Cervical rib
Thoracic outlet syndrome
Peer reviewed by Dr Toni HazellLast updated by Dr Colin Tidy, MRCGPLast updated 24 May 2022
Meets Patient’s editorial guidelines
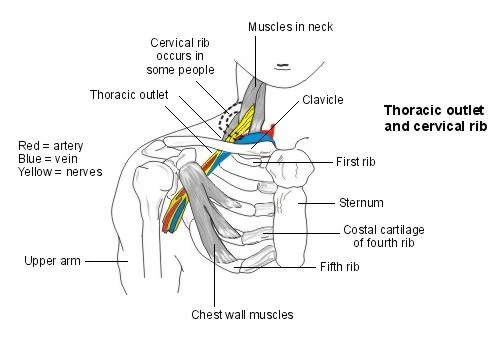
About 1 in 100 people are born with an extra rib called a cervical rib. About 1 in 10 people who have a cervical rib develop thoracic outlet syndrome. The thoracic outlet is a space, or passageway, that lies just above your first rib and behind your collarbone (clavicle). It runs from the base of the neck to the armpit. Your brachial plexus (a group of nerves that pass from the neck to the arm) and your subclavian artery and vein pass through the thoracic outlet. Thoracic outlet syndrome can occur when one or more of these structures is squashed (compressed) in the thoracic outlet. A cervical rib can sometimes cause this compression. Compression of the brachial plexus nerves is most common. This can cause pain and pins and needles in your arm on the affected side. Treatment can include painkillers, physiotherapy and sometimes surgery to relieve the compression caused by, for example, a cervical rib.
In this article:
Continue reading below
Understanding the ribs and the ribcage
Your ribs are curved bones that help to protect the heart and lungs. There are twelve pairs of ribs altogether. Together, these twelve pairs of ribs form your rib cage.
At the back, the head of each rib makes contact with (articulates) one of the thoracic vertebrae. Your vertebrae are your back bones. The thoracic vertebrae are the vertebrae in your chest area (thorax). There are twelve thoracic vertebrae. The cervical vertebrae are the vertebrae in your neck. There are seven cervical vertebrae.
For the first seven pairs of ribs, at the front, the other end of each rib is attached to some cartilage called costal cartilage. (Cartilage is a type of special connective tissue.) The costal cartilage connects each rib to your breastbone (sternum). The next three pairs of ribs are joined by their costal cartilage to the rib above them. The last two pairs of ribs are often called floating ribs because they are just joined to your vertebrae at the back and don't have a connection at the front.
What is a cervical rib?
About 1 in 200 people are born with an extra rib called a cervical rib. Because this is something that you are born with, cervical ribs are known as a congenital condition. At the back, this cervical rib connects to the seventh cervical vertebra in your neck. At the front, in some people a cervical rib can be 'floating' and have no connection. In other people the cervical rib can be connected to your first rib by a band of tough, fibrous tissue. In some others there may be an articulation (like in a joint) with their first rib.
A cervical rib can be present just on the right side, just on the left side, or on both sides.
Thoracic outlet
Continue reading below
What is the thoracic outlet?
The thoracic outlet is a space, or passageway, that lies just above your first rib and behind your collarbone (clavicle). There are also some muscles that surround the thoracic outlet. The thoracic outlet runs from the base of your neck to your armpit. You have a thoracic outlet on the left and the right side of your body.
A number of structures pass through your thoracic outlet, including some important blood vessels and nerves. The brachial plexus, a group of nerves passing from your neck to your arm, passes through the thoracic outlet. The subclavian artery and subclavian vein are blood vessels that pass through the thoracic outlet as they connect between your chest and your arm.
What is thoracic outlet syndrome and what causes it?
If you have thoracic outlet syndrome, the nerves and/or blood vessels in the thoracic outlet are squashed (compressed) for some reason. In most cases of thoracic outlet syndrome, it is nerves that are compressed. This compression causes the typical symptoms (see below). In some people, the subclavian artery or subclavian vein may be compressed. Sometimes, a combination of both nerves and blood vessels may be compressed.
Thoracic outlet syndrome usually only affects one side of your body. However, rarely, compression can occur in the thoracic outlet on both sides and so symptoms then occur on both sides. There are a number of different things that can cause compression of the nerves or blood vessels in thoracic outlet syndrome.
Having a cervical rib
About 1 in 10 people who have a cervical rib develop thoracic outlet syndrome. So, most people with a cervical rib do not develop any symptoms. Having a cervical rib can cause narrowing of your thoracic outlet, making compression of the structures that pass through it more likely.
Other congenital causes
Some people are born with an extra band of tissue underneath their skin around the thoracic outlet area, called a fibrous band. This can act a bit like an extra rib and cause thoracic outlet syndrome in some people. Extra (anomalous) muscles around the thoracic outlet that you may be born with can also cause thoracic outlet syndrome. Also, some people are born with an enlarged or elongated part of a vertebra in their neck which can cause compression in their thoracic outlet.
A recent accident
It is quite common for people with thoracic outlet syndrome to have a history of some kind of recent trauma to their neck - for example, whiplash following a car accident. Trauma during an accident can cause structures in your neck and chest wall to move slightly and narrow the thoracic outlet. If you break (fracture) your collarbone (clavicle), broken bone fragments or bleeding due to the fracture can also cause thoracic outlet syndrome.
A job or hobby that involves repetitive movements
Thoracic outlet syndrome can be more common in someone who has a job that involves very repetitive movements or a lot of overhead work. These movements can lead to 'wear and tear' of the nerves of their brachial plexus. Also, people who play a lot of sport, particularly sports that involve lots of arm movement are also more likely to develop thoracic outlet syndrome - for example, swimmers, javelin throwers and shot putters.
Poor posture
People with a poor posture and 'droopy' shoulders may be more likely to develop thoracic outlet syndrome. Sitting in front of a computer for long hours with a poor posture, an incorrect desk position, or an inadequate chair may be a cause. This poor posture can cause narrowing of your thoracic outlet.
Also, thoracic outlet syndrome can be a problem for women who have large breasts. Their breasts pull the muscles of their chest wall forwards and can cause narrowing of their thoracic outlet, leading to the typical symptoms.
Artery and vein problems
Narrowing and blockage of your subclavian artery or vein is another cause of thoracic outlet syndrome. Some people can have a congenital narrowing of one of these blood vessels. In these people, a blood clot can form if there is a period where the arm is overused - for example, weightlifting or working for long periods with arms raised above the head.
In other people, the blood vessel narrowing may be caused by, for example, a cervical rib. Because of this narrowing, a blood clot is more likely to form in the subclavian artery or vein, which can lead to the typical symptoms of blood vessel compression (see below).
Continue reading below
Who develops thoracic outlet syndrome?
Overall, thoracic outlet syndrome is more common in women than in men. It can occur from the ages of 20-80 years but is most common around the age of 40 years. As mentioned above, people with thoracic outlet syndrome have often had a recent injury to their neck. It is more common in people whose jobs involve repetitive movements or in some athletes whose sport involves a lot of arm movement.
Thoracic outlet syndrome symptoms
The symptoms of thoracic outlet syndrome depend on what is being squashed (compressed) in your thoracic outlet. As mentioned above, in most thoracic outlet syndrome cases it is the nerves of the brachial plexus rather than blood vessels that are compressed. Therefore, symptoms are more likely to be due to nerve compression. However, sometimes a combination of nerves and blood vessels may be compressed at the same time. This can give rise to a mixture of symptoms.
Thoracic outlet syndrome symptoms are usually just felt on one side of the body. Rarely, symptoms can occur on both sides.
Thoracic outlet syndrome symptoms due to nerve compression
The symptoms depend on which nerves of the brachial plexus are compressed. Most commonly you will develop pain and pins and needles in your hand and arm. You may particularly feel these along the inside of your arm and into your ring and little finger. Pins and needles are usually worse at night and can sometimes wake you from your sleep.
If different brachial plexus nerves are compressed, you may have neck, ear, upper back, upper chest and outer arm pain on the affected side. Some people also have headaches.
Your affected arm may feel weak. You may also notice that your affected hand gets very cold, especially in cold weather.
Symptoms due to blood vessel compression or blockage
In rare cases when your subclavian vein is compressed, your arm may become swollen and may sometimes appear a blue colour. The swelling may lead to pins and needles in your affected arm. Some people also develop pain in their arm. The symptoms tend to come and go and may be brought on at times when you are using your arms a lot. If you have a blood clot in your subclavian vein causing blockage of the vein, these symptoms will become constant and urgent treatment is needed.
In rare cases, when your subclavian artery is compressed, this means that blood is unable to get through to your arm and hand on the affected side as readily as it should do. Again this can lead to pain and pins and needles. Your arm and/or hand can appear pale white in colour and it can also feel cold. Like with the vein-related symptoms, the symptoms may be brought on by using your arms a lot.
How is thoracic outlet syndrome diagnosed?
Your doctor will usually start by asking you questions about your symptoms and examining you. If they suspect that you may have thoracic outlet syndrome, they may ask you to move your arms and shoulders into certain positions when they examine you. This is to try to bring on (induce) your symptoms. They may then suggest certain tests to look for the underlying cause. Usually, thoracic outlet syndrome is diagnosed after other conditions that can cause pain or pins and needles in one of your arms have been excluded. You may also be referred to a specialist.
Scans for a cervical rib
A chest X-ray and X-ray of your neck can show if you have a cervical rib. Other tests including an MRI scan or CT scan of your neck and upper chest area may help to rule out other causes for your symptoms. For example, arthritis in your neck may be causing compression of the nerves in your neck. Special tests called nerve conduction studies may sometimes be suggested. These look at the electrical activity of your nerves and can help to show which nerves are being compressed.
If your doctor suspects that you have compression of your subclavian artery or vein, other tests may be carried out to look for this. A test called angiography looks at your arteries and venography looks at your veins. Special tests known as Doppler studies can also look at blood flow through your arteries and veins.
Thoracic outlet syndrome treatment and management
Treatment depends on the underlying cause.
Blood vessel compression or blockage
In the rare case that you have blockage of one of your blood vessels by a blood clot, treatment with a medicine is needed urgently to break down the clot. This used to be in the form of an anticoagulant such as warfarin but recently 'clot busters' such as urokinase have also been used. Treatment with an anticoagulant may then be continued for a period of time to prevent further clots. Surgery may also be needed to relieve any squashing (compression) of your blood vessels. For example, removal of a cervical rib that may be squashing a blood vessel.
Nerve compression
There is not currently a general agreement about what treatment is best for this type of thoracic outlet syndrome. More trials are needed to determine the best treatment. However, in general, treatment is aimed at relieving your symptoms.
Physiotherapy may be helpful for some people and may include stretching exercises, exercises to improve posture and exercises to increase muscle strength and endurance. These exercises may all help to open up the thoracic outlet and relieve the compression.
You may also need to modify or change your work or sport activities. This may involve looking at the way that you sit in a chair or at your desk. An occupational therapist may be able to help with this.
Medicines such as non-steroidal anti-inflammatory drugs (NSAIDs) - for example, ibuprofen - may be helpful in relieving pain in some people. Paracetamol or stronger painkillers may sometimes be needed. Other treatments occasionally tried include a group of medicines called calcium-channel blockers and botulinum toxin injections.
In some cases, surgery to relieve the cause of the compression may be advised. For example, to ease pressure from a cervical rib, or from an extra muscle or fibrous band in your neck, or to repair a broken collarbone (clavicle) that is pressing on nerves (or blood vessels). Surgery is sometimes better performed at an early stage in the condition, before too much damage occurs. Your specialist will be able to advise.
What is the outlook (prognosis) for thoracic outlet syndrome?
In most people with thoracic outlet syndrome, the outlook is generally good and symptoms often improve over time.
If squashing (compression) or blockage of the subclavian artery or vein is diagnosed quickly and treated, a good recovery is possible. However, nerve compression symptoms can be difficult to treat in a few people. Persistent (chronic) pain and weakness with some loss of ability to use the affected arm may be experienced by some. This can sometimes be severe enough to affect quality of life.
Further reading and references
- Aljabri B, Al-Omran M; Surgical management of vascular thoracic outlet syndrome: a teaching hospital experience. Ann Vasc Dis. 2013;6(1):74-9. doi: 10.3400/avd.oa.12.00081. Epub 2013 Feb 28.
- Klaassen Z, Sorenson E, Tubbs RS, et al; Thoracic outlet syndrome: A neurological and vascular disorder. Clin Anat. 2013 May 29. doi: 10.1002/ca.22271.
- Povlsen B, Hansson T, Povlsen SD; Treatment for thoracic outlet syndrome. Cochrane Database Syst Rev. 2014 Nov 26;(11):CD007218. doi: 10.1002/14651858.CD007218.pub3.
- Jones MR, Prabhakar A, Viswanath O, et al; Thoracic Outlet Syndrome: A Comprehensive Review of Pathophysiology, Diagnosis, and Treatment. Pain Ther. 2019 Jun;8(1):5-18. doi: 10.1007/s40122-019-0124-2. Epub 2019 Apr 29.
- Spadlinski L, Cecot T, Majos A, et al; The Epidemiological, Morphological, and Clinical Aspects of the Cervical Ribs in Humans. Biomed Res Int. 2016;2016:8034613. doi: 10.1155/2016/8034613. Epub 2016 Nov 15.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 23 May 2027
24 May 2022 | Latest version

Feeling unwell?
Assess your symptoms online for free