Viral warts
Excluding verrucae
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 29 Dec 2022
Meets Patient’s editorial guidelines
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Warts and verrucas article more useful, or one of our other health articles.
In this article:
Warts are common and usually harmless. They are caused by the human papillomavirus (HPV). Treatment is often not required or appropriate as the majority resolve spontaneously. Studies into the efficacy of the numerous possible treatment options continue to give conflicting results.
Continue reading below
How common are warts? (Epidemiology)
Warts are very common and thought to affect 7-12% of the population.1 No large studies are available; however, small studies suggest up to 30% of children and young adults may have warts.2
Incidence is thought to be higher in children of school age than in preschool children and to peak in teenage years.3
Causes of viral warts (aetiology)3
Warts are caused by HPV. There are well over one hundred types of HPV. Types 1, 2, 3, 4, 10, 27 and 57 are most often implicated in the aetiology of cutaneous warts. Infection of keratinocytes causes hyperkeratinisation and epidermal thickening.
HPV infection is acquired from direct contact with an affected individual or from the environment (eg, from contaminated floors or surfaces). It appears the virus can survive outside the body for a significant length of time, probably months or even years.
Trauma and wetness are contributory in contracting warts. The virus is more likely to spread around other parts of the body if the wart is damaged by trauma or scratching.
Continue reading below
Appearance2
Warts are classified according to their appearance or site. The British Association of Dermatologists (BAD) guidelines recognise the following four subtypes:
Common wart (verruca vulgaris)
Common wart

By Lucien Mahin, via Wikimedia Commons
These appear as papules and nodules with a keratotic and papillomatous surface. They occur anywhere but are most common on the hands in young people and children.
Plane wart, or flat wart (verruca plana)
Plane warts on chin

By Iffat Hassan, Taseer Bhat, Hinah Altaf, Farah Sameem, Qazi Masood, CC BY 4.0, via Wikimedia Commons
These are slightly elevated, flat-topped warts which may occur singly or in a group of many lesions.
Plantar wart, or verruca (verruca plantaris)
These are warts on the sole of the foot and are discussed in the separate Verrucae (Plantar Warts and Myrmecia Verrucae) article.
Genital wart (condyloma acuminatum)
These are discussed in the separate Anogenital Warts article
Other descriptions in common use include:1 4
Periungual wart
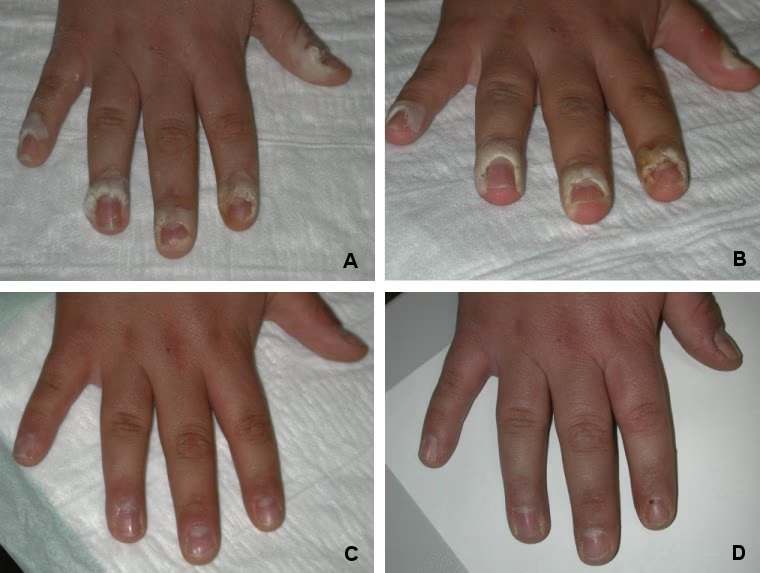
These are warts around the nails. They are more common in people who bite their nails. The image shows the progress of the treatment programme:
A. Before treatment.
B. Before second treatment.
C. Before third treatment.
D. 18 weeks after first treatment.
Periungual warts undergoing treatment
By Department of Dermatology and Allergology, Friedrich Schiller University Hospital, Jena, Germany, CC BY-SA 3.0 DE , via Wikimedia Commons
Filiform wart (verruca filiformis)
Filiform wart on eyelid

By Schweintechnik, Public domain, via Wikimedia Commons
These are small finger-like warts consisting of hyperkeratotic projections. They arise most often on the face or neck.
Mosaic warts
These are groups or clusters of plantar, or occasionally palmar, warts.
Diagnosis2
This is usually obvious clinically but, if necessary, paring down will produce pinpoint bleeding of the capillaries in the roots of the wart.
Continue reading below
Differential diagnosis1
Cutaneous horn.
Lichen nitidus.
Corns and calluses.
Angiokeratoma.
Viral warts treatment and management2 5
No treatment
Warts eventually resolve without therapy, so if they are asymptomatic and the individual is not immunocompromised, they do not necessarily need treatment. Treatment is time-consuming and may have side-effects so should only be recommended if the wart is symptomatic or the person requests it.
Salicylic acid
Topical salicylic acid has the best evidence base and is normally first-line treatment. There is no evidence for one preparation being more effective than another. The wart should be pared down prior to application. Daily treatment for at least 12 weeks is required.
Cryotherapy
Cryotherapy with liquid nitrogen every two weeks until the wart has gone (up to four months) may be effective. Clinicians vary in how long they freeze the wart for; usually liquid nitrogen is applied until a ring of frozen tissue is visible around the wart, typically 5-30 seconds. There is no evidence that there is any difference in effectiveness between a spray and a cotton bud. Over-the-counter preparations do not reach such low temperatures and are probably not as effective. Reported cure rates vary hugely. Cryotherapy may be painful, may cause blistering and should be avoided in young children.
Combination treatment
Applying salicylic acid (once the blistering from the cryotherapy has resolved) in between cryotherapy sessions may be beneficial. Again, the evidence is equivocal.
Other treatments used in secondary care3
A whole host of other treatments is used. These have been subject to trials of varying quality. BAD guidelines include the following potential options in their recommendations:
Physical removal by surgery, curettage, laser, or photodynamic treatment.
Puncturing with a needle (barbotage).6
Antimitotic agents such as:
Podophyllotoxin - topical.
Retinoids - topical or oral.
Bleomycin - intralesional.
Virucidal agents such as:
Formaldehyde.
Glutaraldehyde.
Immunomodulatory agent, including:
Imiquimod 5% - topical.
Interferon - intralesional.
Dinitrochlorobenzene - topical.
Diphencyprone - topical.
5- fluorouracil (5-FU) - topical.
Cantharidin.
Acupuncture (for plane warts).
Of these, the best evidence of efficacy is for bleomycin, 5-FU, laser and topical immunotherapy agents; however, all evidence is weaker than that for salicylic acid and cryotherapy.
Treatments used in the past but found by BAD to have insufficient evidence to recommend their use include:
Occlusion with duct tape.
Hypnosis.
Dithranol.
H2-receptor antagonists
Herbal treatments.
Homeopathy.
When to refer3
Reasons to consider referral to secondary care include:
Uncertain diagnosis.
Persistent symptomatic warts unresponsive to primary care treatment.
Multiple warts in immunocompromised individuals.
Facial warts. Facial warts should not be treated in primary care.
Extensive coverage (eg, mosaic warts).
Prognosis
Warts tend to resolve more quickly in younger age groups and in non-white skins.7 Resolution has been shown to occur in just over half of college students within two years.8 This was either with or without active treatment. Older adults may take longer.9
Complications are rare but include local infection or spread and malignant change. Such events are more common in immunocompromised people.
Prevention of viral warts
The risk of auto-inoculation can be reduced by avoiding biting the area (eg, nail biting), picking at the wart, trauma and maceration of the involved skin. Advise keeping nail files and pumice stones used for filing warts separate and not using for other areas of skin.
Further reading and references
- Fay DL; Is Cutaneous Cryosurgery the Best Treatment Option for Cutaneous Warts? Am Fam Physician. 2020 Dec 1;102(11):648.
- Kaur A, Brar BK, Kumar S, et al; A Randomized Comparative Study of MIP and MMR Vaccine for the Treatment of Cutaneous Warts. Indian J Dermatol. 2021 Mar-Apr;66(2):151-158. doi: 10.4103/ijd.IJD_700_20.
- Lynch MD, Cliffe J, Morris-Jones R; Management of cutaneous viral warts. BMJ. 2014 May 27;348:g3339. doi: 10.1136/bmj.g3339.
- British Association of Dermatologists Guidelines for the management of cutaneous warts; British Journal of Dermatology (2014)
- Warts and verrucae; NICE CKS, February 2020 (UK access only)
- Viral warts; DermNet NZ
- Truong K, Joseph J, Manago B, et al; Destructive therapies for cutaneous warts: A review of the evidence. Aust J Gen Pract. 2022 Oct;51(10):799-803. doi: 10.31128/AJGP-01-22-6305.
- Mclaughlin JS, Fischer TJ, Merrell GA; Treatment of Cutaneous Warts With Multiple Puncture Technique. Hand (N Y). 2019 Sep;14(5):689-690. doi: 10.1177/1558944718771389. Epub 2018 May 15.
- Bruggink SC, Eekhof JA, Egberts PF, et al; Natural course of cutaneous warts among primary schoolchildren: a prospective cohort study. Ann Fam Med. 2013 Sep-Oct;11(5):437-41. doi: 10.1370/afm.1508.
- Liu J, Li H, Yang F, et al; Epidemiology and Clinical Profile of Cutaneous Warts in Chinese College Students: A Cross-Sectional and Follow-Up Study. Sci Rep. 2018 Oct 18;8(1):15450. doi: 10.1038/s41598-018-33511-x.
- Al Aboud AM, Nigam PK; Wart.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 16 Dec 2027
29 Dec 2022 | Latest version

Feeling unwell?
Assess your symptoms online for free