Refraction and refractive errors
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 17 Jan 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Hypermetropia article more useful, or one of our other health articles.
In this article:
Continue reading below
What is refraction?
The purpose of the globe of the eye is to receive light from the outside world and transmit it to the brain for processing into a visual image. There are two essential elements to this function: the image has to be correctly focused on to the back of the eye and this information has to be converted to electrochemical signals and transmitted to the brain.
In optical physics, the term 'refraction' describes the bending of light rays at the interface between two different transparent media. Refraction is measured in dioptres (D) which describes the power that a structure has to focus parallel rays of light (ie bring them to a point) The higher this value, the stronger the focusing ability.
In the eye, refraction happens mainly at the surface of the cornea and at the surface of the lens. Refraction at the front surface of the cornea accounts for about 80%, with the lens being responsible for most of the rest. The air-tear interface, aqueous and vitreous humours also make a small contribution. The lens is, however, the total source of accommodation (focus on near objects) and can change the focal length of the eye by 7-8%.
For good vision the point of focus must be on the retina. This accuracy of refraction depends on:
The curvature of the cornea and lens.
The axial length of the eye (from front to back).
These change as the eye grows and ages. Refractive development is influenced both by environmental factors and by genetic factors.1
Importance of refractive errors2
Uncorrected refractive error accounts for half of avoidable vision impairment globally and nearly a third of avoidable total loss of vision. Globally, 153 million people have visual impairment or total loss of vision due to uncorrected refractive error, most in low-income countries.
Minor reduction in vision (<6/12) has been associated with an increased risk of death and physical, social and psychological problems in people older than 50 years.
Undetected refractive errors in childhood may lead to behavioural problems and adversely affect social interaction and performance at school.
Under-corrected refractive error may account for up to 75% of all vision impairment in high-income countries.
The global problem of refractive error
Global estimates indicate that more than 2.3 billion people in the world experience poor vision due to refractive error and that 13 million children aged 5-15 years worldwide are visually impaired from uncorrected refractive error. Visual impairment from uncorrected refractive errors can have immediate and long-term consequences in children and adults, such as lost educational and employment opportunities, lost economic gain for individuals, families and societies and impaired quality of life.
School vision screening programmes carried out by teachers and other ancillary personnel can identify and treat or refer children with refractive error. The potential impact varies widely between areas, depending on prevalence of refractive error and rates of school attendance. Barriers to acceptance of services include cost and quality of refractive care and cultural beliefs that glasses will harm children's eyes.3 4
Refractive errors5
Back to contentsAmetropia is a global term for any refractive error.
Myopia6
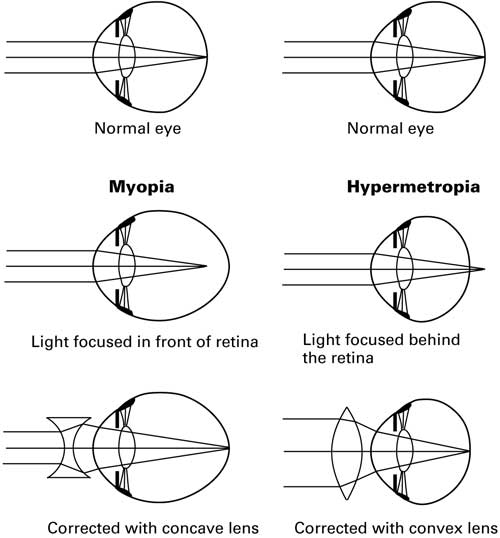
Myopic eyes have excessive optical power for the axial length of the eyeball and so focus the image in front of the retina. This arises as a result of physiological variation in the length of the eye or of an excessively curved cornea. This common condition affects about 1 in 4 adults in the UK and tends to manifest itself in adolescence or early adulthood.2 It is classified as mild (up to 3.0 D), moderate (3.0-6.0 D) or severe/high-degree (>6.0 D). The latter affects about 200,000 British people.
Complications: high myopia can be associated with degenerative fundal changes (Förster-Fuchs spots). High myopia is associated with an increased risk of retinal detachment, cataract formation and glaucoma.7
Patient perspective: patients are said to be near-sighted - distant objects appear to be blurred but, unless severe, close-up objects are in focus. There may be a family history of myopia and there is some evidence to suggest that children who do a lot of close-up work are more likely to become myopic (or to worsen pre-existing myopia). Other associations include:
Prematurity.
Marfan's syndrome.
Stickler's syndrome.
Ehlers-Danlos syndrome.
Homocystinuria.
Lens correction: a concave (minus) lens is used to correct the problem (see diagram and explanation below).
Refraction
Hypermetropia (hyperopia)
The eye has insufficient optical power for its refractive length and therefore light from an object is focused behind the retina, so giving rise to a blurred image. Mild hypermetropia is a common finding in babies and very young children and this usually resolves by about 3 years of age.2
Complications: persistent hypermetropia is associated with an increased risk of glaucoma, squint and amblyopia.
Patient perspective: patients are said to be long-sighted - distant objects are sharply focused but there is difficulty in viewing near objects, which may give rise to eye strain (due to the extra accommodative effort) and headache. There may be a family history but most cases are sporadic. Other eye conditions associated with hypermetropia include:
Corneal dystrophies.
Congenital cataracts.
Retinitis pigmentosa.
Microphthalmia.
Lens correction: a convex (plus) lens is used to correct the problem (see diagram and explanation above).
Astigmatism8
Light from a point in the visual field has to focus at a single point on the retina. This is achieved through the symmetry of the corneal and lens curvatures around their circumference. In astigmatism, variations in the symmetry of these curvatures (usually corneal) result in rays failing to focus on a single point. The degree of astigmatism is measured in cylinders (cyl).
Astigmatism is often present in association with some degree of myopia or hypermetropia. A mild degree of astigmatism is relatively common in childhood and resolves in a number of cases. More severe astigmatism may lead to amblyopia, especially if there is an associated squint.
Patient perspective: there is blurring of vision that is not necessarily associated with obvious far-/short-sightedness, although distant viewing is usually the more problematic of the two. The brain will try to compensate for distortion but optical symptoms may include:
Blurry, distorted, or fuzzy vision.
Difficulty seeing at night.
Eyestrain.
Squinting.
Eye irritation.
Headaches.
Most cases are sporadic but there may be a family history or a background of:
Previous eye surgery.
Previous corneal injury.
Corneal dystrophies.
Congenital cataract.
Optic nerve hypoplasia.
Retinitis pigmentosa.
Albinism.
Nystagmus.
Lens correction: a cylindrical lens is used to 'neutralise' astigmatism. The axis of the cylinder depends on the meridian of asymmetry in the patient's cornea. Where there is associated myopia or hypermetropia, a spherocylindrical lens is used.
Anisometropia9
This refers to the situation where there are unequal refractive errors between both eyes. This may be mild with limited consequences (eg, different degrees of myopia in each eye) - a relatively common situation. Where there are large differences (a ≥2.0 D difference) in childhood, particularly if one eye is myopic and the other hypermetropic, there may be associated amblyopia.
Anisometropia is more unusual in adulthood but can occur following trauma or refractive or cataract surgery. The most extreme form occurs where there is unilateral aphakia (one lens is missing or has been removed).
Patient perspective: differing refractive states result in slight differences in image size (aniseikonia). Where the refractive difference is very small, this is not perceived by the patient and does not cause difficulty. Where there is a large refractive difference, the patient may experience diplopia, headaches, photophobia, reading difficulties, nausea, dizziness and general fatigue.10 In childhood the brain is more likely simply to suppress one of the images, so that amblyopia develops in the eye in which image has been suppressed.
Lens correction:10 this is difficult and usually involves various types of spherical and cylindrical lenses, depending on the type of anisometropia. However, the prismatic effects of the lenses typically vary in different positions of gaze, giving rise to further symptoms (collectively known as anisophoria, which is a lens-induced aniseikonia). Many patients tolerate the lenses even less well than the original problem. Contact lenses often offer a better solution. The management of these patients remains within the remit of specialist optometrists.
Presbyopia11
Accommodation is the process by which the eye adjusts its optical power to maintain a clear image of an object as its distance varies. There are three elements to it: the eyes converge, pupil size reduces and the crystalline lens changes shape and position.
Presbyopia is the gradual loss of the accommodative response due to a decline in the elasticity of the lens. It is a lifelong process which only becomes clinically significant when the residual accommodative amplitude is insufficient for the patient to carry out near-vision tasks such as reading. These symptoms most commonly occur after the age of 40 years (this varies depending on pre-existing refractive error, pupil size and the patient's usual visual tasks). There are an estimated 517 million cases of people with uncorrected presbyopia worldwide, 410 million of whom are likely to be restricted in doing basic tasks.
Patient perspective: the patient finds it difficult to carry out near tasks and may need brighter lighting conditions for these or need reading glasses. They may also complain of an accommodative lag (a slowed recovery time changing from distance to near tasks and vice versa). Individuals may also report tiring with continuous close work.
Correction: if there is no pre-existing eye problem or refractive error, patients may manage well with over-the-counter glasses. They should be advised to take the glasses off when not carrying out near tasks. However, if there is a pre-existing refractive error, prescription glasses are generally required; these may be bifocals or trifocals. Contact lenses may also be used. Surgical correction is possible, although there is a small risk of complications.12
Accommodative insufficiency13
This is in effect a premature form of presbyopia which is probably neuronal in origin. It is associated with a number of neurological conditions, such as encephalitis and closed head trauma. It is also seen in patients with current or past debilitating illness and it may be induced by certain medications (eg, parasympatholytics and tranquilising drugs). It is characterised by an inability to maintain binocular alignment as an object comes nearer to a patient. This condition is relatively common (3-5% of the population) and particularly affects individuals who have high visual demands (a lot of close work such as teenagers, college students and others studying), in periods of illness, anxiety or fatigue.
Patient perspective: initially, patients may complain of asthenopia (a vague discomfort associated with using the eyes, also referred to as 'eye strain', eye or brow ache). This occurs particularly when trying to accommodate. Ultimately, near vision becomes blurred or there is diplopia associated with bringing objects closer. Symptoms vary from mild to severe but are few or absent in distant vision.
Correction: treatment is with corrective lenses or exercises for the eyes involving the near point of convergence. Occasionally there is a role for pharmacological agents.
Accommodative excess
This arises as a result of ciliary muscle spasm. This may arise from ocular disease (eg, iridocyclitis), or from drugs used to treat ocular disease (eg, anticholinesterases used in the treatment of glaucoma) or it may arise due to uncorrected refractive errors (usually hypermetropia). It can also occur after prolonged periods of close work.
Patient perspective: symptoms characteristically include headache, brow ache, variable blurring of distance vision and an unusually close near point.
Correction: lenses and eye exercises are prescribed. Occasionally, the patient may need pharmaceutical treatment (eg, cycloplegics).
Continue reading below
Assessing refractive errors
Back to contentsAlthough the diagnosis of a refractive error can only accurately be made when the patient is refracted (see 'Refraction', below), you can get a sense of whether this might actually be a problem of refractive error.
Presentation2
Symptoms tend to relate to activities of daily living and may include difficulty with driving, reading (particularly small print such as bills or medication instructions) and preparing meals. Symptoms may be so gradual that altered vision may not be noticed and patients may instead complain of headaches or red, sore, watery eyes. Young children may rub their eyes a lot or turn their heads when looking at things. School-aged children may present with behavioural problems.
Associated conditions
Other ocular or systemic conditions may be associated with refractive error (see list of associations, above).
Prescription interpretation
The prescription tells you how strong a lens is needed to bring the eye back to emmetropia. The larger the numbers, the stronger the lens required. The format of the prescription is:
[figure indicating degree of myopia/hypermetropia]/[figure telling you how astigmatic they are] x [meridian in which astigmatism lies]
So, for example, a patient with a prescription of -1.25/-1.00 x 180 has a refractive error requiring a 1.25 D lens to correct the myopic element and a 1.00 D lens to correct the astigmatic element (at 180° which tells the optometrist in which plane the astigmatism lies).
If the prescription was 0.00/-2.00 x 180, the patient has some astigmatism but no myopia or hypermetropia.
Assessment process
Test each eye separately for near and distance vision. See the separate Examination of the Eye article. Patients should use their usual distance glasses or be tested with their contact lenses in, as you are looking for deterioration beyond that already diagnosed/treated. Test again using a pinhole: if they do better, an uncorrected refractive error may be present.
Referral
Depending on the nature of the presentation, you may wish to refer to your local eye unit (acute presentation or presence of other symptoms) or, if for a long-standing problem, recommend an optometrist assessment. Consider:
Semi-urgent referral in anyone unexpectedly scoring 6/60 or worse.
Non-urgent referral where:
Children managing 6/9 or worse or adults managing 6/12 or worse.
There is a two-line difference in visual acuity between the eyes.
You see or suspect strabismus. See the separate Eye Problems in Babies article.
There is difficulty in achieving a reliable visual acuity measurement
Non-urgent referral where the near acuity is less than N5.
Young children should be referred to an ophthalmologist or optometrist able to provide special paediatric care.
Refraction
Assessment of a refractive error can only really be done via the process of refraction (generally carried out by an optometrist). In clinical ophthalmology, 'refraction' is an abbreviation for 'refractive correction' and it refers to the process by which the best possible visual acuity can be obtained for a patient. Refraction has three objectives:
Measure the patient's refractive error.
Determine the optical correction required for focusing on distant and close objects.
Provide appropriate corrective spectacles/lenses.
Refraction has several components:
Objective refraction: this uses an instrument (retinoscope) devised to determine the approximate nature of the patient's refractive error (eg, myopia, astigmatism). It does not require any input from the patient.
Subjective refraction: this uses a series of lenses to refine the measurement of the refractive error. It requires active patient participation and therefore is difficult to perform in patients with limited communication (eg, pre-verbal children).
Binocular balancing: this final step ensures that accommodation and distant viewing are balanced in both eyes.
Treatment and management of refractive errors
Back to contentsThese may be managed by optometrists (specialists in the diagnosis and management of refractive errors), orthoptists (specialists in ocular motility problems and assessment of refractive errors in very young children) or ophthalmologists (medically qualified physicians or surgeons).2
Lenses
Spectacles are the simplest, safest and most cost-effective way or managing refractive errors.2 Lenses may be spherical, cylindrical or a mixture of both.
Spherical lenses have a constant curvature over the entire surface and may be convex (converge light rays, known as plus lenses) or concave (diverge light rays, known as minus lenses).
Cylindrical lenses have focusing powers in one meridian only, the orientation of which depends on the patient's problem.
The power of a spectacle lens can be measured using an instrument known as a lensmeter. Multifocal lenses have more than one refractive component. The power needed for each component can be assessed and prescribed separately.
Contact lenses
Contact lenses work on the same principle as spectacle lenses. Only the tear film separates them from the cornea.
Orthokeratology is an emerging technique of using night-time contact lenses to correct daytime vision: a rigid gas permeable lens is worn at night to distort the corneal shape in a controlled fashion, so reducing symptoms of myopia during the day. See the separate Contact Lenses (Types and Care) and Contact Lens Problems articles.
Surgical correction14
This may entail microsurgery (such as lens implants) or laser treatment to the cornea.
Photorefractive (laser) surgery for the correction of refractive errors is well established and considered safe and effective for use in appropriately selected patients.15 16
Several types of laser surgery have been developed. These include LASIK®, PRK® and LASEK®. They are all similar, typically taking about ten minutes per eye and aiming to reshape the cornea by using the laser to remove a very thin layer of corneal tissue. The reshaping of the cornea allows the refraction of the eye to be corrected.16 17 18
LASIK®
LASIK stands for Laser-Assisted In situ Keratomileusis. This is the most popular form of laser eye surgery.
The laser is used to lift and remove a thin flap of the corneal epithelium.
The laser is used to alter the curvature of the cornea so that the refractive error is corrected.
The flap is then replaced and sticks spontaneously to the underlying corneal stroma. The flap serves as a natural bandage, keeping the eye comfortable as it heals. Healing occurs relatively quickly.
This is the most popular and common type of laser eye surgery.
Vision recovery time is said to be around 24 hours.
An analysis of literature on LASIK® for refractive error showed high rates of patient satisfaction (>95%).17 They concluded that LASIK surgery should be considered among the most successful elective procedures.
For people who are not suitable for LASIK® the following two options are sometimes offered.
PRK®
PRK stands for Photo-Refractive Keratectomy.
During PRK®, instead of creating a corneal flap as in LASIK, the surgeon completely removes the extremely thin outer layer of the cornea using an alcohol solution and a 'buffing' device or a blunt surgical instrument. The underlying cornea is then reshaped with a laser. A new epithelial layer grows back within five days.
The healing time in PRK® is faster than in LASEK®, below.
LASEK®
LASEK stands for LAser Sub-Epithelial Keratomileusis.
The LASEK® procedure involves taking a thinner flap of corneal epithelium than in LASIK®. The cornea underneath is then treated as in LASIK® and the thinner flap repositioned and held in place with a bandage contact lens.
The hinged flap made in LASEK® surgery is much thinner than the corneal flap created in LASIK® (which contains both epithelial and deeper stromal tissues).
The LASEK® technique lessens the likelihood of removing too much cornea. There also is slightly less risk of developing dry eyes afterwards.
Patients with a naturally thin cornea may be more suited to this treatment.
LASEK® can be a better option for patients with a high degree of myopia, which requires more tissue removal from the central cornea.
LASEK® tends to be more painful and discomfort can last longer than with LASIK®. Visual recovery time can be up to a week.
In some cases, the thin flap created during LASEK® is not strong enough to be replaced and will be removed completely as it would have been in PRK.
The alcohol solution used during LASEK® can irritate and slow the healing process immediately after surgery.
Side-effects of all laser surgery may include blurred vision, over-correction or under-correction of short-sight, eye infection and dry eyes.
Intraocular lens (IOL) implants
Occasionally, the best option for correction of severe refractive error is IOL insertion or replacement. The procedure is carried out with the patient under local anaesthesia. The pupil is dilated using topical medication; a phakic IOL is inserted into the anterior or the posterior eye chamber via a small corneal incision. Depending on its design, the phakic IOL is anchored to the iris, placed in the angle between the cornea and the iris, or positioned to float over the surface of the natural lens.
The National Institute for Health and Care Excellence (NICE) concluded that here is good evidence of short-term safety and efficacy. However, there is an increased risk of cataract, corneal damage or retinal detachment and there are no long-term data about this. Therefore, the procedure may be used with normal arrangements for clinical governance and audit but with special arrangements for consent.19
Clinicians wishing to undertake IOL insertion for correction of refractive error, with preservation of the natural lens, should ensure that patients understand the risks of having an artificial lens implanted for visual impairment that might otherwise be corrected using spectacles or contact lenses.
Refractive lens exchange (RLE)
Patients with high degrees of myopia, hyperopia and astigmatism are not good candidates for laser surgery. Presbyopia can usually only be corrected with monovision or reading spectacles. RLE with multifocal or accommodating intraocular lenses in combination with corneal astigmatic procedures can potentially address all refractive errors, and eliminate the future need for cataract surgery.
This is an invasive procedure to counter a problem which might be solved with reading glasses. However, where refractive error is severe (particularly where there are co-existing cataracts) and where patients wish to improve distance and near vision without the use of varifocal spectacles (or where there is co-existing cataract) this may offer a solution.20 21
Kamra® corneal inlay
This is a different approach to presbyopia. The Kamra® corneal inlay was approved in 2015. The inlay is designed to eliminate the need for reading glasses among people between the ages of 45 and 60 years who have good distance vision without glasses but have problems seeing up close due to presbyopia.
The inlay is a small, thin, opaque device with a tiny opening in the centre. It is surgically implanted in the central cornea, directly in front of the pupil of the eye. The central opening in the inlay creates a 'pinhole camera' effect. This effect, also seen if you look through a pinhole in a piece of paper, sharpens near vision while maintaining clear distance vision.
The inlay typically is implanted in the non-dominant eye. This allows both eyes to be used for distance vision, while the inlay sharpens near vision in the non-dominant eye.The procedure takes around 15 minutes and can be performed in the treatment room. No stitches are needed. Healing time may vary but most people are able to resume their normal activities within 24 to 48 hours.22
Monocular surgery for presbyopia23 24
Surgical treatment for presbyopia uses a slightly different approach to traditional laser surgery. Adjustments to the corneal curvature sufficient to compensate for the loss of lens accommodation are likely to reduce distant vision, as the adaptability of focus has been lost. Therefore, many approaches to presbyopia use a monovisual approach, whereby the less dominant eye is corrected for near vision at the expense of some loss of binocular distant vision.25
Monovision LASIK®
LASIK® stands for Laser-Assisted In situ Keratomileusis. This is the most popular form of laser eye surgery and is a means of altering the refractive power of the cornea. In monovision LASIK® for presbyopia this is essentially done for one eye only:
The laser is used to lift and remove a thin flap of the cornea.
This helps to flatten the cornea so that the light rays can be focused further back and on to the retina.
The flap is then replaced and sticks spontaneously to the underlying cornea. The flap serves as a natural bandage, keeping the eye comfortable as it heals. Healing occurs relatively quickly.
This is the most popular and common type of laser eye surgery.
Vision recovery time is said to be around 24 hours.
The LASIK® surgeon fully corrects the distance vision of one eye (usually the dominant eye) and intentionally makes the non-dominant eye mildly nearsighted. The newly nearsighted eye sees near objects clearly without glasses, although its distant vision may be less good. So, after monovision LASIK®, the dominant eye takes the lead to provide clear distance vision and the non-dominant eye is responsible for sharpening near vision. If additional distance vision clarity is desired for specific activities after monovision LASIK®, special-purpose eyeglasses or contact lenses can be prescribed that optimise distance vision.
Monovision conductive keratoplasty (CK)
CK uses low-level, radiofrequency energy to shrink fibres in the edge of the cornea to increase the curve and therefore increase its focusing power. Like monovision LASIK®, one eye is corrected for close vision and the other left for distance vision.
Monovision of any kind, whether it's monovision LASIK® or monovision with contact lenses, involves some compromise and not everyone adapts well to it. It's a good idea to try monovision with contact lenses before committing to a permanent surgical procedure, in case you are one of the small minority who don't adapt to it.
IntraCor®
The IntraCor® procedure uses a laser to create precisely placed gas bubbles, which then reshape the interior of the cornea without penetrating the outer surface. This means less chance of infection, inflammation or other complications. There is significant improvement in near vision, as long as ample light is provided. The technology is approved in Europe for presbyopia correction in people with farsightedness.26
Refractive lens exchange (RLE)
RLE is the replacement of the eye's natural lens with an artificial IOL. The procedure is very similar to cataract surgery. It can reduce the need for reading glasses and can restore significant near vision while providing clear distance vision without glasses.20
Multifocal LASIK® (PresbyLASIK®)
Clinical trials investigating the effectiveness and safety of this procedure are being conducted. This applies the principle of multifocal lenses to eye surgery. Different zones are created on the cornea so that it mimics multifocal reading glasses.27
Other corneal inlays and procedures
Raindrop® Near Vision Inlay is a presbyopia-correcting inlay which looks like a tiny contact lens that is implanted in the cornea under a flap made with a femtosecond laser. It is made of a proprietary hydrogel material.27
Presbia Flexivue Microlens® is a tiny customised lens inserted in a self-sealing pocket created in the cornea of the non-dominant eye, using a femtosecond laser. A clinical trial in the USA commenced in 2014 and results are expected in 2017.
Prevention
There has been evidence to suggest that early outdoor activity may reduce the risk of children developing myopia in later life. Myopia may also be slowed with orthokeratology. See separate Contact Lenses (Types and Care) article.
Continue reading below
Screening
Back to contentsSee also the separate Vision Testing and Screening in Young Children article. There are no robust trials available that allow the benefits of school vision screening to be measured.
Asymptomatic, low-risk patients (no ocular comorbidity or family history) should have regular eye examinations. Patients at increased risk of visual impairment (eg, patients with diabetes, those with cataracts, macular degeneration, glaucoma or a significant family history of these) should have frequent eye examinations. The frequency of eye examinations will depend on a person's age and their medical and ophthalmic history.
Globally there is a place for school vision screening. There is limited provision of spectacles or optical corrections among most of the adults and children with refractive error around the world. School vision screening programmes can identify and treat or refer children with refractive error.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Wojciechowski R; Nature and nurture: the complex genetics of myopia and refractive error. Clin Genet. 2011 Apr;79(4):301-20. doi: 10.1111/j.1399-0004.2010.01592.x. Epub 2010 Dec 13.
- Cochrane GM, du Toit R, Le Mesurier RT; Management of refractive errors. BMJ. 2010 Apr 12;340:c1711. doi: 10.1136/bmj.c1711.
- Naidoo KS, Leasher J, Bourne RR, et al; Global Vision Impairment and Blindness Due to Uncorrected Refractive Error, 1990-2010. Optom Vis Sci. 2016 Mar;93(3):227-34. doi: 10.1097/OPX.0000000000000796.
- Sharma A, Congdon N, Patel M, et al; School-based approaches to the correction of refractive error in children. Surv Ophthalmol. 2012 May-Jun;57(3):272-83. doi: 10.1016/j.survophthal.2011.11.002. Epub 2012 Mar 6.
- Schiefer U, Kraus C, Baumbach P, et al; Refractive errors. Dtsch Arztebl Int. 2016 Oct 14;113(41):693-702. doi: 10.3238/arztebl.2016.0693.
- Cooper J, Tkatchenko AV; A Review of Current Concepts of the Etiology and Treatment of Myopia. Eye Contact Lens. 2018 Jul;44(4):231-247. doi: 10.1097/ICL.0000000000000499.
- Gwiazda J; Treatment options for myopia. Optom Vis Sci. 2009 Jun;86(6):624-8. doi: 10.1097/OPX.0b013e3181a6a225.
- Read SA, Collins MJ, Carney LG; A review of astigmatism and its possible genesis. Clin Exp Optom. 2007 Jan;90(1):5-19. doi: 10.1111/j.1444-0938.2007.00112.x.
- Barrett BT, Bradley A, Candy TR; The relationship between anisometropia and amblyopia. Prog Retin Eye Res. 2013 Sep;36:120-58. doi: 10.1016/j.preteyeres.2013.05.001. Epub 2013 Jun 15.
- About Aniseikonia; Optical Diagnostics
- Katz JA, Karpecki PM, Dorca A, et al; Presbyopia - A Review of Current Treatment Options and Emerging Therapies. Clin Ophthalmol. 2021 May 24;15:2167-2178. doi: 10.2147/OPTH.S259011. eCollection 2021.
- Care of the Patient with Accommodative and Vergence Dysfunction; American Optometric Association - last updated 2010
- Hussaindeen JR, Murali A; Accommodative Insufficiency: Prevalence, Impact and Treatment Options. Clin Optom (Auckl). 2020 Sep 11;12:135-149. doi: 10.2147/OPTO.S224216. eCollection 2020.
- Ang M, Gatinel D, Reinstein DZ, et al; Refractive surgery beyond 2020. Eye (Lond). 2021 Feb;35(2):362-382. doi: 10.1038/s41433-020-1096-5. Epub 2020 Jul 24.
- Photorefractive (laser) surgery for the correction of refractive error; NICE Interventional procedures guidance, March 2006
- Laser correction of refractive error following non-refractive ophthalmic surgery; NICE Interventional procedures guidance, March 2011
- Solomon KD, Fernandez de Castro LE, Sandoval HP, et al; LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009 Apr;116(4):691-701. doi: 10.1016/j.ophtha.2008.12.037.
- Professional Standards for Refractive Surgery; Royal College of Ophthalmologists (Dec 2021)
- Intraocular lens insertion for correction of refractive error, with preservation of the natural lens; Interventional procedures guidance, February 2009
- Alio JL, Grzybowski A, El Aswad A, et al; Refractive lens exchange. Surv Ophthalmol. 2014 Nov-Dec;59(6):579-98. doi: 10.1016/j.survophthal.2014.04.004. Epub 2014 May 9.
- Alio JL, Grzybowski A, Romaniuk D; Refractive lens exchange in modern practice: when and when not to do it? Eye Vis (Lond). 2014 Dec 10;1:10. doi: 10.1186/s40662-014-0010-2. eCollection 2014.
- Naroo SA, Bilkhu PS; Clinical utility of the KAMRA corneal inlay. Clin Ophthalmol. 2016 May 18;10:913-9. doi: 10.2147/OPTH.S89132. eCollection 2016.
- Davidson RS, Dhaliwal D, Hamilton DR, et al; Surgical correction of presbyopia. J Cataract Refract Surg. 2016 Jun;42(6):920-30. doi: 10.1016/j.jcrs.2016.05.003.
- Torricelli AA, Junior JB, Santhiago MR, et al; Surgical management of presbyopia. Clin Ophthalmol. 2012;6:1459-66. doi: 10.2147/OPTH.S35533. Epub 2012 Sep 6.
- Glasser A; Restoration of accommodation: surgical options for correction of presbyopia. Clin Exp Optom. 2008 May;91(3):279-95. doi: 10.1111/j.1444-0938.2008.00260.x.
- Thomas BC, Fitting A, Auffarth GU, et al; Femtosecond laser correction of presbyopia (INTRACOR) in emmetropes using a modified pattern. J Refract Surg. 2012 Dec;28(12):872-8. doi: 10.3928/1081597X-20121115-03.
- Arlt E, Krall E, Moussa S, et al; Implantable inlay devices for presbyopia: the evidence to date. Clin Ophthalmol. 2015 Jan 14;9:129-37. doi: 10.2147/OPTH.S57056. eCollection 2015.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Jan 2028
17 Jan 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free