Inhalers for COPD
Including inhaled steroids
Peer reviewed by Dr Philippa Vincent, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 4 Jul 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
In this series:Chronic obstructive pulmonary diseaseEmphysemaSpirometryMucolyticsOral bronchodilatorsAcute exacerbations of COPD
An inhaler is a device holding a medicine that you take by breathing in (inhaling). Inhalers are often used to treat chronic obstructive pulmonary disease (COPD). There are many different types of inhaler, which can be confusing. The purpose of this leaflet is to give information on the medicines that are inside inhalers, the various types of inhaler device, and some general information about inhalers.

Unsure about mixing medicines?
Check for possible interactions between medicines, supplements and foods before taking them together.
In this article:
Video picks for Chronic obstructive pulmonary disease
This leaflet is about inhalers for chronic obstructive pulmonary disease (COPD). For general information about COPD, see the separate leaflet called Chronic obstructive pulmonary disease. There are also separate leaflets called Asthma and Asthma inhalers.
Continue reading below
Types of COPD inhalers
The medicine inside an inhaler goes straight into the airways when you breathe in. This means that you need a much smaller dose than if you took the medicine as a tablet or liquid by mouth. The airways and lungs are treated but little of the medicine gets into the rest of the body (via the bloodstream).
The proper medicine name is called the generic name. Different drug companies can use the generic medicine and produce different brands - the proprietary medicine names. There are many different brands of inhalers. Inhalers can have generic names and be produced by different drug companies too. For some medicines there are different inhaler devices that deliver the same medicine. This means that there are many types of inhaler available on prescription, all of which are produced in different colours. This can be confusing.
Because there are lots of different coloured inhalers available, it is helpful to remember their names, as well as the colour of the device. This might be important if you need to see a doctor who does not have your medical records (such as in A&E, if you are on holiday, or outside the normal opening hours of your GP surgery). It might be helpful to keep a list of the names of your medicines and inhalers in your wallet or purse. This information will prevent mistakes and confusion.
In the treatment of COPD, the medicines inside inhalers can be grouped into short-acting bronchodilators, long-acting bronchodilators and steroids. There are also combination inhalers containing two or even three different types of medicine.
Short-acting bronchodilator inhalers
An inhaler with a bronchodilator medicine is often prescribed. These relax the muscles in the airways (bronchi) to open them up (dilate them) as wide as possible. People often call them relievers. They include:
Beta-agonist inhalers. Examples are salbutamol (brand names include Airomir®, Salamol®, Salbulin® and Ventolin®) and terbutaline (brand name Bricanyl®). These inhalers are often (but not always) blue in colour. Other inhalers containing different medicines can be blue too. Always read the label.
Antimuscarinic inhalers. For example, ipratropium (brand name Atrovent®).
These inhalers work well for some people but not so well in others. Typically, symptoms of wheeze and breathlessness improve within 5-15 minutes with a beta-agonist inhaler, and within 30-40 minutes with an antimuscarinic inhaler. The effect from both types typically lasts for 3-6 hours. Some people with mild or intermittent symptoms only need an inhaler as required for when breathlessness or wheeze occurs. Some people need to use an inhaler regularly.
The beta-agonist and antimuscarinic inhalers work in different ways. Using two, one of each type, may help some people better than one type alone.
Long-acting bronchodilator inhalers
These work in a similar way to the short-acting inhalers but each dose lasts at least 12 hours. Long-acting inhalers may be an option if symptoms remain troublesome despite taking a short-acting bronchodilator.
Beta-agonist inhalers. Examples are formoterol (brand names Atimos® and Oxis®), salmeterol (brand name Serevent® - a green-coloured inhaler) and indacaterol (brand name Onbrez Breezhaler®). You can continue your short-acting bronchodilator inhalers with these medicines.
Antimuscarinic inhalers. Examples are tiotropium (brand name Spiriva®), glycopyrronium (brand name Seebri Breezhaler®), aclidinium (brand name Eklira Genuair®) and umeclidinium (brand name Incruse®). The inhaler device is green-coloured. If you start this medication, you should stop ipratropium (Atrovent®) if you were taking this beforehand.
Combination inhalers
Many people with COPD need a combination of inhaled medication. Often regular inhaled medication (long acting bronchodilators and steroids) can be given in combination in a single inhaler.
The National Institute for Health and Care Excellence (NICE) recommends that for most people needing combination inhalers, a combination of two long-acting bronchodilators (a beta agonist and an antimuscarinic inhaler) should be offered.
People who should be offered a combination of long-acting beta agonist and antimuscarinic treatment include all patients who have confirmed COPD and who:
Do not have symptoms suggestive of asthma.
Are still breathless or having flare-ups after they:
Have had help to stop smoking (if needed); and
Have had all the immunisations (flu and pneumococcal immunisation) they need; and
Are using short-acting bronchodilator inhalers.
In the past, most patients with COPD needing combination treatment have been given a combination of long-acting bronchodilator and inhaled steroid. The NICE guideline now recommends that this combination should only be considered for patients who have features suggestive of possible asthma.
Steroid inhalers
Are steroid inhalers safe?
A steroid inhaler may help in addition to a bronchodilator inhaler if you have more severe COPD or regular flare-ups (exacerbations) of symptoms. Steroids reduce inflammation.
Steroid inhalers are only used in combination with a long-acting beta-agonist inhaler (this can be with two separate inhalers or with a single inhaler containing two medicines). The main inhaled steroid medications used for COPD are:
Beclometasone. Brands include Clenil Modulite® and Qvar®. These inhalers are usually brown and sometimes red in colour.
Budesonide. Brands include Easyhaler Budesonide®, Novolizer Budesonide® and Pulmicort®.
Fluticasone. Brand name Flixotide®. This is a yellow- or orange-coloured inhaler.
A steroid inhaler may not have much effect on your usual symptoms but may help to prevent flare-ups. So, steroid inhalers are often referred to as preventers.
Combination inhalers are available - duos have combinations of either a long-acting muscarinic antagonist (LAMA), a long-acting beta2 agonist (LABA), and inhaled corticosteroids (ICS) and triple combinations (usually reserved for those with symptoms that are very difficult to control) of a long-acting beta-agonist, a long-acting muscarinic antagonist and a steroid medication.
Examples of combination inhalers are:
Fostair® (formoterol and beclometasone).
Seretide® (salmeterol and fluticasone). This is a purple-coloured inhaler.
Symbicort® (formoterol and budesonide).
Trixeo Aerosphere® (formoterol fumarate dihydrate / glycopyrronium / budesonide)
Combination inhalers are useful if people have severe symptoms or frequent flare-ups. Sometimes it is more convenient to use just one inhaler device.
Different inhaler devices suit different people. They can be divided into four groups.
Pressurised metered dose inhalers (MDIs).
Breath-activated inhalers - MDIs and dry powder inhalers.
Inhalers with spacer devices.
Nebulisers.
Here are some examples of inhaler devices:
The standard metered dose inhaler
MDI inhaler new
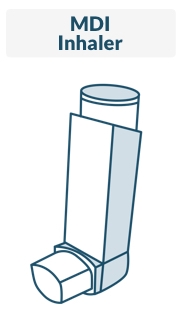
A standard MDI is shown on the right. The MDI has been used for over 40 years and is used to deliver various types and brands of medicines. It contains a pressurised inactive gas that propels a dose of medicine in each 'puff'.
Each dose is released by pressing the top of the inhaler. This type of inhaler is quick to use, small and convenient to carry. It needs good co-ordination to press the canister and breathe in fully at the same time. Sometimes these are known as evohalers.
The standard MDI is the most widely used inhaler. However, many people do not use it to its best effect. Errors include:
Not shaking the inhaler before using it.
Inhaling too sharply or at the wrong time.
Not holding your breath long enough after breathing in the contents.
Until recently, the propellant gas in MDIs has been a chlorofluorocarbon (CFC). However, CFCs damage the Earth's ozone layer, and so are being phased out. The newer CFC-free inhalers work just as well but use a propellant gas that does not damage the ozone layer.
Breath-activated inhalers
Autohaler new

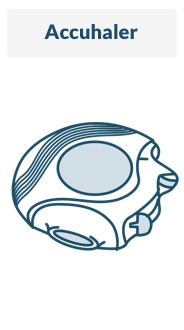
These are alternatives to the standard MDI. Some are still pressurised MDIs but don't require you to press a canister on top. The autohaler shown on the right is an example. Another example of a breath-activated MDI is the Easi-Breathe inhaler®.
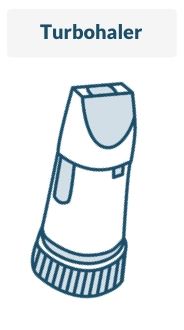
Other breath-activated inhalers are also called dry powder inhalers. These inhalers do not contain the pressurised inactive gas to propel the medicine. You don't have to push the canister to release a dose. Instead, you trigger a dose by breathing in at the mouthpiece. Accuhalers, clickhalers, easyhalers, novolizers, turbohalers, diskhalers and twisthalers are all breath-activated dry powder inhalers. You need to breathe in fairly hard to get the powder into your lungs. Some types are shown below.
Accuhaler new
Turbohaler new
Diskhaler new
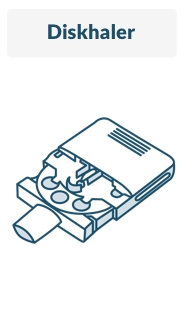
The individual devices all have some differences in how they are operated. However, generally they require less co-ordination than the standard MDI. They tend to be slightly bigger than the standard MDI.
Spacer devices
Asthma spacer device

© The US Food and Drug Administration, Public domain, via Wikimedia Commons
By The US Food and Drug Administration, Public domain, via Wikimedia Commons
Spacer devices are used with pressurised MDIs. There are various types - an example is shown opposite. The spacer between the inhaler and the mouth holds the medicine like a reservoir when the inhaler is pressed. A valve at the mouth end ensures that the medicine is kept within the spacer until you breathe in. When you breathe out, the valve closes. You don't need to have good co-ordination to use a spacer.
There are several different types of spacer. Examples are: Able Spacer®, Aerochamber Plus®, Nebuchamber®, Optichamber®, Pocket Chamber®, Volumatic® and Vortex®. Some of the spacer devices fit all MDIs, others only work (are compatible) with specific brands of inhalers.
Tips on using a spacer device
The following are tips if you are prescribed a holding spacer. These have a valve at the mouth end - the spacer in the picture above is an example.
If your dose is more than one puff then do one puff at a time.
Shake the inhaler before firing each puff.
Start breathing in from the mouthpiece as soon as possible after firing the puff into the device.
Try to hold your breath for a few moments when you have breathed in.
Breathe in and out a few times before firing the next puff. Try to hold your breath for a few moments each time you breathe in.
Check that the valve opens and closes with each breath.
Static charge can build up on the inside of the plastic chamber. This can attract particles of medicine, and reduce the output when the spacer is used. To prevent this, wash the plastic spacer as directed by the maker's instructions. This is usually before first use, and then about once a month and with washing up liquid and water. Let it dry in air without rinsing or wiping.
Nebulisers
Nebulisers are machines that turn the liquid form of your short-acting bronchodilator medicines into a fine mist, like an aerosol. You breathe this in with a face mask or a mouthpiece. Nebulisers are no more effective than normal inhalers.
However, they are extremely useful in people who are very tired (fatigued) with their breathing, or people who are very breathless. Nebulisers are used mainly in hospital for severe attacks of COPD when large doses of inhaled medicines are needed.
They are used less commonly than in the past, as modern spacer devices are usually just as good as nebulisers for giving large doses of inhaled medicines. You do not need any co-ordination to use a nebuliser - you just breathe in and out, and you will breathe the medicine in.
Common questions and further information
Back to contentsDo you get side-effects from inhalers?
At standard inhaled doses, the amount of medicine is small compared with tablets or liquid medicines. Therefore, side-effects tend to be much less of a problem than with tablets or liquid medicines. This is one of their main advantages. However, some side-effects do occur in some people. Read the leaflet that comes with the inhaler for details of possible side-effects. The following just highlights the more common and important ones to be aware of.
One problem that might occur when using a steroid inhaler (especially if you are taking a high dose) is that the back of your throat may get sore. Thrush infection in the mouth may develop. This can usually be treated easily with a course of pastilles that you suck or liquid that you hold in your mouth. You might also notice that your voice becomes hoarse.
If you rinse your mouth with water and brush your teeth after using a steroid inhaler you are less likely to develop a sore throat or thrush. Also, some inhaler devices (such as spacers) are less likely to cause throat problems. A change to a different device may help if mouth problems or thrush occur.
Note: a persistent hoarse voice that does not settle needs further investigation. For example, it can be a sign of cancer of the voice box (larynx). If you have this symptom you should tell your GP.
If you use a high dose of inhaled steroid in the long term it may be a risk factor for 'thinning' of the bones (osteoporosis). You can help to prevent osteoporosis by taking regular exercise, not smoking, and eating a diet with enough calcium. See the separate leaflet called Osteoporosis for more information.
Steroid medicines may aggravate depression and other mental health problems, and may occasionally cause mental health problems. This is more a concern with steroid tablets but, rarely, can be caused by steroid inhalers. Even a severe form of mental health problem called psychosis may (rarely) be triggered by a steroid inhaler. Seek medical advice if worrying mood or behavioural changes occur.
Which is the best inhaler device to use?
This depends on various factors such as:
Convenience. Some inhalers are small, can go easily in a pocket and are quick to use. An example is the standard MDI inhaler. As many as 3 different types of COPD medication can be contained within one device. Having fewer devices to use can be easier for some people.
Your age. Some older people find the MDI inhalers difficult to use.
Your co-ordination. Some devices (in particular the standard MDI) need more co-ordination than others. People with arthritis in their hands may struggle with some devices.
Side-effects. Some of the inhaled medicine hits the back of the throat. Sometimes this can cause problems such as thrush in the mouth. This tends to be more of a problem with higher doses of steroid inhalers. Less of the medicine hits the throat when using a spacer device. Therefore, a spacer device may be advised if you get throat problems, or need a high dose of inhaled steroid.
Some types of inhaler have a bigger carbon footprint than others. That is, they have a bigger effect on climate change (global warming). Everyone has a carbon footprint. If you would like to think about reducing the carbon footprint of your treatment, the decision aid in further reading (below) explains the options. It is intended to help discussions between people and their healthcare professionals.
Often the choice of inhaler is just your personal preference. Most GPs and practice nurses have a range of devices to demonstrate, and let you get a feel for them. If you are unhappy with the one you are using then it is reasonable to try a different type after taking advice from your GP or practice nurse.
Patient picks for Chronic obstructive pulmonary disease

Chest and lungs
Acute exacerbations of COPD
An acute exacerbation is more commonly known as a 'flare-up'. An acute exacerbation of chronic obstructive pulmonary disease (COPD) is a sudden worsening of COPD symptoms compared with the usual severity of symptoms. This often means a worsening of breathlessness and an increase in coughing, with more phlegm (sputum).
by Dr Colin Tidy, MRCGP

Chest and lungs
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a long-term condition of the lungs where the flow of air to the lungs is obstructed. Symptoms include cough and breathlessness. The condition is most often caused by smoking and the most important treatment is to stop smoking. Inhalers are commonly used to ease symptoms. Other treatments such as steroids, antibiotics, oxygen, and mucus-thinning (mucolytic) medicines are sometimes prescribed in more severe cases, or during a flare-up (exacerbation) of symptoms.
by Dr Toni Hazell, MRCGP
Further reading and references
- Chronic Obstructive Pulmonary Disease; NICE Guidance (December 2018 - last updated 2019)
- Chronic Obstructive Pulmonary Disease; NICE CKS, May 2024 (UK access only)
- Celli BR, Wedzicha JA; Update on Clinical Aspects of Chronic Obstructive Pulmonary Disease. N Engl J Med. 2019 Sep 26;381(13):1257-1266. doi: 10.1056/NEJMra1900500.
- British National Formulary (BNF); NICE Evidence Services (UK access only)
- How to use your inhaler video; Asthma and lung UK.
- Asthma/COPD inhalers and climate change; NICE (September 2022)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 3 Jul 2027
4 Jul 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.