Varicose veins
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 20 Nov 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Varicose veins article more useful, or one of our other health articles.
In this article:
Continue reading below
What are varicose veins?
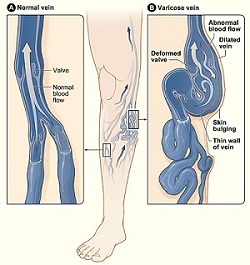
The term varicose derives from the Latin 'varix', which means twisted. A varicose vein is usually tortuous and dilated.
Under normal circumstances, blood collected from superficial venous capillaries is directed upwards and inwards via one-way valves into superficial veins. These in turn drain via perforator veins, which pass through muscle fascia into deeper veins buried under the fascia. Leakage in a valve causes retrograde flow back into the vein.
Unlike deep veins which are thick-walled and confined by fascia, superficial veins cannot withstand high pressure and eventually become dilated and tortuous. The failure of one valve puts pressure on its neighbours and may result in retrograde flow - and hence varicosity - of the entire local superficial venous network.12
The superficial veins in the legs are normally involved, as these are most likely to come under hydrostatic pressure due to gravity.
Other pathological processes may also be involved, such as an inherent weakness of the vein wall. The influence of genetics has been confirmed by twin studies and genetic studies.3
Pregnancy brings its own problems, with hormonal factors increasing the pliability of the venous walls and the valves themselves. In later pregnancy, there is expansion of the circulating blood volume and this is compounded by pressure on the inferior vena cava from the growing uterus. Pelvic vein reflux is known to contribute to the development of primary and recurrent varicose veins in pregnancy.4
Another mechanism that sometimes comes into play is obstruction to venous outflow. This can be either intravascular, as in deep vein thrombosis (DVT), or extravascular from trauma or compression from surrounding structures such as tumours or a cirrhotic liver.
Varicose veins
By Jmarchn, modified from Varicose veins.jpg of National Heart Lung and Blood Institute (NIH), CC BY-SA 3.0, via Wikimedia Commons
Varicose veins on leg

© Self, Public domain, via Wikimedia Commons
By self, Public domain, via Wikimedia Commons
How common are varicose veins? (Epidemiology)5
Back to contentsVaricose veins are thought to affect at least a third of the population.
The prevalence of varicose veins increases with age, and they often develop during pregnancy.
Prevalence rates are higher in industrialised countries and in more developed regions.
Continue reading below
Risk factors for varicose veins6
Back to contentsPregnancy.
Obesity.
Older age (>65 years).
Symptoms of varicose veins (presentation)5
Back to contentsHistory
It is important to establish at the initial consultation why the patient has presented. Patients with cosmetic concerns present less often than they used to, but are still occasionally seen with asymptomatic but unsightly tortuous veins or thread veins.
Commonly, patients will present with chronic sequelae such as itching, discomfort and heaviness of the legs, night cramps, oedema, burning sensations, paraesthesiae, exercise intolerance, or restless legs. Subjective symptoms are usually more severe in the early stages of the condition, less severe in middle stages and worse in latter years.
The pain associated with larger varicose veins is usually described as a dull ache that is worse after prolonged standing. Aggravating factors may include pregnancy, exogenous hormones, menstruation and, occasionally, sexual intercourse.
Apart from the presenting symptoms, the history should include:
History of previous venous problems, any visible abnormal veins and any history of varicosities in pregnancy.
Any risk factors such as family history of varicose veins, a job which involves prolonged standing, past history of trauma.
History of oedema, date of onset, any risk factors, any variation throughout the day, degree of induration and location.
History of any previous hospital assessments or treatment.
History of any previous episodes of superficial or deep vein thrombosis or thrombophlebitis.
History of bleeding from varicose veins.
History of any cardiovascular comorbidity.
Examination7
A complete examination should include a general assessment of the patient's cardiovascular status and abdominal examination to exclude secondary causes, such as tumours which could be causing external venous compression.
To map the areas of varicosity, examine the patient with them standing in the first instance. To confirm that a swelling is a varicose vein, gently press over the area. The vein will empty and then refill.
Attempt to identify which vein the varicosities drain into. Varicosities of the short saphenous vein are normally seen below the knee and are distributed posterolaterally. Long saphenous vein varicosities may run the whole length of the leg and are distributed more medially.
Inspect the skin for changes suggestive of chronic venous insufficiency. These may include ulcers, lipodermatitis, pigmentation, telangiectasia or eczema.
Once you have finished the inspection, ask the patient to lie down, and identify the saphenofemoral junction. One good way to do this is by locating the femoral artery, which lies between the anterior superior iliac spine and the symphysis pubis, by feeling for the pulse. The vein is medial to the artery and the saphenofemoral junction about two fingers' breadth below the inguinal ligament.
Ask the patient to stand and tap the varicosity lower down the leg. A fluid thrill felt at the level of the valve indicates that it is incompetent.
Two tests have classically been used to assess valvular competency (Trendelenburg's test) and deep venous patency (Perthes' test). They have been superseded to a large extent by other non-invasive investigations (see 'Investigations', below) but may still be relevant in a primary care setting. The Royal College of Surgeons in England expects its membership candidates to abandon Trendelenburg's, Perthes' and tap testing in favour of hand-held Doppler assessment but that they should understand the principles behind the techniques.8
Trendelenburg's test
This can sometimes distinguish patients with superficial venous reflux from those with incompetent deep venous valves. The patient should lie flat with the leg elevated, allowing the veins to empty. A tourniquet is applied to the thigh at the saphenous opening. If the valve is competent, the vein should fill from below. If the valve is incompetent, the vein will fill from above on removal of the tourniquet. This can be repeated at various levels, until the location of an incompetent valve is located.
Perthes' manoeuvre
This manoeuvre is used to distinguish antegrade flow from retrograde flow in superficial varicosities. Antegrade flow is an indicator of collateral flow around a deep venous obstruction. A tourniquet is applied to a varicose leg in such a way that the superficial veins are compressed without pressure being applied to the deep vessels. The patient is then asked to stand repeatedly on tiptoe, activating the calf muscles. Normally this would empty the varicosities but, in the presence of deep vein obstruction, they would paradoxically become congested.
Continue reading below
Differential diagnosis
Back to contentsDiagnosing varicose veins (investigations)
Back to contentsImaging
Duplex ultrasound is the preferred modality. It uses a combination of Doppler and conventional ultrasound. It gives more detailed information than a hand-held Doppler and is better at confirming the diagnosis and the pattern of venous disease. This helps to determine the most appropriate treatment option.5
Colour-duplex ultrasound is a newer technique which provides more sensitive information about varicose vein morphology.9
Physiological tests of venous function10
These may be helpful as an adjunct to imaging in complex cases and when researching the effectiveness of treatments:11
Venous refilling time - the time necessary for the lower leg to fill with blood after it has been maximally emptied by the calf-muscle pump.
Maximum venous outflow - the time taken for a leg distended by a tourniquet to empty. It is a measure of possible venous obstruction.
Muscle pump ejection fraction - used to detect failure of the muscle pump to expel blood from the lower leg.
Associated diseases
Back to contentsDVT; any condition causing calf-muscle pump failure (eg, neuromuscular disease, muscle wasting conditions).5
Arterial disease - a review of the literature found some evidence to suggest a link between peripheral arterial disease and varicose veins. The evidence for an association with hypertension was weaker.12
Thrombophilia - one study found that patients with this condition had a higher incidence of varicose veins than those who did not.13
Staging of varicose veins14
Back to contentsVarious classification systems have been used, the original being the CEAP (Clinical picture, Etiology, Anatomical distribution and Pathophysiology) classification, devised by the Consensus Committee of the American Venous Forum. This included such features as the number and extent of varicosities, the presence of skin changes and the disabling effect of any symptoms. The original system was published in 1994 and has been updated over time. The most recent revision was in 2020.15
Management of varicose veins5
Back to contentsPrimary care
It is important to determine why the patient is presenting for treatment. One third of patients have symptoms unrelated to varicose veins, or may simply be seeking advice about possible complications or deterioration.
Lifestyle changes
The evidence base addressing the issue of lifestyle changes such as weight loss and exercise is limited but they are most likely to be of benefit in preventing the initial development of varicosities and their complications, rather than reversing the disease process once it is established (see 'Prevention', below). Patients should be advised to avoid prolonged standing and to keep the leg(s) elevated when possible.
Compression stockings5
The National Institute for Health and Care Excellence (NICE) does not recommend treatment with compression stockings unless interventional treatment is not appropriate. If compression stockings are to be used, it is important to exclude arterial disease before prescribing them, by measuring the ankle-brachial pressure index (ABPI) using a Doppler.
Class 1 (light) or class 2 (medium) below-knee stockings are usually sufficient, the choice depending on the severity of the varicosities and the tolerability of the compression. Thigh-length stockings may be beneficial if the varicosities extend above the knee. Open-toed stockings may be appropriate for people who have problems with their feet, such as arthritis or fungal infection of the toes.
They should be taken off at night and replaced every three to six months. Patients should be made aware that stockings may not prevent new varicosities from developing or existing ones from getting worse. The evidence base supporting their use during pregnancy is weaker but some women may find them helpful in controlling symptoms.
If compression stockings are offered after interventional treatments, they should not be worn for longer than seven days.
When to refer
Refer according to local policies, if available; always consider the patient's general health and comorbidities when assessing appropriateness of referral.
Emergency referral where there is active bleeding from a varicose vein that has eroded the skin.
Urgent referral if there is a history of active bleeding and still a risk of further bleeding. Patients with progressive leg ulcers or painful ulcers despite treatment should also be fast-tracked.
Consider (routine) referral for:
Primary or recurrent varicose veins which cause symptoms (eg, pain, aching, discomfort, swelling, heaviness, or itching).
Skin changes of the legs such as pigmentation or eczema, thought to be caused by chronic venous insufficiency.
Hard, painful veins indicative of superficial venous thrombosis.
Suspected venous incompetence.
A venous leg ulcer (a break in the skin below the knee that has not healed within two weeks) - refer within two weeks.
A healed venous leg ulcer.
Consider the need for referral in pregnant women, as interventional treatments are unlikely to be a realistic proposition.
Treatment options in secondary care16
Although conventional surgery is still performed, NICE recommends that, for confirmed varicose veins with truncal reflux, minimally invasive procedures such as radiofrequency ablation, endovenous laser therapy or foam sclerotherapy should be considered first.
Endothermal ablation
Endothermal (radiofrequency) ablation involves sealing the lumen of the long saphenous vein by delivering radiofrequency energy via a catheter under ultrasound guidance. An alternative is endovenous laser therapy which works by delivering high-intensity laser through a sheathed wire guided into the vein.
Ultrasound-guided foam sclerotherapy
This is recommended if endothermal ablation is unsuitable. It involves imaging-guided injection of sclerosant in foam form. Sodium tetradecyl sulfate is a typical sclerosant and the gas used is usually carbon dioxide or air. It is recommended that incompetent varicose tributaries be treated at the same time.
If foam sclerotherapy is unsuitable, consider conventional surgery.
Avulsion
This is a very old technique in which small incisions are made over each varicosity and that part of the vein is excised using a vein hook or forceps.17
Stripping
A wire, plastic or metal rod is passed through the lumen of the saphenous vein and pulled until the entire vein is stripped out of the leg. Inversion stripping is a refinement of this method, in which the vein is turned in on itself during removal.
Partial stripping to the knee may cause less neurological trauma than stripping to the ankle. It preserves venous tissue that may subsequently be required for vein grafting techniques (eg, coronary artery bypass graft). It is the current preferred invasive method.
Ambulatory phlebectomy
This can be performed, using local anaesthetic, as an outpatient procedure. Small multiple incisions are made in the skin overlying the vein, which is hooked out and extracted in a piece-meal fashion.
The technique is particularly suitable for tortuous veins inaccessible to fine-wire techniques such as laser ablation. Contra-indications are reflux at the saphenofemoral or saphenopopliteal junctions, which must be treated by other means.18
Injection sclerotherapy
Once used as first-line treatment for new varicosities, this is now being employed less frequently due to concerns about skin staining and ulceration. It is only indicated for below-knee varices and is mainly used for persistent or recurrent veins after surgery. It has largely been replaced by foam sclerotherapy.
A Cochrane review concluded that the evidence supported the current place of this treatment, which is usually reserved for recurrent veins after surgery and for thread veins.19
Complications of varicose veins20
Back to contentsComplications directly relating to varicose veins include haemorrhage and thrombophlebitis.
Complications relating to the increased pressure arising from chronic venous incompetence (venous hypertension) include venous ulcers, oedema, skin pigmentation, varicose eczema, atrophie blanche (smooth white areas of atrophic scar tissue with telangiectasia) and lipodermatosclerosis (areas of induration arising from fibrosis of subcutaneous fat).
Potential complications of treatment include DVT and pulmonary embolus, paraesthesiae from injury to the sural nerve or the saphenous nerve and the development of haematomas. Skin burns have been known to occur if radiofrequency catheters are placed too near the skin.21
Prognosis20
Back to contentsUntreated, varicose veins tend to become larger over time and patients with significant reflux are prone to develop chronic venous ulceration. Long-term studies of the outcome of surgical treatment have been less than encouraging. 13.5% of varicose vein surgery is for recurrence. Studies suggest a 90-98% occlusion with radiofrequency ablation after two years.22 The closure rate for endovenous laser treatment after two years was 93.4%.23 For foam sclerotherapy, the clinical recurrence rate with significant symptoms was 4% at five years.24
Prevention of varicose veins
Back to contentsCertain factors such as genetic predisposition, gender and increasing age are unavoidable. There is evidence that weight control acts as a primary preventative measure but only for women.
There is insufficient evidence to support the effectiveness of self-help advice regarding potentially avoidable factors such as prolonged sitting or standing, tight undergarments, low-fibre diet, constipation, and smoking.25
Further reading and references
- Raetz J, Wilson M, Collins K; Varicose Veins: Diagnosis and Treatment. Am Fam Physician. 2019 Jun 1;99(11):682-688.
- de Avila Oliveira R, Riera R, Vasconcelos V, et al; Injection sclerotherapy for varicose veins. Cochrane Database Syst Rev. 2021 Dec 10;12(12):CD001732. doi: 10.1002/14651858.CD001732.pub3.
- Cotton SC, MacLennan G, Brittenden J, et al; Behavioural recovery after treatment for varicose veins. Br J Surg. 2016 Mar;103(4):374-81. doi: 10.1002/bjs.10081. Epub 2016 Jan 25.
- Meissner MH; Lower extremity venous anatomy. Semin Intervent Radiol. 2005 Sep;22(3):147-56. doi: 10.1055/s-2005-921948.
- Surendran S, S Ramegowda K, Suresh A, et al; Arterialization and anomalous vein wall remodeling in varicose veins is associated with upregulated FoxC2-Dll4 pathway. Lab Invest. 2016 Apr;96(4):399-408. doi: 10.1038/labinvest.2015.167. Epub 2016 Jan 25.
- Krysa J, Jones GT, van Rij AM; Evidence for a genetic role in varicose veins and chronic venous insufficiency. Phlebology. 2012 Oct;27(7):329-35. doi: 10.1258/phleb.2011.011030. Epub 2012 Feb 3.
- Dos Santos SJ, Holdstock JM, Harrison CC, et al; The effect of a subsequent pregnancy after transjugular coil embolisation for pelvic vein reflux. Phlebology. 2016 Jan 14. pii: 0268355515623898.
- Varicose veins; NICE CKS, February 2024 (UK access only)
- Heit JA, Spencer FA, White RH; The epidemiology of venous thromboembolism. J Thromb Thrombolysis. 2016 Jan;41(1):3-14. doi: 10.1007/s11239-015-1311-6.
- Varicose Veins Exam; Clinicalexam.com
- Kanani M et al; MRCS Revision Guide: Limbs and Spine, 2011.
- Cavezzi A; Medicine and Phlebolymphology: Time to Change? J Clin Med. 2020 Dec 18;9(12). pii: jcm9124091. doi: 10.3390/jcm9124091.
- Ibegbuna V, Delis KT, Nicolaides AN; Haemodynamic and clinical impact of superficial, deep and perforator vein incompetence. Eur J Vasc Endovasc Surg. 2006 May;31(5):535-41. Epub 2006 Jan 4.
- Volpe EFT, Resqueti VR, da Silva AAM, et al; Supervised exercise protocol for lower limbs in subjects with chronic venous disease: an evaluator-blinded, randomized clinical trial. Trials. 2020 May 19;21(1):414. doi: 10.1186/s13063-020-04314-1.
- Matic M, Matic A, Djuran V, et al; Frequency of Peripheral Arterial Disease in Patients With Chronic Venous Insufficiency. Iran Red Crescent Med J. 2016 Jan 2;18(1):e20781. doi: 10.5812/ircmj.20781. eCollection 2016 Jan.
- Darvall KA, Sam RC, Adam DJ, et al; Higher prevalence of thrombophilia in patients with varicose veins and venous ulcers than controls. J Vasc Surg. 2009 May;49(5):1235-41.
- Rabe E, Pannier F; Clinical, aetiological, anatomical and pathological classification (CEAP): gold standard and limits. Phlebology. 2012 Mar;27 Suppl 1:114-8. doi: 10.1258/phleb.2012.012S19.
- Lurie F, Passman M, Meisner M, et al; The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord. 2020 May;8(3):342-352. doi: 10.1016/j.jvsv.2019.12.075. Epub 2020 Feb 27.
- Varicose veins: diagnosis and management; NICE Clinical Guideline (July 2013)
- O'Sullivan HD; The Treatment of Varicose Veins of the Lower Limb by Avulsion. Br Med J. 1910 Apr 16;1(2572):921.
- Kabnick LS, Ombrellino M; Ambulatory phlebectomy. Semin Intervent Radiol. 2005 Sep;22(3):218-24. doi: 10.1055/s-2005-921955.
- Tisi PV, Beverley C, Rees A; Injection sclerotherapy for varicose veins. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD001732.
- Joseph N, B A, Faizan Thouseef M, et al; A multicenter review of epidemiology and management of varicose veins for national guidance. Ann Med Surg (Lond). 2016 Apr 30;8:21-7. doi: 10.1016/j.amsu.2016.04.024. eCollection 2016 Jun.
- Subramonia S, Lees TA; The treatment of varicose veins. Ann R Coll Surg Engl. 2007 Mar;89(2):96-100.
- Radiofrequency ablation of varicose veins; NICE Interventional Procedure Guidance, September 2013
- Endovenous laser treatment of the long saphenous vein; NICE Interventional Procedure Guidance, March 2004
- Ultrasound-guided foam sclerotherapy for varicose veins; NICE Interventional procedure guidance, February 2013
- Tisi PV; Varicose veins. BMJ Clin Evid. 2011 Jan 5;2011. pii: 0212.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 19 Nov 2027
20 Nov 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free