Hysterosalpingography
Peer reviewed by Dr Rosalyn Adleman, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 9 Sept 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Hysterosalpingography (HSG) is a particular type of imaging of the uterus (womb) and the Fallopian tubes. It uses a dye to be able to visualise the size and shape of the uterus and check whether the Fallopian tubes are blocked.
In this article:
Continue reading below
What is hysterosalpingography?
Hysterosalpingography (also known as HSG) is an X-ray test using dye which can help to investigate problems related to infertility. For example, it may help to detect whether the Fallopian tubes are open. Blockage in the tubes can prevent the sperm and egg from combining together to produce an embryo.
Why is hysterosalpingography done?
Back to contentsHSG is usually performed in women who are having difficulty becoming pregnant. This test allows the doctor to assess the shape and structure of the uterus (womb) and any scarring in the region. It also allows the doctor to check that the Fallopian tubes are not blocked.
The procedure may also be used to investigate repeated miscarriages, as these may result from problems with the uterus.
HSG can also help to see whether there are other problems in the pelvis or uterus including:
Polyps (benign fleshy lumps) in the womb.
An abnormal passage between two places that do not normally connect. This is called a fistula.
Areas where the walls of the uterus are sticking together (adhesions).
Non-cancerous growths in the wall of the uterus (uterine fibroids).
HSG is also used to check the Fallopian tubes are not blocked and to monitor the effects of surgery on the Fallopian tubes. This may include checking for:
Blockage of the Fallopian tubes due to infection or scarring.
The re-opening of the Fallopian tubes following surgery for a blockage.
Continue reading below
How does hysterosalpingography work?
Back to contentsNormally, soft, hollow structures such as the womb cannot be seen on x-ray images. In HSG a dye that blocks x-rays is inserted into the womb (uterus) and ovarian tubes. This dye is called a contrast agent and appears black on the x-ray image.
The person performing the test will be able to look at the pictures on a television screen. They can watch as the contrast agent fills the uterus and Fallopian tubes. They can then observe any problems or defects. In a normal hysterosalpingogram the contrast fills the uterus, enters the uterine tubes and spills out of the ends of these tubes into the body cavity.
In the image below, the small black triangle shape in the middle is a normal womb filled with dye. The dye comes in through the tube which is at the base of the triangle and goes out to the edge of the photo. There are two very thin lines of dye coming away from the points of the triangle and these are normal Fallopian tubes, filled with dye. The larger areas of dye at either side is where the dye has spilled out of the normal tubes.
Hysterosalpingogram
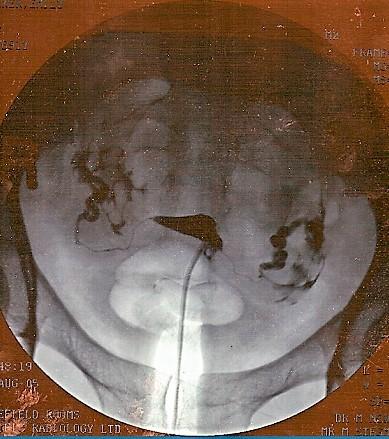
By jemsweb [CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0)], via Wikimedia Commons
What happens during hysterosalpingography?
Back to contentsProcedures may vary slightly in different hospitals, so this explanation is written as a guide. Any specific instructions or advice from a particular hospital should be read clearly.
In some departments you may be given a tablet or injection to help you relax before the procedure takes place. This will not put you to sleep but may make you feel more relaxed. This is rarely used.
You will be asked to lie on the X-ray table. Then you may be asked to slide down to the end of the table, with your knees bent. The position is similar to the one you are in when you have a smear (cervical screening test) taken.
Your pubic area will be cleaned. A speculum will be inserted into your vagina. This is the same instrument used in a smear. This allows the doctor or nurse to see the neck of your womb (cervix).
You may be given a local anaesthetic injection to your cervix, although this is not usually needed. The doctor or nurse will then place a thin tube through your cervix into your womb (uterus). This is often uncomfortable and can cause period-type pain.
Then the contrast agent will be gently syringed through the catheter, gradually filling your uterus and Fallopian tubes. You may feel some pressure and possibly some crampy type pains.
As the contrast enters your uterus the doctor will start taking the images using the fluoroscope. After the fluoroscopic images have been taken you may be asked to remain still for a final X-ray. Then the catheter and speculum will be removed. You will also be given a sanitary towel to absorb the contrast agent.
How long does a hysterosalpingogram take?
The procedure usually takes between 15 and 30 minutes.
Continue reading below
How to prepare for hysterosalpingography
Back to contentsYour local hospital should give you information about how to prepare before the test.
Women who are pregnant should not have hysterosalpingography. This is because the X-rays may damage the unborn child. You should inform your doctor if you are, or think you may be, pregnant. For this reason, some hospitals may ask you to take a pregnancy test before the procedure. Or, the procedure may be done soon after a period to minimise the chance that you may be pregnant.
There are a few instances when an HSG cannot be done. For example, it would not be done:
During a period.
If there is any possibility of pregnancy.
If there are symptoms of pelvic infection such as a high temperature with abdominal pain and vaginal discharge.
What to expect after hysterosalpingography
Back to contentsContrast agent that remains in the uterus will gradually leak out through the vagina. Any other contrast left in the pelvis will be absorbed safely by the body. Only a small amount of contrast is used during the examination and it has no odour or colour.
Some cramping may be experienced following the examination along with some minor 'spotting' (light bleeding). Both should settle in a couple of days. Sanitary towels are best to use, rather than tampons, if needed.
Low-dose X-rays are used so the total amount of radiation for the whole test is quite small and relatively safe. The radiation exposure during this examination, like the radiation produced during any other X-ray test, passes through immediately. It is not necessary to take any precautions following this procedure.
What are the side-effects of hysterosalpingography?
Back to contentsMost women experience only minor side-effects. These may include:
Sticky vaginal discharge as some of the fluid drains out of the womb.
Crampy pains.
Feeling dizzy, faint, or sick.
Slight vaginal bleeding.
Serious problems are rare. They may include an allergic reaction to the fluid, injury to the womb (uterus), or pelvic infection. Medical attention should be sought (ideally from the clinic who did the HSG) if any of these symptoms are experienced after the procedure:
Being sick (vomiting).
Fainting.
Severe abdominal pain or cramping.
Heavy vaginal bleeding.
High temperature (fever) or chills.
Note: a normal HSG does not prove that there is no underlying problem in the uterus or Fallopian tubes. Further tests may be needed - for example, a laparoscopy. The doctor who requested the HSG test will be able to explain the results in detail.
Does a hysterosalpingogram increase the chance of pregnancy?
Back to contentsA hysterosalpingogram is a test for assessing any structural problems rather than a treatment for infertility.
However, studies suggest that the chances of pregnancy increase by up to 30% in the 3 months after an HSG. This is thought to be because the HSG dye may have dislodged potential obstructions within the Fallopian tubes. The effects of this don't wear off after 3 months but it is thought that, where those small obstructions were the only barrier to conceiving, removing them allows women to fall pregnant relatively quickly.
It does not open up blockages of the Fallopian tubes caused by previous infections, most commonly chlamydia.
Anatomy and function of the female reproductive system
Back to contentsFemale reproductive organs
It is thought that a structural problem with the uterus, Fallopian tubes and cervix is a cause of infertility in about 13 out of 100 couples who are struggling to conceive.
Video picks for Imaging
Patient picks for Imaging

Tests and investigations
Radionuclide scan
A radionuclide scan is a way of imaging bones, organs and other parts of the body by using a small dose of a radioactive chemical. There are different types of radionuclide chemical. The one used depends on which organ or part of the body is to be scanned. Note: the information below is a general guide only. The arrangements, and the way tests are performed, may vary between different hospitals. Always follow the instructions given by your doctor or local hospital.
by Dr Rachel Hudson, MRCGP

Tests and investigations
PET scan
A PET scan create images which show where cells are particularly active in the body. It is most commonly used to diagnose and assess cancer. Note: the information below is a general guide only. The arrangements, and the way tests are performed, may vary between different hospitals. Always follow the instructions given by your doctor or local hospital.
by Dr Rosalyn Adleman, MRCGP
Further reading and references
- Fertility - Assessment and treatment for people with fertility problems; NICE Guidance (February 2013, updated September 2017)
- Kavanagh K, Wallace LA, Robertson C, et al; Estimation of the risk of tubal factor infertility associated with genital chlamydial infection in women: a statistical modelling study. Int J Epidemiol. 2013 Apr;42(2):493-503. doi: 10.1093/ije/dyt011. Epub 2013 Mar 14.
- Steinkeler JA, Woodfield CA, Lazarus E, et al; Female infertility: a systematic approach to radiologic imaging and diagnosis. Radiographics. 2009 Sep-Oct;29(5):1353-70. doi: 10.1148/rg.295095047.
- Ziogas AC, Tsakos E, Tsagias N, et al; Enhancing Fertility in the Same Cycle: A Case Report on Effects of Hysterosalpingo-Foam Sonography (HyFoSy) for a Couple With Mild Infertility. Cureus. 2024 Mar 19;16(3):e56495. doi: 10.7759/cureus.56495. eCollection 2024 Mar.
- Walker MH, Tobler KJ; Female Infertility.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 8 Sept 2027
9 Sept 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.