Labour - active management and induction
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 30 Jan 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Continue reading below
Management of labour
The active management of labour was pioneered by K O'Driscoll in 1969, as a means of reducing the number of prolonged labours1 . Its aim was to keep labour to fewer than 12 hours and operative delivery rates to a minimum.
It was originally designed for primiparous women with singleton pregnancies at term, in spontaneous labour.
Important information |
|---|
Active management of labour has been modified significantly over time but the core principles remain: Early diagnosis following strict criteria, by a senior midwife. Vaginal examination hourly for three hours, then every two hours, at least. This allows the rate of progress to be plotted on a partogram. Amniotomy one hour after admission2 . Augmentation with Syntocinon® if not dilating at rate of 1 cm/hour3 4 5 . Women not in labour should be sent home. Personal, psychological support for the woman6 . Liberal use of epidural anaesthesia. Regular rounds by the obstetrician. Early cord clamping and controlled cord traction with uterotonic7 . Antenatal education classes. Regular audit of labour ward process and outcomes. |
'Active management' was not designed to lower caesarean section rates, but may have decreased the number of sections performed for dystocia - failure to progress8 . This effect was most significant in Dublin, where it was first used, but this success has not been matched in other units.
Important information |
|---|
NB: National Institute for Health and Care Excellence (NICE) guidelines do not recommend routinely offering active management of labour9 . |
Elements of active management are retained within normal obstetric care - eg, continuous support for the labouring woman and regular review by the obstetrician.
Cochrane reviews have showed that early intervention with amniotomy and oxytocin (when there is delay in established first stage of labour) appears to be associated with a modest reduction in the rate of caesarean section over standard care2 .
The partogram
Back to contentsDublin partogram
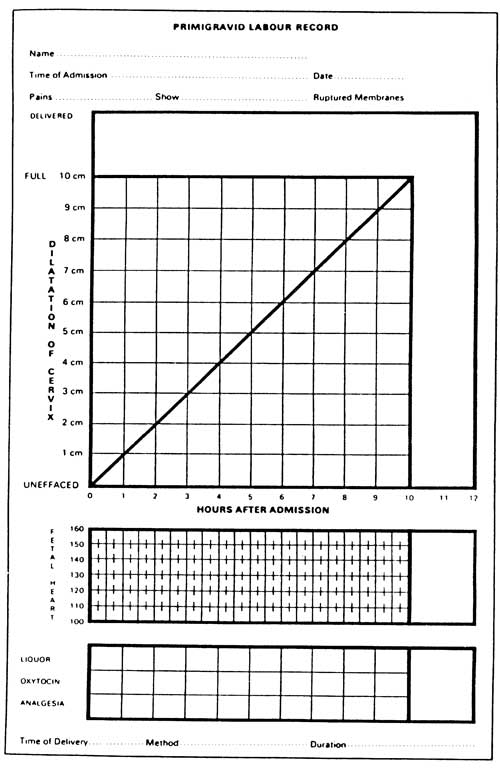
The partogram is used to chart the progress of the woman in labour. If cervical dilatation is less than expected or stops (progress drops below the 'action line'), augmentation may be required. Other important parameters are also recorded - eg, presence of meconium staining in the liquor and perception of strength of contractions. Many advocate its use; however in the absence of any active management of labour, there is little evidence of a positive effect on labour outcomes10 .
Continue reading below
Induction of labour
Back to contentsInduction is the process of starting labour by uterine stimulation. It should be used when it is thought that the baby will be safer delivered than it is in utero. Induction needs to be clearly distinguished from augmentation of labour, which is the enhancement of uterine contractions once labour has started.
There has been an increase in the rate of inductions from 20.3% in 2006-7 to 33% in 2019-2011 .
Recent research provides no evidence that induction labour increases the caesarean section or compromises neonatal outcomes as compared with expectant management12 . Concerns over increased risk of failed induction in women with a Bishop's score from 3 to 6 seem unwarranted.
Other research supports this finding and in addition decreased pregnancy-related hypertension in multiparous and nulliparous women, but increased time from admission to delivery for both nulliparous (1.3 hours; 95% CI 0.2-2.3) and multiparous women (3.4 hours; 95% CI 3.2-3.6)13 .
Indications for induction
The Royal College of Obstetricians and Gynaecologists (RCOG) and the NICE guidelines define the use of induction in clinical practice14 :
It should be offered to women with healthy pregnancy after 41 weeks. Risk of stillbirth increases from 3/3,000 at 42 weeks to 6/3,000 at 43 weeks. Randomised controlled trials suggest that elective induction of labour at 41 weeks of gestation and beyond may be associated with a decrease in both the risk of caesarean section and of meconium-stained amniotic fluid.
It should be offered to women whose pregnancy is complicated by diabetes, before term.
In women with pre-labour ruptured membranes after 37 weeks (6-19% of pregnancies), they should be given a choice of either immediate induction, or watchful waiting for up to maximum of four days. 84% labour within 24 hours, increasing by a further 5% every 24 hours after. Beyond four days, risk of infection outweighs any potential benefit to mother or child.
Important information |
|---|
NB: according to the 2020 MBRRACE-UK report on perinatal mortality, women from some minority ethnic backgrounds or who live in deprived areas have an increased risk of stillbirth and may benefit from closer monitoring and additional support if they do not have spontaneous labour before 41 weeks15 . The report showed that across all births (not just those induced): Compared with white babies (34/10,000), the stillbirth rate is: More than twice as high in black babies (74/10,000). Around 50% higher in Asian babies (53/10,000). The stillbirth rate increases according to the level of deprivation in the area the mother lives in, with almost twice as many stillbirths for women living in the most deprived areas (47/10,000) compared with the least deprived areas (26/10,000). |
The most common reasons for inducing labour are:
Prolonged pregnancy - 70% of such cases are induced after 41 weeks, often at the mother's request. The obstetrician will usually agree if the cervix is ripe.
Suspected intrauterine growth restriction.
Hypertension and pre-eclampsia - approximately 50% of women with this problem are induced.
Planned time of delivery in the best interests of the baby - eg, cardiac abnormalities which may need immediate surgery after birth.
Pre-induction check-list
Prior to induction:
Need to check lie and position of fetus.
Volume of amniotic fluid.
Tone of uterus.
Ripeness of cervix; this is the best predictor of readiness for induction and can be scored using Bishop's system: If the score is >8, the probability of successful delivery with induction is the same as spontaneous onset of labour.
Contra-indications to induction
These are the same as for vaginal delivery. Absolute contra-indications include16 :
Severe degree of placenta praevia.
Transverse fetal lie.
Severe cephalopelvic disproportion.
Cervix <4 on Bishop's score - can be overcome by ripening with prostaglandins.
Relative contra-indications include:
Active primary genital herpes infection.
High and floating fetal head (risk of prolapsed cord).
Induction procedure
The procedure should be fully discussed with the mother, explaining the technique to be used and any possible side-effects and consequences of failure (caesarean section). She needs to give her informed consent, possibly in writing or, if not, a signed note made in the woman's records.
Assess fetal maturity.
Re-check presentation and position of fetus just before induction.
Induction procedure
Methods used include:
Membrane sweeping.
Prostaglandin gel or pessary.
Oxytocin with/or without artificial rupture of membranes.
The most common method of induction in the UK is placing prostaglandin gel or pessary high in the vagina (not cervix). The drug is absorbed through vaginal and cervical epithelium and delivered to the uterus via the bloodstream. The obstetrician or midwife should stay with the woman for 20-30 minutes with cardiotocographic monitoring of the fetus in case of myometrial overreaction.
Complications of induction
It may fail and require caesarean section. All the complications of a normal vaginal delivery, plus:
Uterine hyperstimulation; fetal distress and hypoxic damage to the baby.
Uterine rupture, especially in multiparous women.
Intrauterine infection with prolonged membrane rupture without delivery (less likely if labour occurs within 12 hours).
Prolapsed cord can occur with first rush of amniotic fluid, if the presenting part is not well engaged.
Further reading and references
- Dresang LT, Yonke N; Management of Spontaneous Vaginal Delivery. Am Fam Physician. 2015 Aug 1;92(3):202-8.
- WHO recommendations: Induction of labour at or beyond term; World Health Organization, 2018
- O'Driscoll K, Jackson RJ, Gallagher JT; Prevention of prolonged labour. Br Med J. 1969 May 24;2(5655):477-80.
- Wei S, Wo BL, Qi HP, et al; Early amniotomy and early oxytocin for prevention of, or therapy for, delay in first stage spontaneous labour compared with routine care. Cochrane Database Syst Rev. 2013 Aug 7;(8):CD006794. doi: 10.1002/14651858.CD006794.pub4.
- Selin L, Wennerholm UB, Jonsson M, et al; High-dose versus low-dose of oxytocin for labour augmentation: a randomised controlled trial. Women Birth. 2018 Oct 16. pii: S1871-5192(18)30363-9. doi: 10.1016/j.wombi.2018.09.002.
- Gaudernack LC, Froslie KF, Michelsen TM, et al; De-medicalization of birth by reducing the use of oxytocin for augmentation among first-time mothers - a prospective intervention study. BMC Pregnancy Childbirth. 2018 Mar 27;18(1):76. doi: 10.1186/s12884-018-1706-4.
- Boie S, Glavind J, Velu AV, et al; Discontinuation of intravenous oxytocin in the active phase of induced labour. Cochrane Database Syst Rev. 2018 Aug 20;8:CD012274. doi: 10.1002/14651858.CD012274.pub2.
- Bohren MA, Hofmeyr GJ, Sakala C, et al; Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017 Jul 6;7:CD003766. doi: 10.1002/14651858.CD003766.pub6.
- Begley CM, Gyte GM, Devane D, et al; Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2019 Feb 13;2:CD007412. doi: 10.1002/14651858.CD007412.pub5.
- Brown HC, Paranjothy S, Dowswell T, et al; Package of care for active management in labour for reducing caesarean section rates in low-risk women. Cochrane Database Syst Rev. 2013 Sep 16;(9):CD004907. doi: 10.1002/14651858.CD004907.pub3.
- Intrapartum care for healthy women and babies; NICE Guideline (Dec 2014 - updated Dec 2022) (Replaced by NICE NG235)
- Lavender T, Cuthbert A, Smyth RM; Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev. 2018 Aug 6;8:CD005461. doi: 10.1002/14651858.CD005461.pub5.
- NHS Maternity Statistics, England 2019-20; NHS Digital, October 2020
- Bernardes TP, Broekhuijsen K, Koopmans CM, et al; Caesarean section rates and adverse neonatal outcomes after induction of labour versus expectant management in women with an unripe cervix: a secondary analysis of the HYPITAT and DIGITAT trials. BJOG. 2016 Aug;123(9):1501-8. doi: 10.1111/1471-0528.14028. Epub 2016 May 13.
- Souter V, Painter I, Sitcov K, et al; Maternal and Newborn Outcomes with Elective Induction of Labor at Term. Am J Obstet Gynecol. 2019 Jan 29. pii: S0002-9378(19)30253-4. doi: 10.1016/j.ajog.2019.01.223.
- Inducing labour; NICE guideline (November 2021)
- MBRRACE-UK Perinatal Mortality Surveillance Report; UK Perinatal Deaths for Births from January to December 2018, December 2020
- Chamberlain G, Zander L; ABC of labour care: induction. BMJ. 1999 Apr 10;318(7189):995-8.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 29 Jan 2027
30 Jan 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free