Proctalgia fugax and anal pain
Levator ani syndrome
Peer reviewed by Dr Philippa Vincent, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 8 Jul 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Proctalgia fugax is a fleeting pain in the anus. It lasts less than 20 minutes, with no symptoms whatsoever in between episodes. Levator ani syndrome is a pain which lasts for longer. Both are only diagnosed when no other cause is found.
In this article:
Continue reading below
What is proctalgia fugax?
Proctalgia fugax is one of a number of conditions which cause anal or rectal pain (sometimes called ano-rectal pain). It is a type of levator ani syndrome. Proctalgia means pain around the back passage area. Fugax is a Latin word meaning fugitive or fleeting. So it describes a short-lasting pain in the back passage.
Proctalgia fugax is diagnosed when other causes have been excluded. It is thought to be caused by spasms in the muscles of the anal sphincter.
How common is proctalgia fugax?
Back to contentsProctalgia fugax is thought to be quite common. Up to one in five people may experience it at some point.
Continue reading below
What are the symptoms of proctalgia fugax?
Back to contentsPain occurs on several occasions over a few weeks, each time lasting only seconds or minutes. It is a sudden, cramping, severe pain. It may wake you in the night. You may find you get a cluster of attacks together.
In many people who get this condition, the attacks do not happen very often. In between episodes, there is no pain at all. Proctalgia fugax does not cause any bleeding.
Often there is no reason, but the pain can be triggered in some cases by the following:
Having sex.
Opening your bowels.
Being constipated.
Having a period.
Stress.
What causes proctalgia fugax?
Back to contentsThis is not exactly understood. It is believed to be due to spasms of the muscles of the anus. The muscles here are very strong, as these are the muscles you use to hold your poo in, or relax to let the poo out.
Most of the time it is not obvious what has set it off. In some people, it starts after an operation - for example, an injection for piles, or after a hysterectomy. It seems to be more common in people who have IBS, and in people who have anxiety symptoms.
Continue reading below
How is anal pain investigated?
Back to contentsWhen you visit your doctor, you will be asked questions about the pain you are experiencing. For example, how long it lasts, if it is related to opening your bowels, etc. The doctor will also want to know if you have other symptoms, in particular bleeding. Proctalgia fugax and levator ani syndrome do not cause any bleeding from your back passage.
The doctor will then need to examine you. You will be asked to lie on the couch, usually on your side, with your knees curled up towards your chest. The doctor will look at the outside of your anus first, looking for lumps, bumps, fissures and skin rashes.
They will want to feel inside with a gloved finger, checking for lumps, tenderness and bleeding. They may look inside your anus and rectum with an instrument called a proctoscope. This is a short rigid see-through tube, which allows them to see the inside of just the lower few inches of your gut.
If further tests are needed, you may then be referred to a specialist, usually a gastroenterologist or colorectal surgeon. Further tests might be advised. This could include:
A sigmoidoscopy. This is an examination with a camera on a longer tube, which can pass further up inside your gut.
Anorectal manometry. This is a test used to measure the pressure of anal muscle contractions.
Not everybody needs all these tests. If you have occasional fleeting pains, no bleeding, and a normal examination, you are likely to have proctalgia fugax and will not need any more tests. If this is the case, you would be advised to return to see the doctor if anything changes (for example, if you get any bleeding, or if the pain becomes more persistent).
What is the treatment for proctalgia fugax?
Back to contentsOften no treatment is needed. For many people, the episodes are infrequent. If you know it isn't anything to worry about, you may not need any treatment. You know the pain will settle quickly on its own.
In a few people, it can be more troublesome, and may need treatment. There are no proven treatments for this condition, but options include:
Using a salbutamol inhaler. This is the same inhaler used by people with asthma. It opens up airways by relaxing the muscle in them, so it makes sense that it can work on the muscles around the anus as well.
A cream which works on the blood vessels around the anus, such as glyceryl trinitrate or diltiazem cream.
An injection into the nerve to make it less sensitive.
What is the difference between proctalgia fugax and levator ani syndrome?
Back to contentsIt's mostly about how long the pain lasts. If you have proctalgia fugax, you have short spells of intense pain in your back passage, but it's all over within seconds or minutes, and you feel absolutely normal in between attacks. You may get clusters of episodes, several over a week or two, but most people don't get the pain very often.
Levator ani syndrome pain tends to be worse when sitting, and lasts at least 20 minutes. More often it's there all the time, or comes and goes persistently. It is usually an aching type of pain.
How common is levator ani syndrome?
Back to contentsLevator ani syndrome is less common, affecting around 6 in 100 people.
What are the symptoms of levator ani syndrome?
Back to contentsThe levator ani is a muscle. It is part of the pelvic floor group of muscles which is a sling-like support across your pelvis - as in the image below. It is the muscle group around your anus and rectum.
Levator ani syndrome: anal and rectal muscles
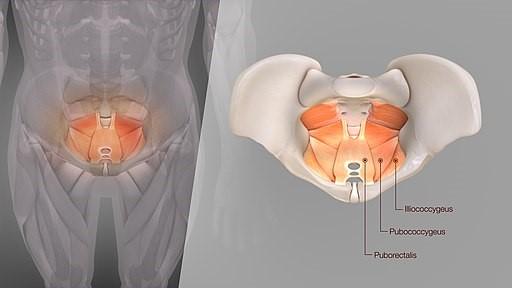
© Scientificanimations.com, CC BY-SA 4.0, via Wikimedia Commons
Image by scientificanimations.com, CC BY-SA 4.0, via Wikimedia Commons
If you have levator ani syndrome, you get an aching pain high up in your back passage. It tends to be worse when you are sitting down, and walking around can make it feel better. The pain is constant or regular, and lasts (unlike proctalgia fugax) for longer than 20 minutes. It continues, either constantly or on and off, for months.
Levator ani syndrome is also known as chronic anal pain syndrome.
What is the treatment for levator ani syndrome?
Back to contentsOptions include:
Biofeedback therapy. This is a type of therapy whereby you learn how to relax your pelvic floor muscles. Electrodes are attached inside providing a trace which shows you what happens as you try to relax and contract the muscles. You need several training sessions to learn how to control the muscles well. This is the treatment option for which there is most encouraging evidence.
Electrogalvanic (electrical) stimulation. This involves stimulation of the anus by an electric current through a probe placed inside it. This is thought to be less effective than biofeedback.
Botox® (botulinum toxin). An injection of Botox® helps to reduce episodes in some cases.
Stimulation of specific nerves. This involves trying to de-sensitise some of the nerves in the area.
A salbutamol inhaler (as above).
Most options require you to be referred to a specialist for advice and for the treatment to be arranged.
Is proctalgia fugax or levator ani syndrome serious?
Back to contentsThat depends what you mean. It is not serious in the way that cancer is serious, for example. Proctalgia fugax doesn't usually affect your life too much. Once your doctor has established nothing more serious is the cause then it is usually an occasional problem for most people.
Levator ani syndrome can, however, have a significant impact on your life. It can wake you up at night, and prevent you doing things that involve sitting. This can get in the way of work, and leisure activities such as cycling, for example. It can, for some people, really interfere in the quality of life, and so for those people, yes it can be serious.
What is the outlook for proctalgia fugax or levator ani syndrome?
Back to contentsThis is variable. Proctalgia fugax usually isn't a long-term problem. Either you get a few episodes here and there with long spells of no problems in between, or it goes away altogether. Each individual episode, by definition, is very short-lived.
Levator ani syndrome can drag on for a long time in some people and it may be difficult to find a treatment which helps.
What other conditions cause anal pain?
Back to contentsColon and Rectum

As you can see in the diagram above, your anus is at the very end of your gut, where it opens out on your bottom. The anal canal is the short tube just above and leads to the rectum just above it.
There are many conditions which can cause a pain in the bottom area. In most of these an abnormality is seen or felt on examination or investigation. Possible causes include:
Piles (haemorrhoids). These are a common cause of anal pain, particularly when one of the piles gets a blood clot in it (a thrombosed haemorrhoid). If this is the case, you may be able to feel a tender lump.
Anal fissure. This is a split in the skin around the anus, usually caused by passing a hard poo. The pain is much worse when you do a poo, and there may be some blood when you poo.
Cancer. Cancer of the anus or rectum can cause pain but other causes are more likely and there are usually additional symptoms. It is usually a more constant pain, and may be worse when you poo. You may have blood on your underwear or mixed with your poo. .
Anogenital warts. These are a sexually transmitted infection (STI) and if you have them you can usually see or feel small bumps around the anus. Other STIs such as herpes can also cause a pain in this area. Again, usually you can see a blister or blistery rash.
Crohn's disease and ulcerative colitis. These are conditions where the gut is inflamed. They usually cause other symptoms such as diarrhoea, blood and mucus in the poo, and tummy pains.
Rectal prolapse. This is a condition where the muscles of the end of the gut are weak, and some of the inside of the gut may come out (prolapse). You would notice you have difficulty holding your stools in, and you may feel a lump.
Prostatitis. This is an inflammation or infection of the prostate gland. Men only - women don't have a prostate gland.
Coccydynia. This is a pain around the tailbone (coccyx) and is very painful when you sit down. Usually this is set off by a fall on to your bottom.
Irritable bowel syndrome (IBS). Usually, IBS causes loose stools or constipation, and tummy pains and bloating, but it may sometimes be accompanied by pain in the anal area.
An infection, such as a collection of pus (an abscess).
The conditions proctalgia fugax and levator ani syndrome are what is left when all these causes have been ruled out. They are a "diagnosis of exclusion", meaning there is no specific test for them, and that all other possible causes must be ruled out first. This leaflet is mainly about these two conditions.
Why do they happen?
The cause isn't really known. It's thought to be caused by a tightening or spasm of the muscles inside your bottom. People often wonder what caused this to start, but often no trigger or cause is found.
Video picks for Anal and rectal problems
Patient picks for Anal and rectal problems

Digestive health
Anal fissure
An anal fissure is a small tear in the lining of the skin around the back passage (anus). An anal fissure that lasts more than six weeks is called a chronic anal fissure. For most people, the anal fissure heals quite quickly but some form of treatment is often needed. Anal fissures may keep coming back.
by Dr Hayley Willacy, FRCGP

Digestive health
Anal fistula
An anal fistula is usually caused by an infection near your back passage (anus) that causes a collection of pus (abscess) in the nearby tissue. When the pus drains away, it can leave a small channel (fistula) behind. An anal fistula may also be associated with certain long-term bowel conditions.
by Dr Hayley Willacy, FRCGP
Further reading and references
- Knowles CH, Cohen RC; Chronic anal pain: A review of causes, diagnosis, and treatment. Cleve Clin J Med. 2022 Jun 1;89(6):336-343. doi: 10.3949/ccjm.89a.21102.
- Hite M, Curran T; Biofeedback for Pelvic Floor Disorders. Clin Colon Rectal Surg. 2021 Jan;34(1):56-61. doi: 10.1055/s-0040-1714287. Epub 2020 Sep 4.
- Grimes WR, Stratton M; Pelvic Floor Dysfunction
- Guidelines on Chronic Pelvic Pain; European Association of Urology (2022)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 6 Jul 2027
8 Jul 2024 | Latest version
9 Jul 2017 | Originally published
Authored by:
Dr Mary Harding, MRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.