Hyponatraemia
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Laurence KnottLast updated 10 Feb 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Hyponatraemia article more useful, or one of our other health articles.
In this article:
What is hyponatraemia?
Serum sodium concentration is maintained by a homeostatic mechanism that involves thirst, antidiuretic hormone (ADH, also called vasopressin) secretion, the renin-angiotensin-aldosterone feedback system and the renal handling of sodium.
Hyponatraemia represents a relative excess of water in relation to sodium and is defined as a serum sodium <136 mmol/L. A level <120 mmol/L is considered severe.
Falsely low sodium value results can occur with very high circulating levels of lipids or proteins in which the concentration of sodium in the water phase is normal (plasma osmolality normal). This can also occur in severe hyperglycaemia as the high levels of glucose draw intracellular water into the extracellular space.
Epidemiology
Back to contentsHyponatraemia is the most common electrolyte abnormality encountered in clinical practice.
An accurate incidence of mild hyponatraemia managed in the community is impossible, as it is rarely reported.
Hyponatraemia is associated with multiple poor clinical outcomes and is often managed suboptimally because of inadequate assessment and investigation1 .
There is no sex predilection.
Infants and the elderly are most at risk because they are less likely to be able to express their thirst and autonomously control their own fluid intake.
Furthermore, infants with diarrhoea, given tap water instead of electrolyte replacement fluid, and those given watered-down milk formula for reasons of economy, are known to be at risk.
Continue reading below
Hyponatraemia symptoms
Back to contentsThis depends upon severity and is dictated not only by the absolute serum sodium level but also by the rate of fall.
Hyponatraemia is often asymptomatic if it is mild to moderate and also chronic (lasting more than 48 hours).
Chronic mild hyponatraemia may be asymptomatic whilst a sudden fall to only 125 mmol/L from normal values can result in convulsions (usually from inappropriate intravenous fluids).
The clinical picture can be confusing, because mild hyponatraemia can cause significant symptoms if the drop in sodium level is sudden, whereas severe chronic hyponatraemia can cause no symptoms, due to cerebral adaption2 .
However, the following symptoms may occur:
Mild - anorexia, headache, nausea, vomiting, lethargy.
Moderate - personality change, muscle cramps and weakness, confusion, ataxia.
Severe - drowsiness.
Signs
These are again highly variable and depend on the level and rate of fall of the serum sodium. They may include:
Neurological signs:
Decreased level of consciousness.
Cognitive impairment (eg, short-term memory loss, disorientation, confusion, depression).
Focal or generalised seizures.
Brainstem herniation - seen in severe acute hyponatraemia; signs include coma; fixed, unilateral, dilated pupil; decorticate or decerebrate posturing; respiratory arrest.
Signs of hypovolaemia - dry mucous membranes, tachycardia, diminished skin turgor.
Signs of hypervolaemia - pulmonary rales, S3 gallop (third heart sound), jugular venous distention, peripheral oedema, ascites.
Aetiology3
Back to contentsThe causes of true hyponatraemia can be divided into three groups based on their effect on extracellular fluid volume. These can further be subdivided by the concentration of sodium in the urine.
Causes of hyponatraemia: flowchart
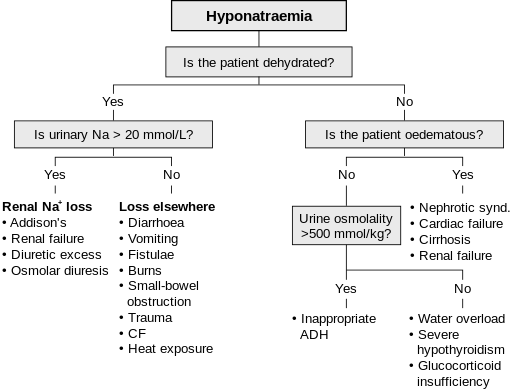
© James Bedford, User: Stannered, Public domain, via Wikimedia Commons
By en User: James Bedford, User: Stannered, Public domain, via Wikimedia Commons
Syndrome of inappropriate ADH secretion (SIADH)
Inappropriate ADH secretion from posterior pituitary or from ectopic source despite low serum osmolality.
Major diagnostic features
Hyponatraemia.
Plasma hypo-osmolality proportional to hyponatraemia.
Inappropriately elevated urine osmolality (>100 mOsmol/kg) commonly > plasma osmolarity.
Persistent urine [Na+] >30 mmol/L with normal salt intake.
Euvolaemia.
Normal thyroid and adrenal function.
Extra features include an elevated ADH level and low blood uric acid level.
Causes (not exhaustive)
Neurological: tumour, trauma, infection, Guillain-Barré syndrome, multiple sclerosis, systemic lupus erythematosus, intracranial haemorrhage, sinus thrombosis, AIDS, porphyria.
Pulmonary: lung small-cell cancer, mesothelioma, pneumonia, cystic fibrosis, asthma, tuberculosis, positive-pressure ventilation.
Other malignancy: oropharyngeal, stomach, pancreas, leukaemia, lymphoma, thymoma, and genitourinary tract cancers.
Drugs: the most common are thiazide diuretics, selective serotonin reuptake inhibitors (SSRIs), proton pump inhibitors, angiotensin-converting enzyme (ACE) inhibitors and loop diuretics.
Miscellaneous: idiopathic, hereditary, pain, postoperative, stress, endurance exercise and marathon runners, herpes zoster.
Continue reading below
Investigations4
Back to contentsClinical examination should be focused on fluid status, including blood pressure (BP), postural deficit, heart rate, peripheral oedema and central venous filling, as well as chest and heart examination.
Clinical assessment should identify potential causes, establish the severity of hyponatraemia and determine if the patient is hypovolaemic, euvolaemic, or hypervolaemic.
Serum sodium. Before embarking on other investigations for hyponatraemia, consider whether the sample suffered from dilution by being taken near the site of an infusion, or whether there is any chance of laboratory error. If necessary, repeat the test.
Serum potassium. If raised, consider Addison's disease.
SIADH needs to be confirmed by results of paired serum and urine samples: serum hypo-osmolality is <275 mOsm/kg, and urine osmolality >100 mOsm/kg and sodium ≥30 mmol/L, in the absence of hypovolaemia, hypervolaemia, adrenal or thyroid dysfunction and use of diuretics.
Urine sodium level. If this is >20 mmol/L, a renal cause should be sought.
Serum thyroid-stimulating hormone and free thyroxine level. These should be checked to exclude hypothyroidism.
Random serum cortisol levels or adrenocorticotropic hormone (ACTH) stimulation test. Either of these should be considered in patients with suspected adrenal suppression (eg, patients who have recently taken oral steroids).
Imaging. This may be contributory in some clinical situations. For example, a CXR may be required in suspected congestive cardiac failure, or a CT brain scan in patients with confusion or altered consciousness.
Hyponatraemia symptoms and management1
Back to contentsAn algorithm based on widely accepted recommendations, expert opinion and published consensus guideline has recently been developed for adults:
UK algorithm for the management of inpatients with hyponatraemia
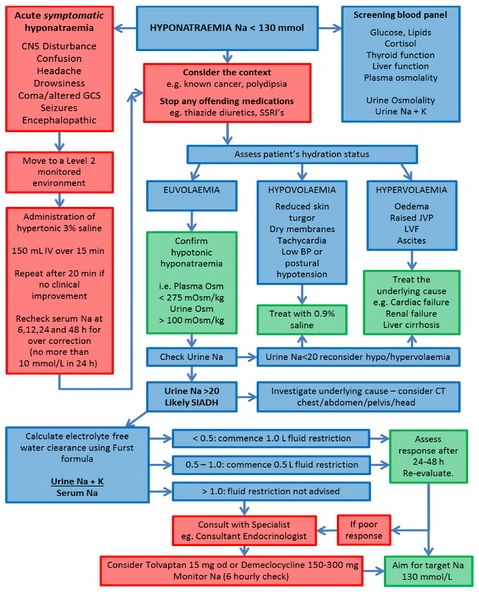
Copyright © 2015 The Authors European Journal of Clinical Investigation published by John Wiley & Sons Ltd on behalf of Stichting European Society for Clinical Investigation Journal Foundation1
Correct underlying cause - eg, stop diuretic. Beware correcting too rapidly.
Acute symptomatic hyponatraemia is a medical emergency.
Treatment involves the use of hypertonic saline to gradually correct the hyponatraemia, with the goal of ensuring that the sodium level does not rise by more than 6 mmol/L in the first six hours or 10 mmol/L in the first 24 hours. Rapid overcorrection leads to a risk of osmotic demyelination syndrome.
If not a severe case then sodium correction method depends on fluid status:
Hypovolaemic:
Intravenous saline replacement - dose is different in adults and children.
As euvolaemia is regained, ADH is suppressed and the resulting diuresis may elevate sodium levels overly rapidly; if so, desmopressin can be given.
Normovolaemic - ie SIADH :
Fluid restrict (500-1000 ml/day for adults). If inadequate consider:
Demeclocycline blocks ADH and induces partial nephrogenic diabetes insipidus. The efficacy of demeclocycline is variable, however, and can depend on the underlying aetiology. Demeclocycline is licensed to treat hyponatraemia associated with SIADH secondary to malignant disease where fluid restriction is ineffective and the patient does not have liver cirrhosis5 .
Vaptans (vasopressin receptor antagonists - eg, tolvaptan) may be useful; however, they can induce thirst, are expensive, have limited availability and potentially may increase sodium levels too rapidly6 .
Hypervolaemic:
The underlying cause should be treated, which is usually heart failure, acute renal injury or liver cirrhosis. Loop diuretics are often beneficial.
Hyponatraemia complications and prognosis
Mild hyponatraemia is associated with gait disturbance in the elderly and with falls. It can also cause a reduction in bone mass and this combination of circumstances increases the incidence of fractures7 .
A sudden fall in serum sodium concentration over a 24- to 48-hour period can result in severe cerebral oedema, leading to cerebral herniation and death.
Chronic hyponatraemia (over more than 48 hours) can result in cerebral oedema but is not associated with brain herniation. Permanent neurological sequelae can arise. Other complications include rhabdomyolysis, seizures and respiratory arrest.
Conversely, too rapid correction of hyponatraemia can cause central pontine myelinolysis (also known as osmotic demyelination syndrome)8 . This is caused by large shifts of intracellular water affecting the pons and other parts of the CNS. Symptoms occur 2-4 days later, typically with quadriplegia and pseudobulbar palsy; however, it can take the form of mutism with paralysis ('locked-in' syndrome). Risk factors for this condition are female gender, hypokalaemia, alcoholism and liver transplant.
Further reading and references
- Shah SA, Ayus JC, Moritz ML; A Survey of Hospital Pharmacy Guidelines for the Administration of 3% Sodium Chloride in Children. Children (Basel). 2022 Jan 3;9(1). pii: children9010057. doi: 10.3390/children9010057.
- Hoorn EJ, Zietse R; Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J Am Soc Nephrol. 2017 May;28(5):1340-1349. doi: 10.1681/ASN.2016101139. Epub 2017 Feb 7.
- Grant P, Ayuk J, Bouloux PM, et al; The diagnosis and management of inpatient hyponatraemia and SIADH. Eur J Clin Invest. 2015 Aug;45(8):888-94. doi: 10.1111/eci.12465. Epub 2015 Jun 28.
- Thompson CJ; Hyponatraemia: new associations and new treatments. Eur J Endocrinol. 2010 Jun;162 Suppl 1:S1-3. Epub 2010 Apr 20.
- Rondon H, Badireddy M; Hyponatremia
- Hyponatraemia; NICE CKS, November 2020 (UK access only)
- Wilke RA; Potential Use of Pharmacogenetics to Reduce Drug-Induced Syndrome of Inappropriate Antidiuretic Hormone (SIADH). J Pers Med. 2021 Aug 28;11(9). pii: jpm11090853. doi: 10.3390/jpm11090853.
- Tzoulis P, Waung JA, Bagkeris E, et al; Real-life experience of tolvaptan use in the treatment of severe hyponatraemia due to syndrome of inappropriate antidiuretic hormone secretion. Clin Endocrinol (Oxf). 2015 Sep 19. doi: 10.1111/cen.12943.
- Tinning CG, Cochrane LA, Singer BR; Analysis of hyponatraemia associated post-operative mortality in 3897 hip fracture patients. Injury. 2015 Jul;46(7):1328-32. doi: 10.1016/j.injury.2015.03.035. Epub 2015 Apr 9.
- Podesta MA, Faravelli I, Cucchiari D, et al; Neurological counterparts of hyponatremia: pathological mechanisms and clinical manifestations. Curr Neurol Neurosci Rep. 2015 Apr;15(4):18. doi: 10.1007/s11910-015-0536-2.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Feb 2027
10 Feb 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free