Uterine cervix and common cervical abnormalities
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 17 Jun 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Common problems of the cervix article more useful, or one of our other health articles.
In this article:
Continue reading below
Anatomy of the cervix
The cervix is the part of the inverted pear-shaped uterus that corresponds to the narrow stalk end of the pear. This cylindrical-shaped muscular structure is about 3-5 cm in length and lies partly in the upper vagina, extending superiorly into the retroperitoneal space behind the bladder and in front of the rectum.
Reproductive female anatomy diagram
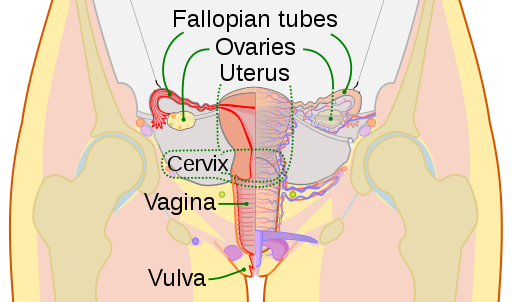
© CDC, Mysid, Public domain, via Wikimedia Commons
By CDC, Mysid, Public domain, via Wikimedia Commons
It is supported by ligaments (cardinal ligaments laterally and uterosacral ligaments posterolaterally). Due to anteversion and retroversion, the cervix rarely lies in the same longitudinal plane as the uterus and is mobile. The cervix opens into the uterine cavity superiorly (via the internal os) and into the vagina inferiorly (via the external os). The os appears round in nulliparous women but can be seen as a transverse slit in those who have gone through labour.
Sectional view diagram

© Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0, via Wikimedia Commons
By Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436; CC BY 3.0, via Wikimedia Commons
It is mainly composed of involuntary muscle superiorly and fibrous connective tissue inferiorly. The cervix is lined in its upper two thirds by ciliated, cylindrical epithelium which changes to stratified squamous epithelium at the squamocolumnar junction or transformation zone, usually found at the external os. Its location in relation to the external os varies depending on age, oestrogen use and other factors, including pregnancy. The transformation zone is the site of initiation of cervical cancer, the second most common cancer in women.
The cervix receives its blood supply from the ovarian and uterine arteries (originating from the aorta and internal iliac arteries respectively). It has an autonomic (sympathetic and parasympathetic) nerve supply and lymphatic drainage is to the external and internal iliac lymph nodes as well as the obturator node and the sacral nodes.
Physiology of the cervix
Back to contentsThe cervix acts as a canal between the vagina and the body of the uterus. Numerous deep glandular follicles lining the mucous membrane of the endocervix are responsible for the production of mucus. This mucus changes consistency in response to the levels of oestrogen: it is profuse, watery and alkaline when levels are high but, as levels drop post-ovulation, it becomes thick, scant and acidic. During pregnancy, it becomes even thicker and more tenacious, forming a plug rich in leukocytes. Microglandular hyperplasia can occur during pregnancy and immediately postpartum as well as in women taking progesterone treatment.
Continue reading below
Examination of the cervix
Back to contentsGeneral points
Examination of the cervix should be carried out in conjunction with examination of the other associated structures.
Offer a chaperone (document this).1
Always explain exactly what you are going to do at the outset.
Prepare everything in advance so that there is no interruption mid-examination.
Encourage the patient to empty her bladder before beginning examination.
Preparation and items required
Verbal consent from the patient.
A comfortable couch with a disposable sheet.
A drape for the patient to cover her torso and legs.
A flexible light source.
Non-sterile gloves (double glove if you plan to then do a rectal examination).
Warm running water.
Vaginal speculae in various sizes (place in warm water if metallic).
Lubricating jelly.
Any additional instruments you may need, such as a cervical smear kit.
Examination2
Position the patient correctly: she should be lying on her back, heels drawn up towards her bottom and knees gently relaxing open; her feet may be together or apart, whichever she finds more comfortable.
Warm the speculum if necessary and add a small amount of lubricating jelly to it.
Let the patient know that you are going to start.
Examine the vulva, expose the introitus, retracting the labia and pubic hair, and insert the closed speculum, initially with the handles to one side, then as you insert it pointing down towards the lower back, gradually turn it 90° so that the handles are anterior.
When the handles of the speculum are almost flush with the perineum, gently open it without exerting pressure on the sensitive tissues of the urethra and clitoris. Position it so that the cervix lies between the two arms of the speculum.
Examine the cervix, making note of the shape of the os, uniformity of colour, and any asymmetry, lumps or other abnormalities.
Carry out a smear if appropriate.
Gently pull the speculum back while still open, just enough to clear the cervix (1-2 cm), then loosen the speculum before fully withdrawing it.
The elusive cervix:
If the cervix is not immediately visible, don't withdraw immediately:Consider angling the blades of the speculum (anteriorly or posteriorly) until it comes into view.
If it is partially concealed, a swab may be used to bring it fully out (it is essential to be able to see its entire circumference).
The chaperone or woman herself may apply gentle pressure on the suprapubic area.
Putting her hands in fists in the small of her back or under her buttocks, thus tilting the pelvis, may help.
Performing a bimanual examination will determine the location of the cervix and you can then consider whether the size of the speculum is right (if it is too small, it will not reach the fornices).
Laying the patient on her side is also used with varying success and has been shown useful in obese patients.3
In obese and multiparous women, the vaginal walls may prolapse between the sides of the speculum, obscuring the view. In this situation, a condom or finger of a glove with the tip cut off, can be rolled on to the speculum. This will then hold back the vaginal wall between the bills of the speculum.
If the view is still not adequate, abandon the procedure and either bring the patient back another day or refer to a colleague or a colposcopy clinic. Be sure to explain what is happening and why.
Intimate gynaecological examinations can be particularly stressful for women with a history of sexual abuse because of the perceived loss of control, power disparity and the physical sensation of the examination.4 5 Clinicians need to be alert to this.6
Further investigative procedures
Back to contentsColposcopy
In certain situations, a speculum examination is not enough (most commonly if abnormal cells are picked up on a routine smear test but also in cases of bleeding after intercourse, persistent severe vaginal discharge, and intermenstrual bleeding, and in immunocompromised patients) and the cervix may need to be further assessed using a colposcope (a mounted binocular microscope). From the patient's perspective, this involves a similar procedure to a speculum examination, although the procedure is longer. The woman is examined in the lithotomy position, using stirrups, and it may involve application of acetic acid or iodine. A biopsy may also be taken and laser treatment carried out. Colposcopy can safely be performed during pregnancy but biopsies and treatment will be postponed until after the time of delivery.
Other procedures
Further assessment of the cervix is usually carried out in the context of suspicions of uterine abnormality, in which case, hysteroscopy or laparoscopy may be indicated.
For information about cancer of the cervix and related topics, see the separate articles Cervical screening (Cervical smear test) and Cervical cancer.
Continue reading below
Structural abnormalities
Back to contentsCongenital abnormalities
These are relatively uncommon and occur as one of three problems:
Failure of fusion of the Müllerian ducts during development, resulting in a duplicated or septate cervix (one cervix with two openings).
Congenital absence or hypoplasia of the cervix - these may be associated with urinary tract or musculoskeletal (notably spinal) abnormalities. Partial agenesis may occur; if there is a primitive uterus containing endometrium, haematometra occurs at puberty, producing cyclical abdominal pain.
In utero exposure to non-steroidal oestrogens such as diethylstilbestrol (DES) which was used widely in the USA until 1971 to prevent preterm labour and miscarriage. 1 in 1,000-1,500 exposed female fetuses develop clear cell vaginal adenocarcinoma of the vagina or cervix in the late teens or early twenties.7 Other problems include a hypoplastic T-shaped uterus as well as various gross and microscopic colposcopic abnormalities (for example, cervical rings, collars and hoods, epithelial changes and a shift in the location of the squamocolumnar junction).
Benign tumours
Polyps
These are the most common benign neoplasms of the cervix (found in 4% of the gynaecological population). They may be endocervical or cervical:
Endocervical polyps are most usually found in the fourth to sixth decade of life. They are cherry red lesions which may be single or multiple and may appear as a pedunculated lesion on a stalk of varying length.
Cervical polyps are equally benign and tend to occur as single, smooth grey-white lesions that bleed easily if touched.
Polyps tend to be asymptomatic but may also present with abnormal bleeding (such as during intercourse, heavy menstrual periods, between menstrual periods or after the menopause). Occasionally, they may grow big enough to obstruct the external os and so cause infertility. Malignancy is rare (less than 1 in 200 cases) and the malignancy tends to arise from sources beyond the cervix.
Polyps may be removed but should all be sent to histology. If the woman is asymptomatic, this can simply be done by twisting them off. Patients may be referred for this but, if it is small (less than 2 cm x 1 cm) and you are confident in carrying out this procedure, it can be done in your surgery. However, be mindful of vagally stimulated bradycardia which may need treatment with atropine. Haemorrhage may also occur and require cautery for haemostasis. Surgical dilatation and curettage, electrosurgical excision or hysteroscopic polypectomy may be performed for more persistent lesions. Occasionally, the appearance of the healed cervix following a cone biopsy can mimic a large polyp.
All patients with suspicious lesions or who are symptomatic should be referred to a specialist clinic and the lesions sent to histology.
Fibroids (myoma/leiomyoma)
When found in the cervix, fibroids (myoma/leiomyoma) are smooth, firm masses which are often solitary and tend to be small (5-10 mm in diameter). They account for about 3-9% of uterine myomata. A fibroid growing down into the cervix from higher up in the uterus is a more common situation. Symptoms relate to its size and exact location: dysuria, urgency, obstruction of the cervix and dyspareunia.
Management is guided by the size of the lesion and the age of the patient (whether she wants to retain fertility). It ranges from simple observation, to medical treatment with gonadotrophin-releasing hormone (GnRH) agonists, to surgery. The latter is tricky on account of the relative inaccessibility of these lesions and the proximity to the bladder and ureters.
Cervical endometriosis
Endometriosis in the cervix is not uncommon and usually considered to cause few symptoms. It may be apparent as blue-red or blue-black lesions 1-3 mm in diameter. Occasionally, it can cause postcoital bleeding and it may present as a mass. Unless there are significant symptoms, the vast majority of patients are managed conservatively but any patient with suspected cervical endometriosis should be referred to a gynaecologist to confirm the diagnosis and exclude more serious lesions.
More unusual tumours
Squamous papilloma.
Microglandular hyperplasia.
Papillary adenofibroma.
Haemangioma.
Mesonephric duct remnants.
Heterologous tissue.
Abnormality of form
Stenosis - this problem may be congenital or acquired and tends to occur at the level of the internal os. There are a number of causes and associations:
Diathermy excision of cervical lesions is the most common cause of stenosis (it occurs in 1.3% of cases).
Other acquired causes include radiotherapy, infection, neoplasia and atrophy following a cone biopsy.
It may also be associated with endometriosis.
Premenopausal patients present with menstrual disorders, pain and infertility, whereas postmenopausal patients may remain asymptomatic or develop symptoms over a very long period of time, after which they may present with haematometra, hydrometra or pyometra. Diagnosis is made upon failure to introduce a 1-2 mm dilator into the uterine cavity and is confirmed when a large but painless palpable uterus is found. Treatment is with ultrasound-guided dilators or with osmotic dilators such as laminaria tents (where the dried-out laminaria seaweed is packed into the cervix and slowly expands). Prostaglandin pessaries can be used to soften the cervix where access is needed for procedures such as hysteroscopy.Ectropion (previously called cervical erosion or abrasion) - this occurs when the columnar epithelium of the endocervix is displayed beyond the os:
The cervix enlarges under the influence of oestrogen and as a result the endocervical canal is everted. It is seen on examination as a red ring around the os and is so common as to be regarded as normal.
It is most commonly seen in teenagers, during pregnancy and in women on combined hormonal contraception but it can be seen at any age.
It is generally an asymptomatic condition but patients occasionally present with bleeding or excessive discharge.
Once a normal cervical smear has been confirmed (or ectropion confirmed on examination, if too young for a smear), it is actively managed only if there are symptoms. Over time, vaginal acidity promotes metaplasia to squamous epithelium when the symptoms will disappear.
After stopping any oestrogen-containing contraceptive, treatment options are controversial but include diathermy, cryotherapy, surgery with laser treatment and microwave therapy.
Nabothian cysts (Nabothian follicle/epithelial inclusion cysts/mucinous retention cysts):
Like ectropion, these mucus-filled lesions are so common as to be considered a normal part of the adult cervix. They look like multiple translucent or opaque, white or yellow lesions ranging from 2 mm to 10 mm in size.
They occur as a result of metaplasia leading to a squamous cell cover over columnar epithelium with mucus-producing crypts within it. When the mucus can no longer be expelled, a Nabothian cyst is formed.
They are asymptomatic and need no treatment. Very rarely they may be problematic if they grow very large, in which case they may be treated with cautery or cryotherapy.
Laceration:
This can occur following mechanical dilatation of the cervix; thus, cervical lacerations can complicate hysteroscopy and abortion.
Misoprostol prior to hysteroscopy reduces the risk of cervical laceration in pre-menopausal women but has no effect on postmenopausal women.8
It occurs more commonly in the presence of cervical stenosis or atrophy and may also occur during delivery.
Acute lacerations present with bleeding and need suturing once the extent of the laceration is ascertained.
Poor repair may lead to subsequent cervical incompetence.
Cervicitis
Back to contentsSymptoms - these vary from none to abnormal yellow-green discharge, bleeding (especially postcoital), dysuria.
Signs - green/yellow/opaque mucopurulent discharge. Endocervical friability (bleeds easily).
Common culprits - Neisseria gonorrhoeae, Chlamydia trachomatis, human papillomavirus, herpes simplex virus and Trichomonas vaginalis.
Treatment - antimicrobial, guided by results from swabs.
See the separate article Sexually transmitted infections for further information.
Inflammatory cervicitis can also be caused by mechanical trauma (tampons, pessaries, threads from an intrauterine device), chemical irritants (douching, spermicides), and systemic inflammatory disease such as Behçet's disease. The treatment depends on the cause.
Problems with the cervix in pregnancy
Back to contentsCervical incompetence
This is usually diagnosed in the context of a miscarriage occurring after 12-14 weeks or in premature labour. It presents as a painless dilatation of the cervix through which the membranes bulge and eventually spontaneously erupt. Diagnosis is based on a past history of second-trimester miscarriages, and ultrasound scanning may confirm shortening or funnelling of the cervix.
Treatment involves prophylactic placement of a cervical stitch (cerclage) with the aim to prevent loss of the pregnancy (an emergency procedure can also be carried out).
Cervical cerclage shows some benefit for women with evidence of a shortened cervix on physical examination but not for those without the short cervix but a previous history of pre-term birth or where the shortened cervix was only seen on ultrasound.9
Ectopic pregnancy in the cervix
The cervix is the least common site for an ectopic pregnancy, occurring in 0.2% of ectopic pregnancies. It may be seen as a bluish hue on the cervix and, rarely, a gestational sac and live fetus can be identified on ultrasonography. This is such a rare occurrence that there is no management protocol but, from the case studies available, medical termination appears to be the best option because life-threatening haemorrhage may occur.
Further reading and references
- Oscarsson MG, Wijma BE, Benzein EG; 'I do not need to... I do not want to... I do not give it priority...'--why women choose not to attend cervical cancer screening. Health Expect. 2008 Mar;11(1):26-34.
- Intimate examinations and chaperones; GMC
- Bates CK, Carroll N, Potter J; The challenging pelvic examination. J Gen Intern Med. 2011 Jun;26(6):651-7. doi: 10.1007/s11606-010-1610-8. Epub 2011 Jan 12.
- Breitkopf DM; Lateral decubitus position to facilitate pelvic examination of the patient with severe obesity. BMC Womens Health. 2021 Apr 7;21(1):143. doi: 10.1186/s12905-021-01289-2.
- Cadman L, Waller J, Ashdown-Barr L, et al; Barriers to cervical screening in women who have experienced sexual abuse: an exploratory study. J Fam Plann Reprod Health Care. 2012 Oct;38(4):214-20. doi: 10.1136/jfprhc-2012-100378.
- O'Connor M, McSherry LA, Dombrowski SU, et al; Identifying ways to maximise cervical screening uptake: a qualitative study of GPs' and practice nurses' cervical cancer screening-related behaviours. HRB Open Res. 2021 May 5;4:44. doi: 10.12688/hrbopenres.13246.1. eCollection 2021.
- Tips for screening survivors of sexual trauma
- Titus-Ernstoff L, Hatch EE, Hoover RN, et al; Long-term cancer risk in women given diethylstilbestrol (DES) during pregnancy. Br J Cancer. 2001 Jan 5;84(1):126-33. doi: 10.1054/bjoc.2000.1521.
- Polyzos NP, Zavos A, Valachis A, et al; Misoprostol prior to hysteroscopy in premenopausal and post-menopausal women. A systematic review and meta-analysis. Hum Reprod Update. 2012 Jul;18(4):393-404. doi: 10.1093/humupd/dms014. Epub 2012 Apr 27.
- The retrospective study for effectiveness of cervical cerclage in preventing recurrent preterm birth; R Seyama et al
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Jun 2028
17 Jun 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free