Neurological examination of the lower limbs
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 1 Dec 2021
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
There is more than one way of performing a neurological examination and a clinician should develop their own technique. Poor technique will fail to elicit signs or will produce false results.
See the separate Neurological History and Examination article which covers the basic principles of examination and technique.
Continue reading below
Inspection of the lower limbs1
Note whether there is any damage to the feet. Neuropathic ulcers and neuropathic joints develop because of a lack of pain perception. Pain is a protective mechanism. When inspecting the motor system, the following points should be assessed:
Note the resting posture. Establish whether there is unusual rotation or posture of a joint. Note whether the patient is symmetrical.
Look for muscle wasting or hypertrophy: note whether it is focal or diffuse.
Look for involuntary movements such as tremor, tics, myoclonic jerks, chorea or athetosis.
Look for muscle fasciculation (a sign of lower motor neurone disease process). These are subcutaneous twitches over a muscle belly at rest. Tapping the belly may stimulate fasciculation.
Lower limbs examination of the sensory system
Examination of the lower limbs may be performed more easily with the patient lying on a couch.
Examination of each of the sensory modalities1
Light touch
Use the light touch of a finger, a piece of cotton wool or a piece of tissue paper.
It is important to touch and not to stroke, as a moving sensation, such as rubbing and scratching, is conducted along pain pathways.
Ask the patient to close their eyes and tell you when they feel you touching them.
Compare each limb in the same position.
Keep the timing of each touch irregular to avoid anticipation by the patient.
A logical progression is required. You may want to start testing over the groin and to move down the front of the leg and up the posterior side as this moves progressively from L1 to S3 dermatomes.
Note any areas of hypoaesthesia or dysaesthesia.
Sharp touch (pinprick)
Test using a dedicated disposable pin. A disposable hypodermic needle is too sharp.
Use the sternal area to establish a baseline for sharpness before you begin.
Follow the same progression as with light touch with the patient's eyes closed, comparing both lower limbs.
Ask the patient to report hypoaesthesia (feels blunter) or hyperaesthesia (feels sharper).
Temperature
This is often overlooked but it can be important.
An easy and practical approach is to touch the patient with a tuning fork, as the metal feels cold.
Compare the quality of temperature sensation on arms, face, trunk, hands, legs and feet.
Containers of warm and cool water may be used for more accurate assessment. Ask the patient to distinguish between warm and cool on different areas of the skin with their eyes closed.
Joint position sense (proprioception)
Test at the interphalangeal joint of the big toe.
Hold the proximal phalanx with one thumb and finger and hold the medial and lateral sides of the distal phalanx with the other. Move the distal phalanx up and down, showing the patient the movement first.
Ask the patient to close their eyes and move the distal phalanx up and down randomly. Ask the patient to tell you the direction of movement each time.
Test on both feet.
If there is an abnormality, move backwards to the metatarsophalangeal joint and so on until joint position sense is normal.
Vibration sense
Use a 128 Hz tuning fork and ensure the tuning fork is vibrating.
Place it on the sternum to start with so that the patient can feel the sensation.
Then place it on the big toe.
If no vibration is sensed, move backwards to the bony malleolus of the ankle, the tibial shaft and tuberosity and the anterior iliac crest.
Asking the patient to tell you when the tuning fork stops vibrating can be helpful if there is doubt that their vibration sense is intact.
2-point discrimination
This test is not usually performed on the soles of the feet because the distinguishing distance is usually much greater than that on the fingers.
Interpreting the findings
The site of any lesion can be determined by looking at the pattern of any dysfunction found. The dermatomal (segmental) and peripheral nerve innervation is labelled below.
Neurological Examination
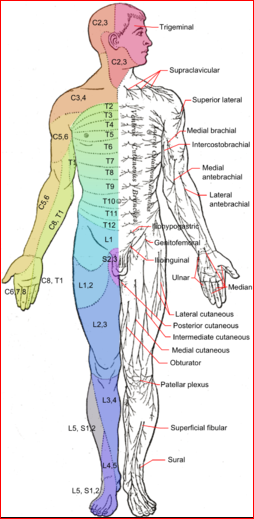
Häggström, Mikael (2014). "Medical gallery of Mikael Häggström 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 2002-4436. Public Domain
All of the sensory modalities can be affected in peripheral neuropathies and nerve injuries, radiculopathy due to disc lesions and spinal injuries.
If an individual nerve or sensory root is affected, all sensory modalities can be reduced.
If there is a spinal cord lesion, there may not be equal diminution across all of the sensory modalities: light touch, vibration and joint position sense may remain intact while sharp touch and temperature are lost. This is because the lateral spinothalamic pathways may be damaged while the dorsal columns remain intact.
Problems with joint position sense or vibration usually occur distally first. Joint position sense is also required for balance, gait and co-ordination.
Vibration sense can be lost before joint position sense in peripheral neuropathy or myelopathy affecting the dorsal columns.
Vibration sense over the ankles is often diminished or lost in elderly people with no apparent neurological lesion.
The distal parts of the limbs tend to be affected in polyneuropathy, the legs usually being involved before the arms. A 'glove and stocking' effect is produced.
Continue reading below
Lower limbs examination of the motor system2
Tone
Tone is the resistance felt when a joint is moved passively through its normal range of movement. Hypertonia is found in upper motor neurone lesions; hypotonia is found in lower motor neurone lesions and cerebellar disorders.
Clonus is rhythmic and involuntary muscle contraction that can be provoked by stretching a group of muscles.
Test tone:
Ask the patient to let their legs 'go floppy'.
Internally and externally rotate the 'floppy' leg. Assess for any increased or reduced tone.
Then lift the knee off the bed with one of your hands. Note whether the ankle raises off the bed as well, signifying increased tone.
Test for ankle clonus:
Flex the patient's knee, resting the ankle on the bed.
Dorsiflex the foot quickly and keep the pressure applied.
You will be able to see the foot moving up and down if clonus is present.
Power
A robust assessment of power is required.
The Medical Research Council (MRC) has a recommended grading system for power (see table). It has been shown to have good reliability although doubts have been expressed over the wide range of grade 43 .
The manual muscle testing is scored differently with 4 - Good: full ROM against gravity with moderate resistance, and 5 - Normal: full ROM against gravity with maximum resistance4 .
Get the patient to contract the muscle group being tested and then you as the examiner try to overpower that group.
Test the following:
Hip flexion, extension, adduction and abduction.
Knee flexion and extension.
Foot dorsiflexion, plantar flexion, eversion and inversion.
Toe plantar flexion and dorsiflexion.
MRC scale for muscle power
0 | No muscle contraction is visible. |
1 | Muscle contraction is visible but there is no movement of the joint. |
2 | Active joint movement is possible with gravity eliminated. |
3 | Movement can overcome gravity but not resistance from the examiner. |
4 | The muscle group can overcome gravity and move against some resistance from the examiner. |
5 | Full and normal power against resistance. |
Deep tendon reflexes
Ensure that the patient is comfortable and relaxed and that you can see the muscle being tested.
Use a tendon hammer to strike the tendon of the muscle and look for muscle contraction.
Compare both sides.
Reflexes can be hyperactive (+++), normal (++), sluggish (+) or absent (-). ± is used when the reflex is only present on reinforcement (see below).
In the lower limbs:
Test the knee jerk (L3, L4): flex the patient's knee and support it by using one of your hands in their popliteal fossa. Elicit the reflex by tapping just below the patella.
Test the ankle jerk (S1): with the patient lying down, flex their knee and dorsiflex their ankle, at the same time rotating their leg slightly laterally. Elicit the reflex by tapping over the Achilles tendon just above the heel. If this is difficult to elicit, an alternative method is to ask the patient to kneel on a chair, facing the back of the chair, so that their feet are dangling off the seat of the chair. Tap over the same area in this position.
If a reflex is difficult to elicit, try 'reinforcement' (the Jendrassik manoeuvre). Ask the patient to flex their fingers and interlock them with one palm facing upwards and the other facing downwards. Then ask them to try to pull their fingers apart just before you strike the tendon.
Interpretation
Upper motor neurone lesions usually produce hyperreflexia.
Lower motor neurone lesions usually produce a diminished or absent response.
It may be normal to have reduced or absent ankle reflexes in some elderly people, although the frequency and significance of this is disputed.
Isolated loss of a reflex can point to a radiculopathy affecting that segment - eg, loss of ankle jerk if there is an S1 disc prolapse.
Superficial tendon reflexes
In the lower limbs, this is the plantar response.
To elicit this, the patient should be lying down with their legs extended.
Use a blunted point and run this along the lateral border of the foot, starting at the heel and moving towards the big toe.
Stop on the first movement of the big toe.
An extensor plantar response (upgoing big toe) is pathological and signifies an upper motor neurone lesion.
Examination of co-ordination
The cerebellum helps in the co-ordination of voluntary, automatic and reflex movement. Tests of cerebellar function in the lower limbs require normal power, tone and sensation to be valid and include:
The heel-shin test:
Ask the patient to lift one of their legs and flex it at the knee, keeping the other leg straight.
They should then place the heel of the flexed leg on the knee of the other leg and run it down the shin towards the ankle and back again towards the knee.
Ask them to repeat this a number of times.
The heel-toe test:
This tests balance mechanisms that rely on the cerebellar, vestibular and proprioceptive systems.
The patient either needs to be barefoot or wearing flat shoes.
They should walk in a straight line so that the heel of the second foot touches the toes of the first foot. This should be repeated so that the heel of the first foot then touches the toes of the second foot, etc, each time with the patient moving forward.
Look at how well they are able to perform this. Is there any staggering which would suggest a lesion of the cerebellum?
Romberg's test:
This also tests balance mechanisms that rely on the cerebellar, vestibular and proprioceptive systems.
Ask the patient to keep their eyes open and stand with their feet together, arms by their sides.
Then ask them to maintain this position when they close their eyes.
Patients who have cerebellar lesions often cannot stand in this position, even with their eyes open. If balance is only lost when the eyes are closed, this signifies a proprioceptive or vestibular lesion.
Be ready to catch the patient by standing behind.
Examining the lower limbs and gait
No neurological examination, especially of the lower limbs, is complete without observing gait.
This is an enormous topic and there are separate articles discussing Abnormal Gait and Gait Abnormalities in Children.
Also, watch the patient as they rise from the chair to walk and note any abnormality of movement.
Further reading and references
- Primary Care Neurology Society
- Neurological examination; Geeky medics (accessed November, 2021)
- Neurological examination; Oxford medical examination (OME)
- Shahrokhi M, Asuncion RMD; Neurologic Exam
- Compston A; Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty's Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O'Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain. 2010 Oct;133(10):2838-44. doi: 10.1093/brain/awq270.
- Naqvi U, Sherman Al; Muscle Strength Grading
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 30 Nov 2026
1 Dec 2021 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free