Retinal artery occlusions
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 28 Apr 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
See also the separate Retinal Vein Occlusions article.
Continue reading below
What is retinal artery occlusion?1 2
Central retinal artery occlusion (CRAO) is an ophthalmic emergency. It is one of the more common causes of severe visual impairment in elderly patients. In order to understand its presentation and effects it is essential to understand the blood supply to the retina:
There are two sources of blood supply to the retina:
The central retinal artery (CRA) is a branch of the ophthalmic artery, which is the first branch of the internal carotid artery. The CRA supplies blood to the surface of the optic disc. From here it divides into two main branches (superior and inferior); these then further divide into temporal and nasal branches, which supply blood to the four quadrants of the retina.
The outer retina is supplied by the choriocapillaries of the choroid that branches off the ciliary artery.
Both the CRA and the ciliary artery must be functioning to maintain retinal function, as both CRA and ciliary artery originate from the OA.
One important variation is the presence of a cilioretinal artery. This artery, thought to be present in 15-30% of people, supplies the macular retina to a varying degree and may help preserve some vision after CRAO. The cilioretinal artery is seen ophthalmoscopically as a single vessel emerging from the edge of the optic disc, most commonly towards the macula.
Depending on where the occlusion occurs, different layers and quarters of the retina can be affected: more proximal ophthalmic artery occlusion will have the most devastating effect, as all layers of the entire retina lose their blood supply, whereas a occlusion of a distal end branch of the retinal artery will only affect the inner neural retina of that part of the retina, sparing the photoreceptors and limiting visual loss.
Occlusion affecting the retinal artery prior to branching is termed CRAO. Occlusion of one of the branches of the retinal artery is referred to as branch retinal artery occlusion (BRAO).
Pathophysiology of retinal artery occlusions1
Back to contentsCRAO is the ocular equivalent of cerebral stroke and is a process of end-organ ischaemia. Many of the risk factors are those for cardiovascular and cerebrovascular disease and its occurrence is a warning sign for other vascular complications.
Individual aetiology remains unclear in many cases. The most common causes are listed below. Potential mechanisms are embolism, vaso-obliteration and vascular compression. Embolism is the most common cause, the major source of this being carotid artery disease, usually due to atherosclerotic plaques. Carotid stenosis and the heart are other important sources of emboli. Around 75% of these emboli are made of cholesterol, 10% of calcific material and 15% of fibrin.
Local atherosclerotic plaques and vasculitis may cause vaso-obliteration. Emboli (calcified, thrombotic, myxomatous, bacterial, or cholesterol) are usually of carotid or cardiac origin. A retrobulbar mass may lead to optic nerve and CRA compression:
Atherosclerosis: atheroma-related thrombus accounts for about 80% of CRAOs, with increased risk for people with hypertension or diabetes.3
Embolism:
Carotid: this may be a cholesterol, fibrinoplatelet, or calcific embolus.
Cardiac: this may be calcific, vegetations from the cardiac valves (endocarditis), or a mural thrombus (eg, in atrial fibrillation).
Aortic disease (including dissection) may be another embolic source.
Inflammatory - such as temporal arteritis (giant cell arteritis), polyarteritis nodosa, systemic lupus erythematosus (SLE), granulomatosis with polyangiitis, Takayasu's arteritis, pancreatitis.
Thrombophilic disorders - such as antiphospholipid antibody syndrome, protein S deficiency, protein C deficiency, leukaemias, or lymphomas.
Infectious origin - toxoplasmosis, mucormycosis, syphilis.
Pharmacological causes - oral contraceptive pill, cocaine.
Ophthalmic causes - severely raised intraocular pressure trauma or optic nerve drusen.
Rarely, retinal migraine (vasospasm) - this can be seen in younger individuals where all other causes have been excluded.4
Retinal damage becomes increasingly irreversible over time. The optimal treatment window during which treatment may be beneficial is controversial but believed to be about 90-100 minutes (some say up to 105 minutes)5 , although some form of treatment will usually be attempted within 24-48 hours of onset.
Continue reading below
Central retinal artery occlusion
Back to contentsWhat is central retinal artery occlusion?1
In CRAO the CRA occludes before it branches, as it emerges from the optic nerve. This leads to a unilateral acute painless loss of vision.
Incidence
It has an estimated incidence of around 1 in 100,000/year.1
The majority of patients are aged >60 years. Younger patients usually have valvular heart disease.
Men are slightly more affected than women.
Central retinal artery occlusion symptoms1
Sudden (over a few seconds), unilateral painless visual loss.
In 94% of cases, vision is usually reduced to counting fingers (worse suggests that the ophthalmic artery may also be affected).
There may be a history of amaurosis fugax (amaurosis fugax precedes loss of vision in up to 10% of patients).
In 1-2% of patients, the loss is bilateral (although the degree is not necessarily the same in each eye).
Cherry red spot and retinal swelling of central retinal artery occlusion
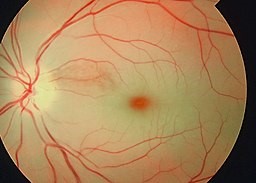
© sidthedoc, CC BY-SA 4.0, via Wikimedia Commons
By sidthedoc, CC BY-SA 4.0, via Wikimedia Commons
Examination reveals an afferent pupillary defect and a pale retina with attenuation of the vessels. There may be segmentation of the blood column in the arteries ('cattle-trucking') and the centre of the macula (supplied by the intact underlying choroid) stands out as a cherry-red spot.
Systemic examination should include carotid auscultation for bruits, heart sounds for murmurs, radial pulse for atrial fibrillation and blood pressure.
Risk factors1
Differential diagnosis
Investigations1
Diagnosis is usually clinical and investigations are aimed at ruling out underlying diseases. The most important cause to rule out is giant cell arteritis because, with timely intervention, the visual loss is reversible and the fellow eye will be protected. If there is any doubt about the diagnosis then fluorescein angiography and optical coherence tomography may be helpful.
Urgent ESR and CRP are measured in patients over 60 years of age, when a diagnosis of giant cell arteritis cannot be excluded. Coagulation studies, full blood examination and screening tests for vasculitis are usually performed. In the longer term, cardiovascular risk assessment includes measurement of fasting blood sugar and lipid profile.
Central retinal artery occlusion treatment and management5 6 7
Retinal artery occlusion is an ocular emergency, both because the retinal damage rapidly becomes irreversible with time and because of the urgent need to optimise management of other risk factors in order to protect both the other eye and the cerebrovascular and cardiovascular systems. However, whilst several management options have been, and still are, employed, there is currently no evidence-based treatment to reverse the visual loss.
If giant cell arteritis is suspected, it needs immediate treatment (intravenous steroids followed by oral steroids), as it is in itself an ophthalmological emergency.
Management of the eye8
The principle of management is to attempt to reperfuse ischaemic tissue as quickly as possible and to institute secondary prevention early.
'Standard' therapies are unfortunately of no proven benefit. Many have had anecdotal support and, in the absence of anything more certain, they are often tried. They include:
If the patient presents within 90-100 minutes of onset of symptoms, firm ocular massage (repeatedly massaging the globe over the closed lid for ten seconds with five-second interludes) may dislodge the obstruction. However, this only works very occasionally.
Lowering intraocular pressure with anterior chamber paracentesis (withdrawal of a little fluid from the anterior chamber under local anaesthetic, done in the clinic), together with treatment with acetazolamide. Other intraocular pressure-lowering drugs include apraclonidine, mannitol and beta-blockers.
Dilatation of the artery (eg, sublingual isosorbide dinitrate, inhaled carbogen or hyperbaric oxygen).
Oral pentoxifylline, for example. In trials this showed improved retinal perfusion but no clinical improvement in vision.
Intra-arterial fibrinolysis through local injection of urokinase into the proximal part of the ophthalmic artery.
Enhanced external counterpulsation (EECP) offers some promise for the future. This non-invasive technique has been reported as helping to relieve refractory angina and improve exercise tolerance. Pneumatic cuffs on the lower extremities are inflated sequentially at the onset of diastole, causing aortic counter pulsation and increased venous return. Some trials have suggested that it results in increased retinal perfusion after CRAO and BRAO, although again it is as yet unclear whether this translates into improved functional vision.9
There has been considerable interest in thrombolysis using tissue plasminogen activator (tPA), delivered either intravenously or intra-arterially (by direct catheterisation of the ophthalmic artery). A number of observational series had suggested effectiveness in restoring retinal perfusion. However, formal trials suggest that intra-arterial delivery of thrombolytic may result in an increased risk of intracranial and systemic haemorrhage, and intravenous tPA has not been shown to be effective within 24 hours of symptom onset.6 7 10
Long-term management5 8
Retinal artery occlusion is a marker for increased risk of ischaemic end-organ damage such as cerebral stroke and vascular dementia.11 12 13
Long-term management of any retinal artery occlusion therefore aims to:
Identify and address underlying causes in order to prevent further ischaemic events (eg, investigate and treat hypertension).14
Assess for coagulopathies - assessment should also be performed, particularly if no embolic source is found.
Reduce risk factors for atherosclerosis: optimised management of hypertension and prophylaxis with statins and low-dose aspirin may be beneficial.
Long-term management of the condition may also involve the following:
Carotid endartectomy - may be necessary depending on the degree of carotid occlusion and local policy.
Ophthalmic follow-up in the eye department - will be necessary to assess for complications, the main one being iris neovascularisation, which can cause glaucoma or vitreous haemorrhage. In arterial occlusions, neovascular sequelae are uncommon, unlike venous occlusions, perhaps due to the complete ischaemia in the affected retinal segment.
Referral to low vision aid clinics - consideration should be given to this, particularly if acuity in the other eye is also affected.
Driver and Vehicle Licensing Agency (DVLA) notification - if there is complete loss of vision in one eye (lacking even light perception), the DVLA may need to be notified. Patients may still be able to drive after clinical advice of successful adaptation to the condition.
Outcome2
Even with early treatment, the prognosis is generally very poor, as the inner neural layer swiftly becomes atrophic and all useful vision is generally lost. Only about a third of patients show any improvement.
Spontaneous resolution of the blockage has been reported in 1-8% (some have reported up to 15%) of patients.
Patients with retinal emboli have a 3 x increased mortality rate compared to those without. They should be managed in the same way as patients with a personal history of coronary heart disease.
Branch retinal artery occlusion2
Back to contentsWhat is branch retinal artery occlusion?
In branch retinal artery occlusion (BRAO) one or multiple branches of the CRA may be affected.
Branch retinal artery occlusion symptoms
This is as for CRAO but only part of the vision is lost: the defect is usually the upper/lower half of vision or sectoral. Retinal pallor corresponds to the area supplied by the affected artery. Occasionally, an embolus (cholesterol, fibrinoplatelet, calcific) can be seen within the artery, and cotton wool spots may eventually occur around that area.
Branch retinal artery occlusion treatment and management
Refer within 24 hours. However, there is no proven effective management.
Long-term management is as for CRAO.
Full and thorough assessment of the cardiovascular system as for CRAO. Carotid endarterectomy or anticoagulation may be indicated.
Thorough assessment for coagulopathies should also be performed if no embolic source is found.
Outcome
Occasionally, recanalisation of the artery occurs but this is rare. However, around 30% of eyes have collateral cilioretinal arteries serving the macular retina so that central vision can be retained to some extent.
Visual acuity of 20/40 OR BETTER is seen initially in 74% of cases of permanent BRAO, AND 94% of transient BRAO, and on follow-up, in 89% and 100% of cases, respectively.
Continue reading below
Cilioretinal artery occlusion2
Back to contentsThe cilioretinal artery is present in 15-30% of the population. An isolated occlusion of this artery will cause variable central visual loss. Cilioretinal artery occlusion results from the same factors as CRAO; therefore, the same long-term approach to the management of underlying and contributing conditions is needed. Central vision is affected but, depending on the level of reliance of the macular retina on the cilioretinal artery, the degree can be variable - from moderate blurring of vision to loss of central vision.
Fundal appearance is of an attenuated cilioretinal artery with localised area of superficial retinal whitening, often between the optic nerve head and macula. There may be an associated central retinal vein occlusion, or anterior ischaemic optic neuropathy (which is more often seen in elderly patients and may be associated with giant cell arteritis).
Visual prognosis is usually good if the macula has been spared; however, a visual field defect may remain. Around 75% of patients with isolated cilioretinal artery occlusion regain visual acuity of 20/40 (6/12) or better; the prognosis is only slightly worse if combined with a central retinal vein occlusion. However, if the condition is combined with anterior ischaemic optic neuropathy the visual prognosis is poor.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Hayreh SS, Podhajsky PA, Zimmerman MB; Retinal Artery Occlusion Associated Systemic and Ophthalmic Abnormalities. Ophthalmology. 2009 Jul 2.
- Mac Grory B, Schrag M, Biousse V, et al; Management of Central Retinal Artery Occlusion: A Scientific Statement From the American Heart Association. Stroke. 2021 Jun;52(6):e282-e294. doi: 10.1161/STR.0000000000000366. Epub 2021 Mar 8.
- Hayreh SS; Is Management of Central Retinal Artery Occlusion the Next Frontier in Cerebrovascular Diseases? J Stroke Cerebrovasc Dis. 2019 Feb;28(2):256-258. doi: 10.1016/j.jstrokecerebrovasdis.2018.09.044. Epub 2018 Oct 26.
- Varma DD, Cugati S, Lee AW, et al; A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013 Jun;27(6):688-97. doi: 10.1038/eye.2013.25. Epub 2013 Mar 8.
- Hayreh SS, Podhajsky PA, Zimmerman MB; Branch retinal artery occlusion: natural history of visual outcome. Ophthalmology. 2009 Jun;116(6):1188-94.e1-4. doi: 10.1016/j.ophtha.2009.01.015. Epub 2009 Apr 18.
- Chang YS, Ho CH, Chu CC, et al; Risk of retinal artery occlusion in patients with diabetes mellitus: A retrospective large-scale cohort study. PLoS One. 2018 Aug 9;13(8):e0201627. doi: 10.1371/journal.pone.0201627. eCollection 2018.
- Grosberg BM, Solomon S, Friedman DI, et al; Retinal migraine reappraised. Cephalalgia. 2006 Nov;26(11):1275-86.
- Fraser SG, Adams W; Interventions for acute non-arteritic central retinal artery occlusion. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD001989. doi: 10.1002/14651858.CD001989.pub2.
- Feltgen N, Neubauer A, Jurklies B, et al; Multicenter study of the European Assessment Group for Lysis in the Eye (EAGLE) for the treatment of central retinal artery occlusion: design issues and implications. EAGLE Study report no. 1 : EAGLE Study report no. 1. Graefes Arch Clin Exp Ophthalmol. 2006 Aug;244(8):950-6. Epub 2005 Dec 22.
- Chen CS, Lee AW, Campbell B, et al; Efficacy of intravenous tissue-type plasminogen activator in central retinal artery occlusion: report from a randomized, controlled trial. Stroke. 2011 Aug;42(8):2229-34. doi: 10.1161/STROKEAHA.111.613653. Epub 2011 Jul 14.
- Cugati S, Varma DD, Chen CS, et al; Treatment options for central retinal artery occlusion. Curr Treat Options Neurol. 2013 Feb;15(1):63-77. doi: 10.1007/s11940-012-0202-9.
- Yang Y, Zhang H, Yan Y, et al; Clinical study in patients with ocular ischemic diseases treated with enhanced external counterpulsation combined with drugs. Mol Med Rep. 2013 Jun;7(6):1845-9. doi: 10.3892/mmr.2013.1445. Epub 2013 Apr 26.
- Zhang X, Ji X, Luo Y, et al; Intra-arterial thrombolysis for acute central retinal artery occlusion. Neurol Res. 2009 May;31(4):385-9.
- Singh Hayreh S; Risk of acute stroke in patients with retinal artery occlusion. Eye (Lond). 2020 Jun;34(6):1149. doi: 10.1038/s41433-019-0715-5. Epub 2019 Nov 25.
- Lee CS, Lee ML, Gibbons LE, et al; Associations Between Retinal Artery/Vein Occlusions and Risk of Vascular Dementia. J Alzheimers Dis. 2021;81(1):245-253. doi: 10.3233/JAD-201492.
- Zhou Y, Zhu W, Wang C; Relationship between retinal vascular occlusions and incident cerebrovascular diseases: A systematic review and meta-analysis. Medicine (Baltimore). 2016 Jun;95(26):e4075. doi: 10.1097/MD.0000000000004075.
- Colucciello M; Retinal vascular disease in hypertension. Risk factor modification optimizes vision outcomes. Postgrad Med. 2005 Jun;117(6):33-8, 41-2.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 28 Mar 2027
28 Apr 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free