Mallory-Weiss tear
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Philippa Vincent, MRCGPLast updated 23 Mar 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
In this series:Vomiting blood
Mallory-Weiss syndrome (also called Mallory-Weiss tear) is the name given to bleeding and other symptoms caused by a tear in the lining of the upper part of the gut (gastrointestinal tract). It is usually diagnosed by having a test called a gastroscopy (endoscopy). This involves a tube being passed down through the gullet (oesophagus) into the stomach. In many cases, the bleeding has stopped by the time gastroscopy takes place and specific treatment is not needed. The tear usually heals by itself after a few days.
In this article:
Video picks for Other digestive conditions
What is Mallory-Weiss syndrome?
Upper gut

Mallory-Weiss syndrome (also called Mallory-Weiss tear) is the name given to bleeding and other symptoms caused by a tear in the lining of the upper part of the gut (gastrointestinal tract). The upper gut consists of the gullet (oesophagus), stomach and duodenum.
The tear usually occurs at one of two particular places in the upper gut:
The gastro-oesophageal junction - the part of the upper gut where the gullet joins the stomach; or
Within the lining of the upper part of the stomach.
Mallory-Weiss syndrome was first described in 1929 by two doctors called Mallory and Weiss. They had noticed it in people retching and being sick (vomiting) after bingeing on alcohol.
What causes Mallory-Weiss syndrome?
Back to contentsThe tear in the lining of the gut that occurs in Mallory-Weiss syndrome can be caused by anything that leads to a sudden rise in pressure in the stomach or the lower part of the gullet (oesophagus). Repeated vomiting and retching after binge drinking, because of severe morning sickness during pregnancy, or because of bulimia nervosa (episodes of binge eating followed by self-induced vomiting) are among the most common causes of Mallory-Weiss syndrome.
Any condition that causes vomiting or coughing, however, can cause this tear to happen. Less commonly it happens because of violent coughing, hiccupping, excessive straining or heavy lifting. Sometimes an obvious cause for the tear cannot be found.
Continue reading below
Who does Mallory-Weiss syndrome affect?
Back to contentsThe problem tends to affect people aged in their 30s to 50s, although it can occur at any age. It is more common in men than in women and is also more common in people with a hiatus hernia. (A hiatus hernia occurs when part of the stomach pushes up into the lower chest through a weakness in the diaphragm - the large flat muscle that lies between the lungs and the tummy area. See the separate leaflet called Hiatus Hernia for more details.) It is also more common in patients who drink alcohol above recommended limits.
What are the symptoms of Mallory-Weiss syndrome?
Back to contentsMost people with Mallory-Weiss syndrome will bring up (vomit) an amount of bright red blood. This will often happen after a bout of normal retching or vomiting. The amount of bleeding (and so blood vomited as a result) varies from person to person. Most people have just a small amount of bleeding but sometimes there can be a lot of blood lost.
Other symptoms can be:
Dark black or tarry-coloured foul-smelling stools (faeces) - this is known as melaena and is caused by blood from the upper part of the gastrointestinal tract changing as it moves through the lower part.
Severe pain in the upper part of the tummy (abdomen).
Dizziness and light-headedness due to the blood loss.
Fainting.
Note: there are many other conditions that can lead to vomiting blood. For example, a stomach ulcer, stomach inflammation (gastritis) or inflammation of the gullet (oesophagus). See the separate leaflet called Vomiting Blood (Haematemesis) for more details. About 5% of cases of bleeding from the upper part of the gut are caused by a Mallory-Weiss tear. Medical attention should be sought quickly with the above symptoms.
Continue reading below
How is Mallory-Weiss syndrome diagnosed?
Back to contentsMallory-Weiss syndrome is usually diagnosed by having a gastroscopy (sometimes known as an endoscopy or an OGD - oesophago-gastro-duodenoscopy).
A gastroscopy is a test where a clinician looks into the upper part of the gut using an endoscope. . An endoscope is a thin, flexible telescope which is about as thick as a little finger.
The endoscope is passed through the mouth, into the gullet (oesophagus) and down towards the stomach and duodenum. The tip of the endoscope contains a light and a tiny video camera so the operator can see inside the gut. The endoscope also has a side channel down which various instruments can pass in order to be used by the operator.
For further details see the separate leaflet called Gastroscopy (Endoscopy).
A gastroscopy allows the operator to see if a Mallory-Weiss tear is present in the gut lining, as well as its location. They will also be able to see if the tear is still bleeding.
Endoscopic image of Mallory-Weiss tear
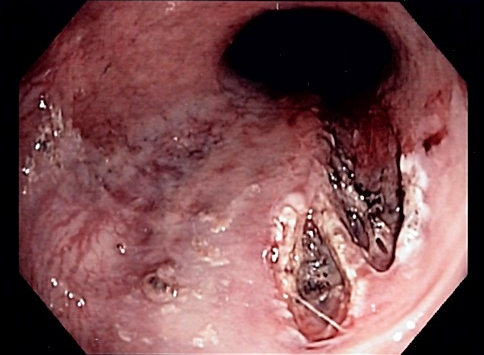
© Samir,CC BY-SA 3.0, via Wikimedia Commons
By Samir, CC BY-SA 3.0, via Wikimedia Commons
What is the treatment for Mallory-Weiss syndrome?
Back to contentsThe first thing that doctors and nurses will do if they suspect Mallory-Weiss syndrome is to make sure that the person's condition is stable. If a lot of blood has been lost, fluids may be given into the veins (intravenously). Sometimes a transfusion of blood may be given. Blood pressure and pulse rate will be closely watched so that the medical staff can check the response to any treatment.
Blood tests will usually be carried out - for example, to check for anaemia (to see how much blood has been lost because of the bleeding) and to check that the blood is clotting normally. Medication may be given to help with symptoms of feeling sick (nausea) or being sick (vomiting).
If people do not show any signs of ongoing bleeding and their condition is stable, they may not be admitted to hospital but may be followed up as an outpatient.
Management will depend on whether the Mallory-Weiss tear is still bleeding when the gastroscopy is carried out. In many cases the bleeding has stopped by the time gastroscopy takes place.
If the Mallory-Weiss tear is still bleeding
If the tear is still bleeding, treatment to stop the bleeding is usually given during the gastroscopy. A number of different treatments are available including:
The tear can be repaired, or closed, using special metal clips passed via the side channel . This is known as haemoclipping.
A band can be used to tie off a bleeding blood vessel. This is known as band ligation.
A heater probe may be passed down the side channel of the endoscope to apply a heat source to the bleeding blood vessels, to stop the bleeding.
Adrenaline (epinephrine) may be injected around the bleeding point. This medication causes closure (constriction) of the bleeding blood vessels thus stopping the bleeding
A combination of these treatments may be used
Very rarely, the above treatments do not stop the bleeding. In this case a procedure known as angiography with embolisation may be used. A special dye is injected into the bloodstream and X-rays are taken which show up the blood vessels (called angiography). In this way, doctors can see where the bleeding is coming from. A substance is then injected directly into the bleeding blood vessel either to stop the bleeding or to block it off (this is called embolisation).
Rarely, surgery is needed to treat Mallory-Weiss syndrome by sewing up the tear if other treatments have failed to stop the bleeding
If the Mallory-Weiss tear has stopped bleeding
If the tear is found to have stopped bleeding by the time gastroscopy takes place then no specific treatment may be needed. The tear should heal by itself. The person may be observed in hospital for a period of time so that they can be monitored closely to ensure that bleeding doesn't return (recur). Medication to suppress stomach acid may be given to help the tear heal.
What is the outlook for Mallory-Weiss syndrome?
Back to contentsThe outlook (prognosis) is generally very good. In most people, the bleeding stops by itself and no specific treatment is needed. Mallory-Weiss tears usually heal quickly (within a few days).
Can Mallory-Weiss syndrome return?
Back to contentsIt is not common for Mallory-Weiss syndrome to return (recur). However, if someone has had Mallory-Weiss syndrome in the past, there is the possibility of the condition recurring It is more likely to occur again if the bleeding was extremely heavy the first time.
Patient picks for Other digestive conditions

Digestive health
Abdominal masses
An abdominal mass is a lump felt in the tummy (abdomen). There are many different causes of an abdominal mass. Urgent medical attention should be sought if a new mass is found in the abdomen.
by Dr Philippa Vincent, MRCGP

Digestive health
Chronic pancreatitis
Chronic pancreatitis can cause tummy (abdominal) pain, poor digestion, diabetes and other complications. Alcohol is the common cause. Treatment includes painkillers, other medication and, most importantly, stopping alcohol drinking for good. Surgery is sometimes needed.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Holster IL, Kuipers EJ; Management of acute nonvariceal upper gastrointestinal bleeding: current policies and future perspectives. World J Gastroenterol. 2012 Mar 21;18(11):1202-7.
- Wilkins T, Khan N, Nabh A, et al; Diagnosis and management of upper gastrointestinal bleeding. Am Fam Physician. 2012 Mar 1;85(5):469-76.
- Acute upper gastrointestinal bleeding in over 16s: management; NICE Clinical Guideline (August 2016)
- Rawla P, Devasahayam J; Mallory Weiss Syndrome. Sovah Health, Martinsville, VA, University of South Dakota, 2022.
- National Clinical Guideline Centre (UK) - Acute Upper Gastrointestinal Bleeding: Management; London: Royal College of Physicians (UK), 2012
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 21 Mar 2028
23 Mar 2023 | Latest version
15 Dec 2011 | Originally published
Authored by:
Dr Michelle Wright, MRCGP

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.