the definition of recurrent miscarriage and explores the tests and treatments that may be needed. The good news is that the eventual outlook is generally good as most couples who have experienced recurrent miscarriage go on to have a successful pregnancy.
by Dr Mary Harding, MRCGP
Further reading and references
- Diagnosis and management of ectopic pregnancy; Royal College of Obstetricians and Gynaecologists. Green Top Guideline No 21. November 2016
- Ectopic pregnancy and miscarriage: diagnosis and initial management; NICE Guidance (last updated August 2023)
- Ectopic pregnancy; NICE CKS, February 2023 (UK access only)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 7 Jul 2027
8 Jul 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.