PSA test
Prostate specific antigen
Peer reviewed by Dr Laurence KnottLast updated by Dr Colin Tidy, MRCGPLast updated 21 Oct 2021
Meets Patient’s editorial guidelines
In this series:Prostate problemsEnlarged prostateUrinary retentionUrethral strictureChronic prostatitisLower urinary tract symptoms in men
The PSA test (prostate specific antigen) is a blood test to see if you might have prostate cancer and to monitor treatment for prostate cancer.
The PSA blood level is also increased in other conditions. So having an increased PSA test result does not mean that you have prostate cancer. Experts disagree on how useful the PSA test is. There is a lot of ongoing research about PSA. At the moment there is no national screening programme for prostate cancer in the UK.
In this article:
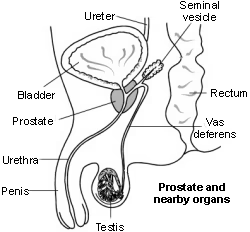
Cross-section diagram of the prostate and nearby organs
Continue reading below
What is a PSA test?
The PSA test (prostate specific antigen) is a blood test that measures the level of PSA in your blood. PSA is made by the prostate gland. The PSA level in your bloodstream is measured in nanograms per millilitre (ng/mL).
When you have a PSA test, you should not have:
An active urine infection.
Produced semen during sex or masturbation (ejaculated) in the previous 48 hours.
Exercised heavily in the previous 48 hours.
Had a prostate biopsy in the previous six weeks.
Had an examination of the back passage with a gloved finger (a digital rectal examination) in the previous week.
Had receptive anal intercourse for a period of 48 hours before a PSA test. This is an essential requirement for gay, bisexual, and other men who have sex with men.
Each of these may produce an unusually high PSA result.
If you decide to have a PSA test, your doctor will give you a digital rectal examination to feel the prostate gland. This is to find out if the prostate gland is enlarged or feels abnormal in any way.
In England, the PSA test is available free to any well man aged 50 and over who requests it. GPs should use their clinical judgement to manage men with symptoms and those aged under 50 who are considered to have higher risk for prostate cancer.
Patient picks for Blood tests
What is a normal result?
The normal range changes as you get older.
PSA Cut-off Values | |
|
|
40-49 | 2.5 micrograms/litre or higher |
50-59 | 3.5 micrograms/litre or higher |
60-69 | 4.5 micrograms/litre or higher |
70-79 | 6.5 micrograms/litre or higher |
There are no age-specific reference limits for men older than 80 years of age. Whether you are referred will depend on your discussion with your doctor.
The higher the level of PSA, the more likely it is to be a sign of cancer.
Continue reading below
What are the benefits and limitations of a PSA test?
Benefits of PSA testing
PSA testing may lead to prostate cancer being detected earlier, before symptoms develop.
Detecting prostate cancer early before symptoms develop may improve outcome (prognosis) and improve the chance of complete cure.
Limitations and risks of PSA testing
False negative result: about 15 out of 100 men with a negative PSA test may have prostate cancer.
False positive result: about 75 out of 100 men with a positive PSA test have a normal prostate biopsy (ie no evidence of cancer).
Therefore a false positive PSA test may lead to unnecessary investigations, such as a prostate biopsy, and there may be side-effects from this investigation, such as bleeding or infection.
A positive result may also lead to unnecessary treatment. Many prostate cancers are slow growing and may not become evident during your lifetime. Side-effects of treatment are common and can be serious, such as urinary incontinence and sexual problems.
What causes a raised PSA level?
A raised PSA level may mean you have prostate cancer but about two out of three men with a raised PSA level will not have prostate cancer.
Other conditions may also cause a raised PSA level, including:
Inability to pass urine, causing an enlarged bladder (acute retention of urine).
Older age.
Transurethral resection of the prostate (TURP) operation. TURP is a prostate operation used if you have benign enlargement of the prostate.
If you have a tube (catheter) to help pass urine
Continue reading below
What happens after a PSA test?
If your PSA level is not raised
You are unlikely to have cancer. No immediate further action is needed but you may need further tests to confirm the result.
If your PSA level is slightly raised
You probably do not have cancer. You might need further tests, including more PSA tests.
If your PSA level is definitely raised
Editor’s note
Dr Sarah Jarvis, 15th December 2021
Updated guidance from NICE
In December 2021, the National Institute for Health and Care Excellence (NICE) updated its guidance on referrals for possible cancer. They recommend that the GP should consider referring men urgently to a Urology Specialist, for an appointment within two weeks, depending on their age, risk factors, preferences and level of PSA. The levels they recommend are outlined in the list under 'What is a normal result?' above.
You can find out more about the recommendations made by NICE from the link in the further reading section below.
Your GP will refer you to see a doctor who is a specialist, for you to have further tests to find out if you have prostate cancer. The specialist will discuss with you the options for further investigations, which may include a sample taken (a biopsy) of your prostate gland and an MRI scan.
If prostate cancer is found, what are my options?
Further reading and references
- Prostate cancer risk management programme: overview; Public Health England
- Moyer VA; Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012 Jul 17;157(2):120-34. doi: 10.7326/0003-4819-157-2-201207170-00459.
- Ilic D, Neuberger MM, Djulbegovic M, et al; Screening for prostate cancer. Cochrane Database Syst Rev. 2013 Jan 31;1:CD004720. doi: 10.1002/14651858.CD004720.pub3.
- Suspected cancer: recognition and referral; NICE guideline (2015 - last updated October 2023)
- Prostate Cancer; NICE CKS, June 2021 (UK access only)
- Prostate cancer: diagnosis and management; NICE Guidance (2019 - last updated December 2021)
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 20 Oct 2026
21 Oct 2021 | Latest version

Feeling unwell?
Assess your symptoms online for free

