Audit and audit cycle
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 7 Feb 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Continue reading below
What is an audit?
Audit in healthcare is a process used by health professionals to assess, evaluate and improve care of patients in a systematic way. Audit measures current practice against a defined (desired) standard. It forms part of clinical governance, which aims to safeguard a high quality of clinical care for patients.1
Key features of audit are:1
Audit asks the question: 'Are we actually doing what we believe is the right thing, and in the right way?' (unlike research, which asks 'What should we be doing?').
Audit can be used to evaluate various aspects of patient care:
Structure of care - eg, the availability of a smoking cessation clinic in a locality.
Process of care - eg, waiting times for an appointment at the smoking cessation clinic.
The outcome of care - eg, the number of smokers who quit smoking for one year.
Audit should be transparent and non-judgemental. The aim is to find out how the present provision compares with the desired standard. This information can then be used to plan improvements in the service. It is not intended to cause confrontation or blame.
Requirements for audit by UK doctors
Back to contentsThe General Medical Council (GMC) states that, as part of good medical practice, in maintaining, developing and improving performance, doctors are required to take steps to monitor, maintain, develop, and improve performance and the quality of work, including taking part in systems of quality assurance and quality improvement to promote patient safety across the whole scope of your practice. This includes:2
Contributing to discussions and decisions about improving the quality of services and outcomes.
Taking part in regular reviews and audits of work, and the team’s work, and responding constructively to the outcomes, taking steps to address problems, and carrying out further training where necessary.
Audit is also a part of the revalidation process for GPs.3 4
Audits should be full cycle - ie initial audit, change implemented, re-audit to demonstrate improvement.
There should be at least one complete audit in each five-year revalidation cycle.
Audits may be undertaken by several GPs working as a team. However, you must have been involved in all key parts of the audit, and explicitly state how you were involved.
Key points to audit for GPs are:
Relevance of the topic chosen.
Appropriateness of the standards of patient care set.
Reflection on current care and the appropriateness of changes planned.
Implementation of change for the GP's patients.
Demonstration of change by the GP.
Description of the audit should include:
Title.
Reason for choice.
Dates of first and second sets of data collection.
Criteria to be audited and standards set with justification, or clinical condition to be audited, or process of care to be audited (all with reference to evidence-based guidelines).
Results of the first data collection and comparison to standards which have been set.
Summary of subsequent discussion, and plan of change agreed.
Changes implemented.
Results of second data collection and comparison to standards set.
Quality improvement achieved.
Reflection on audit in terms of the principles of good medical practice (ie knowledge, skills and performance, safety and quality, communication, partnership and teamwork, and maintaining trust).
Continue reading below
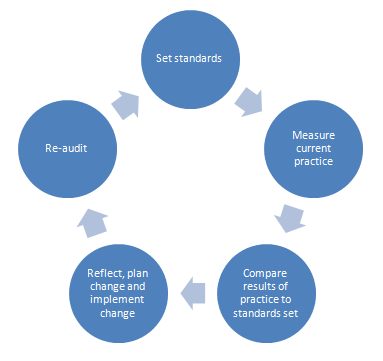
The audit cycle1
Back to contentsStage 1 - preparation
Choose a topic:
Preferably one which is a high priority for your organisation.
This may involve areas in which there is a high volume of work, high risks or high costs of care, or an area identified as a priority by patients.
Identify available resources - eg:
Your organisation may have a local audit lead or office.
There may be existing guidelines defining desired standards for the topic you have chosen.
Stage 2 - select criteria
Define the criteria. This should be in the form of a statement - eg: 'All patients with hypertension who smoke should be offered smoking cessation advice.'
Define the standard - usually a target (percentage). This may be a minimum standard or an optimal one, depending on the clinical scenario.
For definitions of criteria and standards, see those headings, below.
Stage 3 - measuring level of performance
Collect the data:
May be from computerised records, manual collection, or both.
May be retrospective or prospective.
Analyse the data collected:
Compare actual performance with the set standard.
Discuss how well the standards were met.
If the standards were not met, note the reasons for this (if known).
Stage 4 - making improvements
Present the results and discuss them with the relevant teams in your organisation.
The results should be used to develop an action plan, specifying what needs to be done, how it will be done, who is going to do it and by when.
Stage 5 - maintaining improvements
This follows up the previous stages of the audit, to determine whether the actions taken have been effective, or whether further improvements are needed.
It involves repeating the audit (ie targets, results, discussion); hence the terms 'audit cycle' or 'audit spiral'.
An example of this cycle in practice is described by Benjamin.1
The audit cycle: at a glance
Audit cycle
Notes and advice for audit
Back to contentsDefinitions
Criteria
A definable measurable item of healthcare that describes quality and which can be used to assess it - eg, the number of people with coronary heart disease who have had their lipids checked within the preceding one year.
It is often best expressed as a statement - eg: 'All patients with coronary heart disease should have had their lipids checked annually.'
Criteria should be evidence-based wherever possible.
Standards
Describes the level of care to be achieved for any particular criterion.
For example, in the above scenario the standard chosen might be 80% (allowing for a number of patients to opt out, or for patients in whom testing is not appropriate - eg, those with terminal illness). For other scenarios (eg, number of patients with chest pain reaching hospital within a set time), higher standards may be appropriate.
Advice on planning1
When constructing criteria and standards:
Make unambiguous statements.
Refer to the literature indicating current practice and guidelines - eg, National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN) and Royal College of General Practitioners (RCGP) guidelines.
NICE now produces clinical audit tools for a number of standard topics. They contain resources including standards based on NICE guidelines, data collection sheets, an action plan template, and a clinical audit report.5
Choose criteria and standards in line with current practice.
The choice of standard can be controversial and there are three options:
A minimum standard: the lowest acceptable standard of performance. Minimum standards are often used to distinguish between acceptable and unacceptable practice.
An ideal standard: the care it should be possible to give under ideal conditions, with no constraints.
An optimum standard: lies between the minimum and the ideal. Represents the standard of care most likely to be achieved under normal conditions of practice. Setting an optimum standard requires consensus with other members of the team.
Collecting data:
Identify which data need to be collected, how and in what form, and who is going to collect them.
Only collect information that is absolutely essential.
Tips for a successful audit1
Adequate training and support for all staff involved.
Choose the topic carefully:
Audits are more likely to be effective where adherence to recommended practice is low.
Choose a topic with high priority (as above).
Enlist support from your organisation.
A team approach - involve all relevant staff.
Agree confidentiality of findings and a 'no blame' culture.
Allow sufficient time - protected time is helpful.
Good data collection and/or IT systems are required.
Set realistic standards (optimum rather than ideal) that are agreed by the team.
Deliver intensive feedback.
The RCGP has developed resources for supporting successful audit of clinical practice.
Further reading and references
- Principles for Best Practice in Clinical Audit; NICE, 2002
- Clinical Audit How To Guides; University Hospitals Bristol
- Audit and service improvement; National Institute for Health and Care Excellence (NICE).
- Benjamin A; Audit: how to do it in practice. BMJ. 2008 May 31;336(7655):1241-5.
- Good medical practice; General Medical Council (GMC). 2024.
- Supporting information for appraisal and revalidation; General Medical Council
- Revalidation; Royal College of General Practitioners
- Audit and service improvement; National Institute for Health and Care Excellence (NICE).
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 5 Feb 2029
7 Feb 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free