Lower urinary tract symptoms in women
LUTs
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Rachel Hudson, MRCGPLast updated 27 Feb 2023
Meets Patient’s editorial guidelines
In this series:Cystitis in womenRecurrent cystitis in womenUrge incontinenceOveractive bladder syndromeStress incontinenceMedicines for urinary urgency and incontinence
Lower urinary tract symptoms (LUTS) are common in women of all ages, especially between the ages of 40-60. For many women, the symptoms come and go. But for some women, the symptoms are ongoing and interfere with normal life. The symptoms may include wetting yourself (incontinence), needing to pass urine frequently, or discomfort passing urine. These and other symptoms can result in poor quality of life. Many women never tell anyone about their symptoms. Your doctor may recommend tests to look for an underlying cause. Referral to a specialist is not usually needed. Often, no specific underlying cause is found. Treatment may help to relieve symptoms.
In this article:
What is a UTI?
Continue reading below
What are lower urinary tract symptoms in women?
LUTS are divided into three groups:
Problems with the storage of urine in the bladder.
Problems passing urine.
Problems after passing urine.
Sometimes symptoms cross into more than one of these groups. Sometimes women just have symptoms from one group. Others may have symptoms from two or all groups. Some of the LUTS women may experience are:
Burning or stinging when you pass urine.
Constant lower tummy (abdominal) ache.
Needing to pass urine often (frequency).
An urgent feeling of needing to empty your bladder (urgency).
Loss of bladder control (Incontinence).
Needing to get up to urinate several times in the night.
Feeling of needing to empty your bladder even after urinating. Or, a dribble of urine after you think you have finished.
Difficulty urinating.
A slow stream of urine.
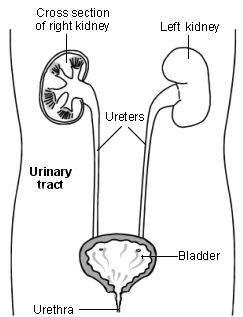
The urinary tract
What causes lower urinary tract symptoms?
There are several possible causes of LUTS. Often, no specific cause is found.
Urinary tract infection (UTI)
UTIs are very common among women. They are due to germs (bacterial infection) in the bladder. A UTI causes:
Lower tummy (abdominal) discomfort.
A soreness or burning sensation when you pass urine.
A feeling you need to pass urine more often.
A feeling that you need to pass urine urgently.
The urine may look cloudy or have blood in it. Your doctor can perform a urine test and may suggest an antibiotic medicine if needed. If you have a urine infection, you should drink plenty of fluids to help flush the germs out. Some women get repeated infections after the menopause. Hormone replacement therapy (HRT) may help.
Some women have recurrent, sometimes frequent, episodes of cystitis. Read more about recurrent cystitis.
Menopause
After the menopause, levels of a female hormone produced by your ovaries (oestrogen) fall. Because of this, some women may notice changes in their vagina and genital area after the menopause. These changes may include vaginal dryness, discomfort during sex and bladder symptoms. These can all usually be improved with treatment. Treatment options include:
Oestrogen cream or pessaries.
Lubricating gels.
See the separate leaflet called Vaginal Dryness (Atrophic Vaginitis) for more details.
Urge incontinence (detrusor instability)
Urgency is a symptom where you have a sudden urgent desire to urinate. You are not able to put off going to the toilet. In urge incontinence, urine leaks before you get to the toilet when you have urgency.
Urgency and urge incontinence are often due to an unstable or overactive bladder, or detrusor instability. (The detrusor muscle is the medical name for the bladder muscle.) Bladder training exercises are the first line of treatment. Medication may also help. Some people have mixed incontinence, which is both stress incontinence and urge incontinence.
Stress incontinence
Stress incontinence is the most common form of incontinence. It means you leak urine with actions such as coughing, laughing, sneezing or exercise. It happens when the pelvic floor muscles that support the bladder are weakened. Childbirth is a common reason for a weak pelvic floor.
The first treatment for stress incontinence is pelvic floor exercises. Surgery to tighten or support the bladder outlet can also help. Medication may be used in addition to exercises if you do not want, or are not suitable for, surgery.
Some people have mixed incontinence, which is both stress incontinence and urge incontinence. You should always see your doctor if you develop incontinence. Each type has different treatments. See the separate leaflet called Urinary Incontinence for a general overview and to understand what is likely to happen during your doctor's assessment.
Diabetes mellitus
If diabetes is not well controlled, the high sugar (glucose) levels in the blood may make you produce more urine. UTIs are also more common if you have diabetes.
Bladder stones
Stones in the bladder or kidneys usually cause other symptoms rather than LUTS. They may cause blood in the urine and severe pain when urinating.
Bladder cancer
This is also uncommon. It causes blood in the urine and is painless. In most cases, the cancer is confined to the inside lining of the bladder. Treatment of these superficial bladder cancers is relatively easy and often completely cures the cancer. If the cancer has spread into or through the muscle layer of the bladder wall then treatment is less likely to result in a complete cure but can often slow the progress of the cancer. See the separate leaflet called Bladder Cancer for more details.
Neurological conditions
Conditions such as multiple sclerosis may affect the nervous system and cause LUTS.
Medication
Sometimes medication you take can give you LUTS. Examples of medication which may do this include:
Antidepressants such as amitriptyline may sometimes make it difficult to pass urine.
'Water' tablets (diuretics) make you pass urine more frequently. They may also give you a feeling of urgency.
Lithium tablets can make you pass urine more often and with a sensation of urgency.
Continue reading below
What tests are commonly performed?
The tests you may have will depend on your symptoms.
Your doctor may want to examine your tummy (abdomen). A vaginal examination may be suggested.
Common LUTS tests performed
A urine dipstick test for infection, sugar (glucose) and blood.
A urine test to send to the hospital to confirm the dipstick findings.
A blood test for glucose to rule out diabetes.
You may have an ultrasound scan on your bladder and urinary tract. You may be referred to a specialist (urologist) for tests on your urinary system (urodynamic tests). Urodynamic studies test the working of the bladder and are used to see how the urinary system and pelvic floor work.
You may be asked to keep a diary. In your diary make a note of the times you pass urine and the amount (volume) that you pass each time. Also, make a note of the times you leak urine (are incontinent). Your doctor or nurse may have some pre-printed diary charts to give you for this purpose. Keep an old measuring jug by the toilet (you will need to urinate directly into this) so that you can measure the amount of urine you produce each time you go to the toilet.
If you have unexplained blood in your urine, you will be referred urgently to a urologist for further tests.
What self-help treatments are available?
The following may help your symptoms:
Avoid drinking too many drinks containing caffeine. Caffeine can make symptoms worse.
For a dry, sore vagina after the menopause, vaginal lubricants (for example, K-Y Jelly®) may be useful. They can be bought at a chemist.
For an overactive bladder there are bladder training exercises. Try to empty your bladder at a set time before you are desperate to go - for example, every hour. Gradually increase the interval until you can hold your urine for longer. See the leaflet called Incontinence chart.
For stress incontinence, practise pelvic floor exercises - for example, repeated clenching of the pelvic floor muscles.
Try to lose weight if you are overweight.
Try to stop smoking if you are a smoker.
If you have UTIs frequently after having sex, it may help to get up and pass urine straight after having sex. If it keeps happening, your doctor may prescribe you an antibiotic to take each time.
Continue reading below
What other treatments are available?
The treatment for LUTS will depend on the underlying cause. Often, no specific cause is found and so there is no specific treatment. Some women find that their symptoms come and go and do not cause them a great deal of bother or distress. But if your LUTS do interfere with your normal life, you should see your doctor for advice.
Continence clinics
You may be offered help at a special continence clinic which can advise about pelvic floor exercises and ways of coping with incontinence. Specialist incontinence nurses can also advise about pads and catheters.
Medication
Medicines can be effective in helping symptoms of an overactive bladder if there is not enough improvement with bladder training alone. These medicines work by blocking certain nerve impulses to the bladder which relax the bladder muscle, so increasing the bladder capacity. These medications are called antimuscarinics (or anticholinergics). There are several different types and many different brand names. They include oxybutynin, solifenacin and tolterodine.
Hormone replacement therapy
HRT can help menopausal symptoms including vaginal dryness and discomfort when you urinate.
Surgery
An operation may be required to repair or boost your pelvic floor in some cases.
You may be referred to a specialist if your symptoms do not improve after self-help measures and treatment from your doctor.
Further reading and references
- Perrotta C, Aznar M, Mejia R, et al; Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD005131.
- Chapple CR, Wein AJ, Abrams P, et al; Lower urinary tract symptoms revisited: a broader clinical perspective. Eur Urol. 2008 Sep;54(3):563-9. doi: 10.1016/j.eururo.2008.03.109. Epub 2008 Apr 8.
- Urinary incontinence and pelvic organ prolapse in women: management; NICE guideline (April 2019 - updated June 2019)
- Incontinence - urinary, in women; NICE CKS, October 2019 (UK access only)
- Urinary tract infection (lower) - women; NICE CKS, March 2023 (UK access only)
- Hoffmann TC, Bakhit M, Del Mar C; Uncomplicated urinary tract infection in women. BMJ. 2021 Mar 30;372:n725. doi: 10.1136/bmj.n725.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 26 Feb 2028
27 Feb 2023 | Latest version
12 Feb 2013 | Originally published
Authored by:
Dr Ann Robinson, MRCGP

Feeling unwell?
Assess your symptoms online for free