Fractured humerus
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 9 Feb 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Broken upper arm article more useful, or one of our other health articles.
In this article:
Continue reading below
How common are humerus fractures?
Fractures of the humerus are common and usually result from injury. They are also associated with pathological fractures and osteoporosis, particularly in the elderly.
Humeral fractures account for 4-6% of all fractures in young people and 1-3% of all fractures in the elderly. 1
The anatomy of the humerus
Back to contentsHumerus - front
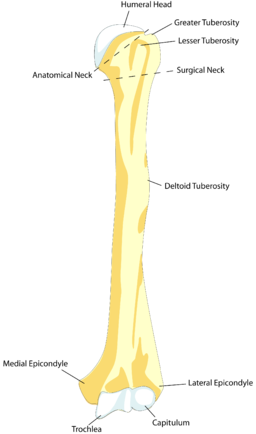
© BDB, Public domain, via Wikimedia Commons
By BDB, Public domain, via Wikimedia Commons
The humeral head articulates with the glenoid fossa of the scapula. The anatomical neck separates the greater and lesser tuberosities from the humeral head. The long head of biceps runs between the tuberosities in the bicipital groove, and the surgical neck is just below the greater and lesser tuberosities.
The radial nerve runs posteriorly around the middle third of the humeral shaft in the spiral groove. The medial and lateral epicondyles are at the lower end of the humerus, and the joint surface consists of the capitulum (articulates with the head of the radius) and the trochlea (articulates with the ulna).
Continue reading below
Mechanism of injury
Back to contentsFractures of the humerus usually result from falls or direct trauma. In young men, high-energy trauma is the commonest cause; in older women, they most often result from a fall from standing.1
In children the possibility of non-accidental injury should be borne in mind when taking the history and examining the child, especially in very young children. In the elderly, pathological fracture should be considered.
Important information |
|---|
The humerus is a relatively common site of pathological fracture. 8% of humeral shaft fractures in a Swedish study were pathological.2 Suspect pathological fracture if any of the following features are present: Bone pain preceding fracture. Limb swelling predating fracture, or marked post-fracture swelling. Cystic abnormality of the humerus on X-ray. History of malignancy, particularly metastatic. Paget's disease of bone. |
Classification of humeral fractures
Back to contentsClassification of humeral fractures is difficult. One method is to classify them as:
Proximal humeral fractures.
Humeral shaft fractures.
Distal humeral fractures.
Fracture of the supracondylar (distal) humerus is one of the most common fractures encountered in children.3 Fractures of the distal humerus in the adult account for approximately one third of all humeral fractures.4 Distal humeral fractures are discussed in the separate Elbow injuries and fractures article.
Continue reading below
Proximal humeral fractures
Back to contentsProximal humerus fractures often occur in older patients after a low-energy fall.5
How common are proximal humeral fractures? (Epidemiology)
Proximal humeral fractures are the 7th most common fracture in adults and make up between 4 and 10% of all fractures.6Their frequency increases with age in mobile and active patients.
Mechanism of injury
Usually after a fall on to an outstretched hand from standing height.
Can also occur during seizures or electric shock when fracture may be associated with a posterior shoulder dislocation.
Can also result from a direct blow.
High-energy trauma is unusual in a proximal humeral fracture.6
Age group affected
People between the ages of 40 and 80 are most commonly affected. It is common in women. Many patients are osteoporotic.
In younger people, the same injury mechanism can cause fracture with co-existing shoulder dislocation. In younger age groups, trauma is likely to be of higher energy and the resulting injury more serious. Humeral epiphysis separation can occur in adolescents.
Symptoms of proximal humeral fractures (presentation)7
History of trauma.
Pain, loss of shoulder/arm function, swelling and bruising.
Proximal humerus fractures may either occur in isolation or be associated with concurrent dislocation of the glenohumeral joint. Additional injuries to the shoulder girdle may also be present, such as scapular fractures causing a 'floating shoulder'.
Assessment of proximal humeral fractures
Determine the injury mechanism. Establish whether osteoporosis is likely.
Assess for associated injuries to the arm/shoulder/chest wall/lungs.
Perform a neurological examination, particularly examining the axillary nerve by testing for sensation in the regimental badge area over the deltoid muscle and assessing upper limb muscle power. Assess for brachial plexus injury through distal neurological examination.
Check peripheral pulses.
If there are neurological or vascular deficits, orthopaedic referral is required.
Diagnosing proximal humeral fractures (investigations)
X-rays - include AP, trans-scapular (or Y) and axillary views.
CT scan may be needed in difficult cases.
Classification of proximal humeral fractures
Neer classification: based on the four usual cleavage lines that occur due to the anatomy of the proximal head of the humerus (the articular segment or head, the lesser tuberosity, the greater tuberosity and the surgical neck/shaft). Two-part, three-part and four-part fractures can occur. The fractures are then classified by their degree of displacement and angulation.
Considered to be displaced if there is more than 10 mm movement or angulation >45°.
Surgical neck fractures are the most common type of proximal humeral fracture.
Management of proximal humeral fractures
General principles: the fracture should be immobilised as soon as possible and potent analgesia given. Keep the patient comfortable and minimise any need for movement. Open fractures, those associated with a shoulder dislocation or combined with fracture in the forearm are a surgical emergency and an immediate orthopaedic opinion is necessary.
Most fractures are extra-articular and minimally displaced.
Most proximal humeral fractures can be treated non-operatively. This involves the use of a sling or a shoulder immobiliser. A physiotherapy referral should be made.
If displaced or open, surgery may be needed.8
Surgery involves either hemiarthroplasty, open reduction and internal fixation, or reverse shoulder arthroplasty.9
Reverse shoulder arthroplasty (RSA) is becoming more popular than open reduction and internal fixation (ORIF). RSA results in fewer early complications and re-operations than ORIFs; however patients who had an RSA were more likely to be re-admitted within 90 days of the surgery. It is thought that this might reflect the fact that RSA is more likely to be offered to an older cohort with other co-morbidities.9
Fracture dislocations and fractures of the anatomical neck should be referred for orthopaedic review.
Complications of proximal humeral fractures
Neurovascular injury: about a third of proximal humeral fractures result in neurovascular injury. Axillary nerve damage is most common. Suprascapular, radial and musculocutaneous nerves can also be affected. Axillary artery injury may (rarely) occur (look for expanding mass over the proximal shoulder girdle). The brachial artery is also rarely injured.
Avascular necrosis of the humeral head: this is more common in complex fractures with multiple fragments where interruption to the blood supply is more likely and in fractures of the surgical neck. It causes pain and stiffness in the shoulder. Shoulder arthroplasty may eventually be needed or may be the initial treatment of choice in the fracture management. The development of intramedullary nails and minimally invasive locking plates provides greater ability to fix more complex fractures with less risk to the blood supply.
Malunion.
Associated glenohumeral dislocation.
Associated rotator cuff injury.
Prognosis
This depends on fracture type, mechanism of injury and the patient's age and underlying health. In general, an elderly person with a proximal humeral fracture rarely regains full range of movement, whether treated conservatively or surgically. The aim is rehabilitation to a functional range of movement.
Generally recovery takes at least one year but union is expected at 6-8 weeks.
Prevention of proximal humeral fractures
Adequate treatment of those at risk of osteoporosis.
Important information |
|---|
Hill-Sachs lesion10 This is a type of proximal humeral fracture: It is defined as a posterolateral humeral head compression fracture and can occur following anterior shoulder dislocation. It occurs in 35-40% of anterior dislocations and up to 80% of recurrent dislocations. X-ray views should include an AP view of the shoulder in internal rotation and a special view known as the Stryker notch view. The reverse Hill-Sachs lesion is a compression fracture of the anteromedial humeral head as a result of posterior shoulder dislocation. |
Humeral shaft fractures
Back to contentsHow common are humeral shaft fractures? (Epidemiology)
Humeral shaft fractures are a relatively common fracture. The incidence has an overall bimodal distribution due to a peak incidence for males between 20 to 30 years old and a second peak for older females aged between 60 and 70 years.11
60% of humeral shaft fractures occur in people over 50 years of age. 70% of those under 50 at the time of injury are men; 70% of those over 50 are women.12
The middle third is the most commonly fractured part of the shaft.12
Mechanism of injury
A humeral shaft fracture is usually a result of direct trauma or torsion injury to an upper limb. Occasionally, a fall on to an outstretched abducted arm can result in a humeral shaft fracture. Blunt injury/bending forces usually cause transverse fractures. Torsional force tends to result in spiral fracture.
Symptoms of humeral shaft fractures (presentation)
History of trauma.
Arm pain, swelling and deformity.
Assessment of humeral shaft fractures
Neurovascular examination should be performed. Particular attention should be paid to radial nerve assessment.
Diagnosing humeral shaft fractures (investigations)
AP and lateral X-rays of the humerus.
Include views of the shoulder and the elbow.
Classification of humeral shaft fractures
There is no recognised universally accepted classification. Can be described using:
Location - proximal, middle, distal. Distal third humeral fractures are also known as Holstein-Lewis fractures.
Type of fracture line - transverse, oblique, spiral, comminuted, segmental.
Open or closed.
Management of humeral shaft fractures
Conservative management is the treatment of choice for most humeral shaft fractures.13
Most can be treated non-operatively in a hanging arm cast or coaptation splint (a splint from the axilla to the nape of the neck with a stirrup around the elbow) followed by a functional arm brace (this has an anterior and posterior plastic shell held together by adjustable Velcro® straps) after 1-3 weeks. A physiotherapy referral should be made.
Mildly displaced/overlapping humeral shaft fractures may be treated by closed reduction and long arm splint from shoulder to wrist. After any humeral closed reduction, neurovascular assessment and X-rays should be repeated.
Surgical fixation may be needed if the fracture is segmental or if there is vascular compromise.
Surgical fixation may be done by external fixation, intramedullary nail fixation, and open reduction and internal fixation (ORIF).12 Radial nerve injury, which may only be temporary, is a risk in any operative procedure.
Complications of humeral shaft fractures13
Radial nerve injury.
Brachial artery injury.
Non-union.
Prognosis
Uncomplicated fractures usually heal within four months.
Further reading and references
- Image of proximal humerus fracture; Wheeless' Textbook of Orthopaedics
- Image of transverse humeral shaft fracture; Wheeless' Textbook of Orthopaedics
- Attum B, Thompson JH; Humerus Fractures Overview.
- Ekholm R, Adami J, Tidermark J, et al; Fractures of the shaft of the humerus. An epidemiological study of 401 fractures. J Bone Joint Surg Br. 2006 Nov;88(11):1469-73.
- Kumar V, Singh A; Fracture Supracondylar Humerus: A Review. J Clin Diagn Res. 2016 Dec;10(12):RE01-RE06. doi: 10.7860/JCDR/2016/21647.8942. Epub 2016 Dec 1.
- Amir S, Jannis S, Daniel R; Distal humerus fractures: a review of current therapy concepts. Curr Rev Musculoskelet Med. 2016 Jun;9(2):199-206. doi: 10.1007/s12178-016-9341-z.
- Monica J, Vredenburgh Z, Korsh J, et al; Acute Shoulder Injuries in Adults. Am Fam Physician. 2016 Jul 15;94(2):119-27.
- Epidemiology of proximal humerus fractures; S Iglesias-Rodriguez, Journal of Orthopaedic Surgery and Research
- Vachtsevanos L, Hayden L, Desai AS, et al; Management of proximal humerus fractures in adults. World J Orthop. 2014 Nov 18;5(5):685-93. doi: 10.5312/wjo.v5.i5.685. eCollection 2014 Nov 18.
- Jordan RW, Modi CS; A review of management options for proximal humeral fractures. Open Orthop J. 2014 Jun 27;8:148-56. doi: 10.2174/1874325001408010148. eCollection 2014.
- Alrabaa RG, Ma G, Truong NM, et al; Trends in Surgical Treatment of Proximal Humeral Fractures and Analysis of Postoperative Complications Over a Decade in 384,158 Patients. JB JS Open Access. 2022 Nov 2;7(4):e22.00008. doi: 10.2106/JBJS.OA.22.00008. eCollection 2022 Oct-Dec.
- Hill Sachs Lesion; Wheeless' Textbook of Orthopaedics
- Clement ND; Management of Humeral Shaft Fractures; Non-Operative Versus Operative. Arch Trauma Res. 2015 Jun 20;4(2):e28013. doi: 10.5812/atr.28013v2. eCollection 2015 Jun.
- Bounds EJ, Frane N, Jajou L, et al; Humeral Shaft Fractures.
- Gallusser N, Barimani B, Vauclair F; Humeral shaft fractures. EFORT Open Rev. 2021 Jan 4;6(1):24-34. doi: 10.1302/2058-5241.6.200033. eCollection 2021 Jan.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 8 Feb 2028
9 Feb 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free