Ankle fractures
Peer reviewed by Dr Laurence KnottLast updated by Dr Colin Tidy, MRCGPLast updated 15 Feb 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Ankle injury article more useful, or one of our other health articles.
In this article:
What is an ankle fracture?
An ankle fracture is a break in one or more of the bones of the ankle joint - the tibia, fibula and talus. Two joints are involved in ankle fractures:
Ankle joint - where the tibia, fibula and talus meet.
Tibiofibular joint - fibrous joint held together by ligaments (syndesmosis joint).
The ankle is a complex joint that is capable of a wide range of movement: flexion, extension, inversion and eversion as well as a combination of these movements. This allows locomotion and balance on both level and uneven ground. The ankle takes the full weight of the body and is subject to considerable force, particularly in running and jumping.
Many ankle injuries are managed conservatively. However, obvious clinical deformity (ie dislocation) or injuries with neurovascular compromise of the foot are an orthopaedic emergency, for which immediate reduction is required (see 'Management' section, below).
See the separate Ankle Injuries article for the assessment of ankle fractures and sprains (this details the history, examination, investigation and differential diagnosis of ankle injuries and the management of ankle sprains and strains).
Anatomy of the ankle joint
Back to contentsTwo joints allow movement of the ankle:
The true ankle joint (tibiotalar joint) - articulation is between the lower end of the tibia, the malleoli and the body of the talus. This joint allows dorsiflexion and plantar flexion of the ankle.
The subtalar joint - articulation is between the talus and calcaneus. This joint allows inversion and eversion of the ankle.
The distal tibia has a prominent medial malleolus and a less prominent posterior malleolus. The distal fibula is known as the lateral malleolus. The joint capsule and the surrounding ligaments stabilise the ankle. The distal fibula is joined to the distal tibia by the anterior and posterior inferior tibiofibular ligaments, an inferior transverse ligament and a syndesmosis ligament. The anterior and posterior talofibular ligaments join the fibula to the talus. The talus is joined to the calcaneus by the calcaneo-fibular ligament. The deltoid ligament joins the medial malleolus to the talus, calcaneus and navicular bones.
Joints of the ankle and foot
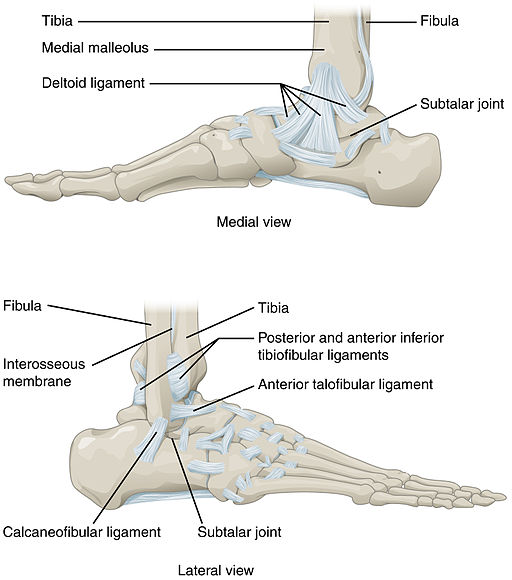
© OpenStax College,Anatomy & Physiology, Connexions Website, Jun 19, 2013, via Wikimedia Commons
By OpenStax College, Anatomy & Physiology, Connexions Website, Jun 19, 2013, via Wikimedia Commons
Continue reading below
Symptoms of an ankle fracture1
Back to contentsSevere sprains and fractures can present in a similar manner. Typical symptoms are of:
Immediate, severe pain, which may extend from foot to knee.
Swelling, localised or along the leg.
Bruising.
Tenderness.
Inability to weigh bear, although patients do sometimes walk on ankle fractures.
Joint deformity.
Ankle fracture symptoms2
Back to contentsHistory and examination of ankle injuries are discussed in detail in the separate Ankle Injuries article. However, some key points for suspected ankle fractures are detailed below.
Principles of care for ankle fractures
When assessing ankle fractures, consider:
What was the mechanism of injury (inversion, eversion, plantar flexion, dorsiflexion)? This can help to determine the nature and severity of the injury.
What happened afterwards? Was the patient able to weight bear immediately? Did they need help to walk? If it was a sports injury, were they able to continue?
Did the ankle swell? Was the swelling immediate? (Immediate swelling is due to bleeding.)
Are there associated injuries (ligamentous, capsular, vascular)?
Is there a history of osteoporosis or of risk factors for osteoporosis?
Does the ankle need immobilising?
Is specialist orthopaedic referral needed?
Examination
Ankle fractures and ankle sprains can present in a similar way. Features that may suggest a fracture include obvious deformity, swelling, bruising, inability to weight bear and bony tenderness.
The patient should also be assessed and examined for co-existing injuries.
Inspection:
Did the patient walk in? If so, with how much discomfort and disability?
Look at the ankle. Is there obvious deformity?
Is there swelling or bruising? Does it look compatible with the mechanism of injury?
Is an effusion present? This may be a fullness either side of the Achilles tendon.
Are there any open wounds?
Palpation:
Palpate for crepitus and tenderness, especially over the malleolar regions, over the anterior tibiofibular ligament, the whole length of the fibula and the base of the 5th metatarsal. Does calcaneal pressure elicit pain?
Examine for neurovascular injury:
Assessment of neurovascular status is by sensation over the dorsal and plantar surfaces of the foot, measuring capillary refill in all digits, and palpating the distal pulses (the dorsalis pedis artery is absent in 2-3% of the population). Vascular compromise is the urgent concern in dislocations and fracture-dislocations. Sural nerve and peroneal nerve palsies are a rare complication of severe sprains.
Movement/power:
These cannot be tested in most cases as the joint may be swollen, painful, fractured or dislocated.
Examine for co-existing injuries:
Pay special attention to the ipsilateral knee and foot.
Check for tenderness (fracture) of the proximal fibula.
Specific tests of tendon function are listed in the separate Ankle Injuries article.
Examination of the uninjured ankle may give an indication of the normal range of movement and power.
Investigations3 4 5
Not everyone with an ankle injury needs to have an X-ray. Clinically it may be very difficult to differentiate a fracture from a severe sprain without an X-ray unless there is obvious distortion or instability. The Ottawa Ankle Rules were introduced in 1992 as a guideline with which to reduce costs and waiting times when ruling out serious ankle and midfoot fractures in the non-athletic, adult population:
Ankle radiography is indicated only if a patient has pain in the malleolar zone and any of the following findings:
Bone tenderness at the posterior edge or tip of the medial or lateral malleolus, or
Inability to bear weight (four steps) immediately after injury and at the time of assessment.
Foot radiography is indicated only if a patient has pain in the midfoot zone and any of the following findings:
Bone tenderness at the base of the fifth metatarsal or over the navicular bone (located on the top inner side of the middle of the foot), or
Inability to bear weight (four steps) immediately after injury and at the time of assessment.
The Buffalo Rule was derived to increase the diagnostic accuracy of the Ottawa Ankle Rules, with the point tenderness criterion directed to the crest or midportion of the malleoli (distal 6 cm of the fibula and tibia), reducing the likelihood of palpating over injured ligament structures6 .
Assessment of the Ottawa Ankle Rules suggests that they are valid in children and they are in widespread clinical use, as they massively reduce costs and unnecessary X-ray exposure7 .
Imaging
If an X-ray is performed, anteroposterior (AP), lateral and mortise (oblique) views can be taken. For the mortise view, the foot is rotated about 15° internally. This allows a better view of the ankle mortise.
If one injury is seen on X-ray, always look for a second.
CT and MRI scanning are sometimes needed for fracture diagnosis (eg, talar fractures)and assessment of ligamentous or intra-articular injuries.
Continue reading below
Classification of ankle fractures8
Back to contentsThere are various ways of classifying ankle fractures.
The Danis-Weber classification
This classification is simple and is probably the most useful for primary care (see below). It is based on the fibular fracture in relation to the syndesmosis on radiography (this refers to the syndesmosis between tibia and fibula):
Type A: fibular fracture below the tibiofibular syndesmosis, which is intact.
Type B: fibular fracture at the level of the syndesmosis.
Type C: fibular fracture above the syndesmosis, indicating rupture of the syndesmosis.
A simple classification based on the malleoli involved
This can be used, as it has implications for joint stability and further management options:
Monomalleolar fracture.
Bimalleolar fracture:
Sometimes the deltoid ligament ruptures instead of the medial malleolus being fractured; this is equivalent to a bimalleolar fracture and is treated similarly.
Trimalleolar fracture (the third malleolus being the 'posterior malleolus', ie the posterior part of the distal tibia).
The Lauge-Hansen system
This system is also in popular use: it classifies fracture types according to the mechanism of injury as it relates to the position of the foot (the most common type is supination-external rotation).
Some eponymous ankle fractures and associated fractures
Pott's fracture: this is a term less used now. It loosely refers to fractures and fracture-dislocations of the distal tibia and fibula (bimalleolar fractures), involving at least two elements of the ankle ring. These fractures are unstable and require urgent treatment.
Pilon fracture: a fracture of the distal tibial metaphysis and also disruption of the talar dome. The talus is 'driven' into the tibia as may happen in a fall from a height or a foot braced against the floor of a car in a collision. The fracture may be open. There may be associated injuries - eg, spinal compression fractures or pelvic injury.
Snowboarder's fracture: this is a fracture of the lateral process of the talus produced by dorsiflexion and inversion of the ankle. The patient complains of lateral ankle pain. The fracture may not be evident on X-ray and may need CT scanning for diagnosis. Have a high index of suspicion for this fracture in snowboarders who complain of lateral ankle pain.
Maisonneuve fracture: this may be associated with ankle fracture and is a spiral fracture of the proximal third of the fibula with a tear of the distal tibio-fibular syndesmosis and the interosseous membrane. There is an associated fracture of the medial malleolus or rupture of the deep deltoid ligament. This type of injury can be difficult to detect.
Jones fracture may also be associated with ankle fracture and should be excluded by palpating the foot. It is a fracture of the meta-diaphyseal part of the fifth metatarsal - this is at the proximal end, near the mid-portion of the foot.
Ankle fracture treatment and management8 9
Back to contentsInitial management
As with any trauma patient, carry out a primary survey following the 'ABCDE' principles of trauma care.
Assess clinically for obvious deformity and for neurovascular status:
If there is neurovascular compromise or dislocation (obvious deformity) of the joint, the fracture should be reduced immediately - before X-ray - under analgesia or sedation.
Displaced fractures should be reduced as soon as possible after initial assessment - this reduces pain/swelling and may prevent skin necrosis.
Assessment of neurovascular status is by testing sensation over the dorsal and plantar surfaces of the foot, measuring capillary refill in all digits, and palpating the distal pulses (although the dorsalis pedis artery is absent in 2-3% of the population).
Open fractures should be covered with a wet, sterile dressing secured by loosely wrapped dry sterile gauze. Check tetanus immunisation; consider antibiotic prophylaxis.
Provide analgesia if required.
Full history, examination and X-rays (see the separate Ankle Injuries article).
Once reduced, stabilise the fracture in a well-fitted backslab cast.
Elevate the limb.
Re-assess neurovascular status to ensure there has been no compromise during the reduction.
Arrange post-reduction X-rays to confirm adequate fracture reduction.
Further management10
Treatment is determined by the stability of the ankle joint. Some fracture patterns are considered stable and may be managed as ankle sprains. All other fracture types may be offered either conservative therapy or surgery, depending on individual circumstances. Surgery usually consists of open reduction and internal fixation, followed by casting or splinting.
Unstable ankle fractures include:
Fracture dislocation.
Bimalleolar or trimalleolar fractures.
Any lateral malleolar fracture with substantial talar shift.
Conservative treatment
Conservative treatment (in a cast) can be considered for:
Non-displaced fractures or anatomically reduced fractures - although functional outcome may be better if treated operatively.
Patients with serious comorbidities who are not fit for surgery.
Conservative treatment comprises:
A well moulded cast for 4-6 weeks - following this, weight-bearing can be resumed.
Serial radiographs to ensure the reduction, joint congruity and healing are maintained (typically repeat radiographs immediately after reduction, at 48 hours, at seven days and then at two-weekly intervals).
Consider operative treatment if the fracture fails to heal or displaces.
Some stable fractures may be more effectively treated in a functional brace than a cast and do not need further X-rays11 .
Operative treatment
Operative treatment involving open reduction and internal fixation is suitable for:
Displaced unstable fractures.
Talar subluxation.
Joint incongruity.
Bimalleolar or trimalleolar fractures - >25-30% involvement of the plafond or >2 mm step off.
Syndesmotic disruption:
Weber C fractures; some Weber B fractures.
Tibiofibular clear space of ≥6 mm on anteroposterior radiography.
The choice between conservative and operative treatment will depend on individual circumstances. Evidence as to which produces the best long-term outcomes is mixed and sometimes contradictory, although a 2012 review concluded that generally unstable fractures fare better with surgical treatment, the decision being based on the degree of distal fibular dislocation and the fracture type10 12 .
Patient factors will also influence the decision, including operative fitness and bone condition. Delayed wound healing and poor bone quality can hinder recovery from open reduction in elderly patients.
Ankle fractures among the elderly population may cause treatment difficulties, with medical co-morbidities, fragile local soft tissues and osteoporosis. Historically, many unstable ankle fractures in elderly patients were treated non-operatively because of high anticipated complications. However, data from recent studies has given weak support in favour of operative intervention in these patients, as some improved outcomes have been demonstrated13 .
Complications14
Back to contentsEarly complications
Soft tissue injury. Only subcutaneous tissue protects the malleoli. Significant wound complications may therefore precede any intervention, particularly where fractures are displaced.
Infection. Particular risk factors for deep infection include:
Increased age.
Diabetes: failed treatment of infection in patients with diabetes who have an ankle fracture can lead to limb loss. Perioperative glycaemic control is very important. Pre-existing peripheral neuropathy and absence of pedal pulses are predictors of worse outcomes.
Smoking.
Open fracture.
Compromised soft tissue envelope.
Alcohol dependency.
Infection in closed ankle injuries may be limb-threatening.
Fracture blisters: these are thought to result from cleavage injury and the dermo-epidermal junction. Anatomical areas with closely adhered skin and little muscle cover are prone to this. there are two types; haemorrhagic blisters and non-haemorrhagic blisters. The former are the more severe injury. there is debate as to whether it is better to allow the blisters to resolve prior to surgical intervention, or to deroof and apply antibiotic cream until they re-epithelialise.
Vascular compromise and foot ischaemia.
Poor wound healing.
Deep vein thrombosis and pulmonary embolism (secondary to immobilisation). The risk is significant if the leg is immobilised without prophylaxis. Risk is increased by high body mass index, pregnancy, contraceptive pill, greater age, active cancer and the need for an above knee plaster. Individualised risk assessments are recommended when considering prophylaxis.
Later complications
Fracture non-union and malunion.
Metalwork failure.
Poor wound healing.
Osteoarthritis (especially talus fractures).
Loss of function: Reduced movement at the ankle (calcaneal fractures can compromise inversion and eversion).
Ankle fractures involving the growth plate in children can lead to deformity and growth disturbance.
Persisting pain.
Muscle atrophy.
Cartilage degeneration.
Joint stiffness and swelling.
Sensory deficit, tarsal tunnel syndrome.
Complex regional pain syndrome type I.
Charcot arthropathy (usually associated with delay in diagnosis and inadequate immobilisation).
Rehabilitation14
Back to contentsPain, stiffness, weakness and swelling are all barriers to overcome for successful rehabilitation. Evidence is sparse regarding rehabilitation after conservative management. There is more evidence available on interventions following surgery.
A combination of early mobilisation, early commencement of weight-bearing and the use of a removable immobilisation device, in conjunction with exercise, has a positive effect on ankle range of motion.
It is important to consider patient factors, particularly their ability to use a temporary immobilisation device and their compliance with exercise regimes.
Immobilisation devices may help reduce pain and encourage participation in the activity but they may also predispose to surgical site complications. Individualised risk-benefit analysis is essential.
A 2015 randomised controlled trial compared a supervised exercise programme with individually tailored advice about self-management (prescribed, monitored and progressed), both delivered by a physiotherapist; it found that they were equally effective15 .
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Ankle Joint Menu; Wheeless' Textbook of Orthopaedics
- Paediatric ankle fractures, Wheeless' Textbook of Orthopaedics
- Rehabilitation after traumatic injury; NICE guideline (January 2022)
- Slimmon D, Brukner P; Sports ankle injuries - assessment and management. Aust Fam Physician. 2010 Jan-Feb;39(1-2):18-22.
- Lynch SA; Assessment of the Injured Ankle in the Athlete. J Athl Train. 2002 Dec;37(4):406-412.
- Tiemstra JD; Update on acute ankle sprains. Am Fam Physician. 2012 Jun 15;85(12):1170-6.
- Venkatadass K, Sangeet G, Prasad VD, et al; Paediatric Ankle Fractures: Guidelines to Management. Indian J Orthop. 2020 Oct 6;55(1):35-46. doi: 10.1007/s43465-020-00270-9. eCollection 2021 Feb.
- Yavas S, Arslan ED, Ozkan S, et al; Accuracy of Ottawa ankle rules for midfoot and ankle injuries. Acta Biomed. 2021 Sep 2;92(4):e2021241. doi: 10.23750/abm.v92i4.9962.
- Jenkin M, Sitler MR, Kelly JD; Clinical usefulness of the Ottawa Ankle Rules for detecting fractures of the ankle and midfoot. J Athl Train. 2010 Sep-Oct;45(5):480-2. doi: 10.4085/1062-6050-45.5.480.
- Bulloch B, Neto G, Plint A, et al; Validation of the Ottawa Knee Rule in children: a multicenter study. Ann Emerg Med. 2003 Jul;42(1):48-55.
- Mordecai S, Al-Hadithy N; Management of ankle fractures. BMJ. 2011 Oct 28;343:d5204. doi: 10.1136/bmj.d5204.
- Goost H, Wimmer MD, Barg A, et al; Fractures of the ankle joint: investigation and treatment options. Dtsch Arztebl Int. 2014 May 23;111(21):377-88. doi: 10.3238/arztebl.2014.0377.
- Donken CC, Al-Khateeb H, Verhofstad MH, et al; Surgical versus conservative interventions for treating ankle fractures in adults. Cochrane Database Syst Rev. 2012 Aug 15;8:CD008470. doi: 10.1002/14651858.CD008470.pub2.
- Jain N, Symes T, Doorgakant A, et al; Clinical audit of the management of stable ankle fractures. Ann R Coll Surg Engl. 2008 Sep;90(6):483-7.
- Van Schie-Van der Weert EM, Van Lieshout EM, De Vries MR, et al; Determinants of outcome in operatively and non-operatively treated Weber-B ankle fractures. Arch Orthop Trauma Surg. 2012 Feb;132(2):257-63. doi: 10.1007/s00402-011-1397-z. Epub 2011 Sep 30.
- Dhillon MS, Rajnish RK, Patel S, et al; Osteoporotic ankle fractures: A narrative review of management options. J Clin Orthop Trauma. 2020 May-Jun;11(3):380-387. doi: 10.1016/j.jcot.2019.10.010. Epub 2019 Nov 4.
- Mehta SS, Rees K, Cutler L, et al; Understanding risks and complications in the management of ankle fractures. Indian J Orthop. 2014 Sep;48(5):445-52. doi: 10.4103/0019-5413.139829.
- Moseley AM, Beckenkamp PR, Haas M, et al; Rehabilitation After Immobilization for Ankle Fracture: The EXACT Randomized Clinical Trial. JAMA. 2015 Oct 6;314(13):1376-85. doi: 10.1001/jama.2015.12180.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 14 Feb 2027
15 Feb 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free