Pressure ulcers
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 22 May 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Pressure sores article more useful, or one of our other health articles.
In this article:
Synonyms: pressure sores, bed sores, decubitus ulcers
Continue reading below
What are pressure ulcers?
Pressure ulcers occur when skin and underlying tissues are placed under pressure that impairs blood supply, leading to tissue damage. Pressure ulcers may present as persistently red, blistered, broken or necrotic skin and may extend to underlying structures - eg, muscle and bone. A pressure ulcer may be caused by pressure, shear, friction or a combination of these. The cost of treating a pressure ulcer is huge and depends upon its severity. Costs increase with ulcer severity because the time to heal is longer and the incidence of complications is higher in more severe cases.
It has been estimated that treating pressure damage costs the NHS £3.8 million every day.1
Pressure sore
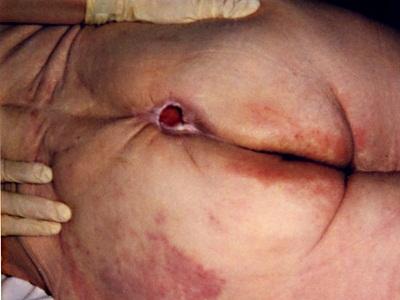
© Mennfield, via Wikimedia Commons
By Mennfield, via Wikimedia Commons
Risk factors
Pressure ulcers are caused by pressure and/or shear forces over a bony prominence in the presence of a number of risk factors, the most important of which is immobility.
Other conditions that increase the risk include:
Cardiovascular disease.
Hip fracture and hip surgery.
Limb paralysis.
Lower limb oedema.
Malignancy.
Risk assessment
The use of pressure ulcer risk assessment tools or scales is a component of the assessment process used to identify individuals at risk of developing a pressure ulcer.
However, risk assessment tools should only be used as an aide-mémoire and should not replace clinical judgment.
Commonly used assessment scales include the Norton, Braden and the Waterlow scales.
The Braden Risk Assessment Scale is a scale made up of six subscales: sensory perception, moisture, activity, mobility, nutrition, friction/shear. Each item is scored between 1 and 4. The lower the score, the greater the risk.2
However, there is little evidence to suggest that the use of structured, systematic pressure ulcer risk assessment tools reduces the incidence of pressure ulcers. 3
Assessment of pressure ulcers 4
Back to contentsPressure ulcers can develop in any area of the body. In adults, damage usually occurs over bony prominences, such as the sacrum. Patients with pressure ulcers should receive an initial and ongoing assessment which should include:
Pressure ulcers and the person's general physical condition are very closely related and the two should be assessed together. Health status includes:
Comorbidities.
Nutrition.
Pain.
Continence.
Neurological (sensory impairment, level of consciousness, cognitive status).
Blood supply.
Mobility.
Signs of local or systemic infection.
Medication.
Previous pressure damage.
Psychological and social factors.
Ulcer assessment: should be supported by photography (calibrated with a ruler) and tracings. Ulcer assessment should include:
Cause of ulcer.
Site/location.
Dimensions of ulcer.
Stage or grade (see 'Classification system', below).
Exudate amount and type.
Local signs of infection.
Pain.
Wound appearance.
Surrounding skin.
Undermining/tracking (sinus or fistula).
Odour.
Reassessment of the ulcer should be performed at least weekly but may be required more frequently. The overall goals are to achieve a healthy wound bed and promote healing.
European Pressure Ulcer Advisory Panel grading system
Grade 1: non-blanchable erythema of intact skin. Discolouration of the skin, warmth, oedema, induration or hardness may also be used as indicators, particularly on individuals with darker skin - in whom it may appear blue or purple.
Grade 2: partial-thickness skin loss involving epidermis, dermis, or both. The ulcer is superficial and presents clinically as an abrasion or blister. Surrounding skin may be red or purple.
Grade 3: full-thickness skin loss involving damage to, or necrosis of, subcutaneous tissue that may extend down to, but not through, underlying fascia.
Grade 4: extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures, with or without full-thickness skin loss. Extremely difficult to heal and predisposes to fatal infection.
Unstageable (depth unknown): full-thickness tissue loss in which the base of the ulcer is covered by slough and/or eschar in the wound bed, resulting in the true depth, and therefore Category/Stage, being unable to be determined.
The National Institute for Health and Care Excellence (NICE) has produced a quality standard which covers the prevention, assessment and management of pressure ulcers in all settings, including hospitals, care homes (with and without nursing) and people's own homes.5
Continue reading below
Pressure ulcer treatment and management6
Back to contentsPressure ulcers are often difficult to heal, painful and impact negatively on the individual's quality of life.7
Patients with extensive superficial pressure ulcers, Grade 3 or 4 pressure ulcers or those that are deteriorating should be referred to a specialist service.
Healing is not usually a fast process. However, as long as the patient has adequate pressure redistribution, good nutrition and appropriate wound management, the ulcer will heal in most cases.
Treatment includes:
Repositioning of the patient.
Treatment of concurrent conditions which may delay healing.
Pressure-relieving support surfaces such as beds, mattresses, overlays or cushions.
Local wound management using modern or advanced wound dressings and other technologies.
Patients with identified Grade 1 pressure ulcers are at a significant risk of developing more severe ulcers and should receive interventions to prevent deterioration.
Pain relief:
Pain is often significant and disabling for those with pressure ulcers.
Paracetamol may be sufficient but patients often require stronger analgesia.
Non-steroidal anti-inflammatory drugs may increase peripheral oedema and are inappropriate for patients with pressure ulcers.
Pain relief may need to be increased for dressing changes.
Patients may require referral to a pain clinic.
Infection control:
All pressure ulcers are colonised with bacteria. Most local infection can be managed using antimicrobial wound products; systemic antibiotics should not be used routinely for local infection.
Reduce risk of infection and enhance wound healing by hand washing, wound cleansing and debridement. Protect from exogenous sources of contamination - eg, faeces.
At the time of dressing, cleaning wounds with sterile water, saline or a topical antiseptic can reduce the bacterial burden and the risk of infection.
If purulent material or foul odour is present, more frequent cleansing and possibly debridement are required.
The simplest method for debriding necrotic tissue involves careful use of a sterile scalpel with adequate analgesia or anaesthesia. Alternative approaches include the use of topical hydrating products, such as hydrogels, cadexomer iodine beads or larval therapy.
Systemic antibiotics are required for patients with clinical evidence of systemic sepsis, spreading cellulitis or underlying osteomyelitis.4
NB: do not offer systemic antibiotics to adults based only on positive wound cultures without clinical evidence of infection.4
Malnutrition and/or dietary deficiency can adversely affect wound healing.8
However, there is currently no clear evidence of a benefit associated with nutritional interventions for either the prevention or treatment of pressure ulcers.9
Nutritional supplements should not be offered specifically to prevent a pressure ulcer in adults whose nutritional intake is adequate.4
It is recommended that high-calorie, high-protein nutritional supplements be offered in addition to the usual diet to adults with nutritional risk and pressure ulcer risk, if nutritional requirements cannot be achieved by dietary intake.6
There is no evidence that electromagnetic therapy (EMT), in which electrodes produce an electromagnetic field across the wound, improve healing of pressure ulcers.10
Mobility and positioning
Patients at risk of pressure ulcer development should be positioned to minimise pressure, friction, shear and the potential for further tissue damage.11 Patients who can move independently should be encouraged and enabled to do so.
Patients should be repositioned in such a way that pressure is relieved or redistributed.
All patients with pressure ulcers should actively mobilise, change their position or be repositioned frequently.
Passive movements should be considered for patients with pressure ulcers who have compromised mobility.
Avoid positioning individuals directly on pressure ulcers or bony prominences.
Seating should support pressure redistribution: chairs should provide appropriate support taking into account the person's body size, shape, posture, mobility, and lifestyle needs.6
Pressure relief6
Pressure-relieving equipment - eg, alternating pressure systems - redistributes the load or relieves the pressure at regular intervals. Pressure-reducing equipment redistributes pressure by spreading the weight over a larger surface area - eg, mattresses, cushions and dynamic air loss systems.
Patients with pressure ulcers should have access to appropriate pressure-relieving support surfaces which should be chosen on an individual basis depending on the needs of the individual for pressure redistribution.
It is currently recommended that:
A high-specification reactive foam mattress be used rather than a non-high-specification reactive foam mattress for all individuals assessed as being at risk for pressure ulcer development.
An active support surface (overlay or mattress) be used for individuals at higher risk of pressure ulcer development when frequent manual repositioning is not possible.
NB: ring or doughnut-shaped devices should not be used, as the edges of these devices create areas of high pressure that may damage tissue.
Dressings and topical agents
There is no conclusive research evidence to guide clinicians' decision-making about which dressings are most effective in pressure ulcer management.12
The ideal dressing should be easy to apply and remove, have low allergenic potential, be sterile and impermeable to micro-organisms, provide a moist environment but remove excess exudate, reduce pain and not add to wound debris.
Excess loose slough and exudate should be removed prior to a dressing change.
Modern dressings (eg, hydrocolloids, hydrogels, foams, films, alginates, soft silicones) should be used in preference to basic dressing types - eg, gauze, paraffin gauze and simple dressing pads.
Dressings that promote a warm, moist wound healing environment should ideally be used to treat Grade 2, 3 and 4 pressure ulcers.
Barrier creams should not be used with superficial pressure ulcers.
Products for wound management, listed in the table below, are currently widely available for the management of pressure ulcers.
Products for the management of wounds
Alginates: | these are often used for ulcers with moderate-to-heavy exudate. |
Cadexomer iodine: | this works well for sloughy or infected wounds. |
Films: | these work best on epithelialising wounds with low exudate. |
Foams: | different foams have different levels of absorbency. They are best used on granulating wounds. |
Hydrocolloids: | these may be used for most types of wounds with low-to-moderate exudate. Not suitable for infected wounds. |
Hydrogel: | this provides moisture to dry, sloughy or necrotic wounds and assists autolytic debridement. Can be used on wounds with low exudate. Not suitable for infected wounds. |
Silver: | silver is an antibacterial and is generally found as a composite dressing with other products - eg, alginates, foams, hydrocolloids. Use on infected wounds. |
Soft polymers: | these are non-adherent and best used on granulating wounds. |
Debridement4
An assessment of the need to debride a pressure ulcer in adults should be undertaken, which takes into consideration:
The amount of necrotic tissue.
The grade, size and extent of the pressure ulcer.
Patient tolerance.
Any comorbidities.
Debridement may be autolytic (see below), mechanical (allowing a dressing to become moist and then wet before manually removing the dressing), or surgical:
The presence of devitalised tissue delays the healing process.
Superficial pressure ulcers may benefit from autolytic debridement techniques, which use the body's own enzymes and moisture to rehydrate, soften and liquefy hard eschar and slough.
Autolytic debridement can be achieved with the use of occlusive or semi-occlusive dressings which maintain wound fluid in contact with the necrotic tissue.
For individuals who are terminally ill or with other comorbidities, overall quality of life should be considered before deciding whether and how to debride.
Debrisoft® is cost-saving in most analyses compared with hydrogel, saline and gauze.13
NICE recommends that the Debrisoft® pad can be an option for debridement in wound management in the community.14
For deep pressure ulcers not responding to standard care, surgery can offer a rapid closure for some patients. This is usually undertaken by plastic surgeons and often involves creating rotational flaps.
Prognosis
Back to contentsPressure ulcers are often slow to heal because of continued adverse factors such as pressure or poor nutrition.
May spread to deep tissues and also cause localised infection, including osteomyelitis and systemic infection.
The presence of pressure ulcers is associated with a two-fold to four-fold increased risk of death but this is because pressure ulcers are a marker for underlying disease severity and other comorbidities.
Continue reading below
Prevention of pressure ulcers6
Back to contentsThe majority of pressure ulcers can be prevented.
Skin injury due to friction and shear forces should be minimised through correct positioning, transferring and repositioning techniques.
Pressure redistributing equipment should be used.
Eliminate any source of excess moisture due to incontinence, perspiration or wound drainage.
Reduce underlying risk factors such as poor nutrition.
Education and training - eg, mobility, positioning, skin care, use of equipment - for patients and their carers.
Consider the use of emollients if the skin is dry or barrier products if the skin is excessively moist.
People at high risk of developing pressure ulcers should use higher-specification foam mattresses rather than standard hospital foam mattresses.15
Medical grade sheepskins are associated with a decrease in pressure ulcer development.
A polyurethane foam dressing can be applied to bony prominences (eg, heels, sacrum) for the prevention of pressure ulcers in anatomical areas frequently subjected to friction and shear.6
A barrier preparation can be used to prevent skin damage in adults who are at high risk of developing a moisture lesion or incontinence-associated dermatitis, as identified by skin assessment.4
NB: Whilst widely-used, there is a paucity of high-quality evidence to show that wound-care teams make a difference to the incidence or healing of pressure ulcers.7
Further reading and references
- Pressure ulcers: revised definition and measurement - summary and recommendations; NHS Improvement, 2018.
- Braden Risk Assessment Tool; Healthcare Improvement Scotland
- Moore ZE, Patton D; Risk assessment tools for the prevention of pressure ulcers. Cochrane Database Syst Rev. 2019 Jan 31;1(1):CD006471. doi: 10.1002/14651858.CD006471.pub4.
- Pressure ulcers: prevention and management of pressure ulcers; NICE Clinical Guideline (April 2014 - last verified by NICE 2018)
- Pressure ulcers; NICE Quality Standard, June 2015
- Prevention and Treatment of Pressure Ulcers/Injuries: Quick Reference Guide; National Pressure Ulcer Advisory Panel, 2019
- Moore ZE, Webster J, Samuriwo R; Wound-care teams for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2015 Sep 16;9:CD011011.
- Thomas DR; Role of Nutrition in the Treatment and Prevention of Pressure Ulcers. Nutr Clin Pract. 2014 Jun 24;29(4):466-472.
- Langer G, Fink A; Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2014 Jun 12;6:CD003216. doi: 10.1002/14651858.CD003216.pub2.
- Aziz Z, Bell-Syer SE; Electromagnetic therapy for treating pressure ulcers. Cochrane Database Syst Rev. 2015 Sep 3;9:CD002930.
- Gillespie BM, Chaboyer WP, McInnes E, et al; Repositioning for pressure ulcer prevention in adults. Cochrane Database Syst Rev. 2014 Apr 3;4:CD009958. doi: 10.1002/14651858.CD009958.pub2.
- Dumville JC, Stubbs N, Keogh SJ, et al; Hydrogel dressings for treating pressure ulcers. Cochrane Database Syst Rev. 2015 Feb 17;2:CD011226. doi: 10.1002/14651858.CD011226.pub2.
- Meads C, Lovato E, Longworth L; The Debrisoft Monofilament Debridement Pad for Use in Acute or Chronic Wounds: A NICE Medical Technology Guidance. Appl Health Econ Health Policy. 2015 Aug 28.
- The Debrisoft monofilament debridement pad for use in acute or chronic wounds; NICE Medical technologies guidance, March 2014 - last updated March 2019
- McInnes E, Jammali-Blasi A, Bell-Syer SE, et al; Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev. 2015 Sep 3;9:CD001735.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 12 May 2028
22 May 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free