Anticoagulants
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 19 Sept 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Anticoagulants are medicines that prevent the blood from clotting as quickly or as effectively as normal. Some people call anticoagulants blood thinners. However, the blood is not actually made any thinner - it just does not clot so easily whilst you take an anticoagulant.
Anticoagulants are used to treat and prevent blood clots forming in blood vessels, such as in arteries or veins.

Unsure about mixing medicines?
Check for possible interactions between medicines, supplements and foods before taking them together.
In this article:
Video picks for Heart and blood medicines
Continue reading below
How do anticoagulants work?
Our blood has a complex system of chemicals in it, which, when activated, cause blood clots to form. This is called the clotting cascade. This is normally a good thing; it's activated if we have an injury, like a bleeding wound. The clotting cascade causes a clot to form, stopping the bleeding.
However, some people get problems when blood clots form at the wrong time, or in the wrong places. Anticoagulants are used to treat this, or stop it from happening.
Anticoagulants interfere with different points in the clotting cascade.
Warfarin, acenocoumarol and phenindione block the effects of vitamin K. They are also called 'vitamin K antagonists'. Vitamin K is needed to make important proteins (clotting factors) in the clotting cascade. So, blocking vitamin K stops the clotting cascade from working as well. It usually takes two or three days for these anticoagulants to work fully.
A newer, and more frequently-used, type of anticoagulant medicines are the direct-acting oral anticoagulants (DOACs).
Dabigatran, apixaban, edoxaban and rivaroxaban prevent a blood chemical called thrombin from working. This stops a protein called fibrin from being made; fibrin is the main component of a blood clot. Dabigatran binds to thrombin and stops it from working. Apixaban and rivaroxaban stop thrombin from being made. All four medicines work quickly - within two to four hours.
Another type of anticoagulant is heparin.
One type of heparin, called unfractionated heparin (UFH) can be given through a drip into a vein. More commonly, a type called low molecular weight heparin (LMWH) is given as an injection under the skin.
Heparin activates a chemical called antithrombin; antithrombin then stops other clotting factors from working, reducing the blood's ability to clot. UFH starts working immediately if given into a vein, and LMWH works within a few hours of being given.
What are anticoagulants used for?
Back to contentsThere are two main reasons to use anticoagulants:
To treat someone who already has a blood clot, such as a clot in the veins of the leg (a deep vein thrombosis, or DVT), or in the arteries of the lung (a pulmonary embolus, or PE).
These don't actually get rid of the clot, but they prevent it from getting bigger, and prevent other blood clots from forming. Over time, the body breaks down the original clot on its own.
To prevent a blood clot, in someone who is at high risk of getting one.
People who are at high risk of getting a blood clot, and might be recommended anticoagulants, include people with:
A fast irregular heartbeat - atrial fibrillation or AF. Having AF is one of the most common reasons for taking an anticoagulant. Anticoagulants reduce the risk of having a stroke due to AF.
A mechanical heart valve. Anticoagulants stop blood clots forming on the metal heart valve, which could otherwise lead to a stroke.
Certain blood conditions which make blood clots much more likely; for example, antiphospholipid syndrome or inherited thrombophilias.
A temporary condition that makes them at high risk of having a DVT or PE, such as:
Recent surgery, especially hip and knee surgery.
Sometimes, pregnant women, or women who have just given birth.
Some people who have been admitted to hospital, especially people who are much less mobile than normal.
Sometimes, people who have had fractured (broken) a bone.
For many years, warfarin was the most commonly-used anticoagulant. DOACs are much more commonly-used now; most people find them easier to take, and they require monitoring much less often.
In 2021, the UK's National Institute for Health and Care Excellence (NICE) recommended that DOACs should be the preferred option for AF, instead of warfarin.
Speak to your doctor if you'd like to consider changing your anticoagulant.
Warfarin is still preferred in some groups of people, such as:
People with mechanical heart valves (warfarin is much better at preventing strokes than DOACs in people with mechanical heart valves).
People with antiphospholipid syndrome (warfarin seems to work better than DOACs for this).
People who need an INR target between 3 and 4 (it's not really possible to achieve a similar effect with DOACs).
Continue reading below
How and why does blood clot?
Back to contentsWithin seconds of cutting a blood vessel, the damaged tissue causes tiny cells in the blood (platelets) to become sticky and clump together around the cut. These activated platelets and the damaged tissue release chemicals which react with other chemicals and proteins in the blood, called clotting factors. There are 13 known clotting factors which are called by their Roman numbers - factor I to factor XIII. A complex cascade of chemical reactions involving these clotting factors, called the clotting cascade, quickly occurs.
The final step of this cascade of chemical reactions is to convert factor I (also called fibrinogen - a protein dissolved in the blood) into thin strands of a solid protein called fibrin. The strands of fibrin form a meshwork and trap blood cells and platelets, which form into a solid clot.
If a blood clot forms within a blood vessel it can cause serious problems. So, there are also chemicals in the blood that prevent clots from forming and chemicals that dissolve clots. There is a balance between forming and preventing clots. Normally, unless a blood vessel is damaged or cut, the balance tips in favour of preventing clots forming within blood vessels. However, sometimes a clot forms within a blood vessel which has not been injured or cut.
Anticoagulants side-effects
Back to contentsThere are a number of possible side-effects with anticoagulants and it is not possible to list all these here. However, the major side-effect of all anticoagulant medicines is major bleeding. Anticoagulants don't cause spontaneous bleeding, but they do make bleeding worse if it happens for another reason. So, for example, people who have a bleeding stomach ulcer may bleed more heavily if they are taking an anticoagulant.
People who take warfarin, acenocoumarol and phenindione need to have regular blood tests to measure how quickly the blood clots. See the leaflet that comes with your particular brand for a full list of possible side-effects and cautions.
Anticoagulants sometimes react with other medicines that you may take. So, make sure your doctor knows of any other medicines that you are taking, including ones that you have bought rather than been prescribed.
Continue reading below
Are anticoagulants safe?
Back to contentsAnticoagulants are commonly-used medications, and most people don't have major problems with them.
They do have risks; the most important risk being major bleeding. These have to be weighed against the benefits of anticoagulants: preventing major problems from blood clots, such as strokes or blood clots on the lung.
The risks and benefits of anticoagulants differ from person to person.
For example, a younger person with atrial fibrillation who has no other medical problems may have a very low risk of having a stroke. For them, anticoagulation may only have a very small benefit. Other people with atrial fibrillation (particularly older people with other medical conditions) may have a much higher risk of stroke, and so anticoagulants may be much more helpful in reducing that risk and preventing them from having a stroke.
Likewise, the safety of anticoagulants differs from person to person. Some people are unlikely to have major bleeding, whereas others have a much higher risk. For example, people who drink lots of alcohol, or people who take other medications that make bleeding more likely, are at higher risk of bleeding problems.
Your doctor should discuss the benefits and risks of anticoagulants in your situation with you, to help you understand what they are, and decide whether or not to take them.
There are various different calculators available to help clinicians estimate the benefits and harms of anticoagulation in different situations. For example, SPARCtool (see Further Reading) can be used to estimate the pros and cons of anticoagulants in atrial fibrillation.
What if I bleed whilst taking an anticoagulant?
Back to contentsOne indication that you may be taking too much anticoagulant is that you may bleed or bruise easily. Also, if you bleed, the bleeding may not stop as quickly as normally. If any of the following serious bleeding side-effects occur while you are taking an anticoagulant you should see a doctor urgently:
Passing blood in your urine or stools (faeces). Note: blood in faeces may be bright red. But, if you are bleeding from your stomach or small intestine, your faeces may turn a black or plum colour. This is called melaena. You should seek urgent medical attention if you have melaena.
Heavy bleeding during a period or other heavy vaginal bleeding (in women).
Severe bruising.
Prolonged nosebleeds (lasting for longer than 10 minutes).
Blood in your sick (vomit).
Coughing up blood.
If you cut yourself or have any other bleeding, you should seek medical help as soon as possible if the bleeding does not stop as quickly as you would expect.
Head injury and anticoagulants
Back to contentsAnticoagulants increase the risk of bleeding inside the skull after a head injury. Bleeding inside the skull and around the brain can be life-threatening, and may require emergency brain surgery.
If you have a head injury, you should seek immediate medical attention. This usually means going straight to your nearest Emergency Department; make sure they know which medications you are taking.
The UK's national guidelines from NICE used to recommend that everyone taking anticoagulant treatment with a head injury should have a CT head scan to rule out bleeding inside the skull.
This changed slightly in 2023, when NICE instead advised that healthcare professionals could use their judgement in individual cases as to whether a CT scan is needed or not. It's still important to see a healthcare professional to be assessed. Most clinicians still have a low threshold for doing a CT scan.
What else should I be aware of when taking an anticoagulant?
Back to contentsSome other important things to consider on anticoagulants are:
If you have any medical treatment you should always tell the healthcare professional looking after you that you are taking an anticoagulant. It is important that they know you may take longer to stop bleeding.
If you take warfarin you should always carry with you the yellow anticoagulant treatment booklet which will be given to you. This is in case of emergencies and a doctor needing to know that you are on warfarin, and at what dose.
If you have surgery or an invasive test then you may need temporarily to stop taking an anticoagulant; always ask the people performing the operation or test beforehand what you should do.
Tell your dentist that you take an anticoagulant. Most dental work does not carry a risk of uncontrollable bleeding. However, for dental extractions and surgery, you may need temporarily to stop taking an anticoagulant.
You should limit the amount of alcohol that you drink to a maximum of one or two units in any day and never binge drink.
Ideally, try to avoid activities that may cause abrasion, bruising, or cuts (for example, contact sports). Even gardening, sewing, etc, can put you at risk of cuts. Do be careful and wear protection such as proper gardening gloves when gardening.
Take extra care when brushing teeth or shaving, to avoid cuts and bleeding gums. Consider using a soft toothbrush and an electric razor.
Try to avoid insect bites. Use a repellent when you are in contact with insects.
Who cannot take an anticoagulant?
Back to contentsYou cannot take anticoagulant tablets if you:
Are pregnant (if you are pregnant and need anticoagulation, you may be treated with injections of a medicine called heparin).
Have a stomach ulcer.
Have had a bleed into the brain (a haemorrhagic stroke).
Take certain medicines that may interfere with your anticoagulant (these vary between the different anticoagulants - your doctor or pharmacist can advise).
Have major bleeding and this is not being treated.
Are going to have surgery where you might be at risk of a major bleed.
Have very high blood pressure.
Have severely reduced kidney function - the degree of reduced kidney function at which you cannot take anticoagulation varies between different anticoagulant drugs. Sometimes, anticoagulants are used under expert advice.
For a full list of people who cannot take an anticoagulant, please see the leaflet that comes with your medicine.
Patient picks for Heart and blood medicines

Treatment and medication
Potassium-sparing diuretics
Diuretics are medicines which increase the amount of fluid removed from the body when we pass urine. Potassium-sparing diuretics are one type of diuretic. They are weak diuretics usually prescribed in combination with other types of diuretics. They are used to increase the amount of fluid passed from the body in urine, whilst also preventing too much potassium being lost with it. Side-effects are uncommon when routine low doses are used. Most people are able to take these medicines.
by Dr Doug McKechnie, MRCGP
Treatment and medication
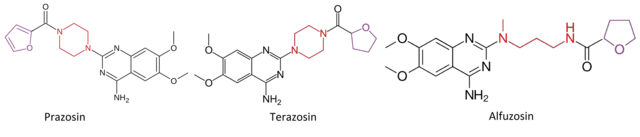
Alpha-blockers
Alpha-blockers are medicines that are mainly used to treat high blood pressure (hypertension) and problems with passing urine in men who have enlargement of the prostate gland. Prostate gland enlargement is also called benign prostatic hyperplasia (BPH).
by Dr Doug McKechnie, MRCGP
Further reading and references
- Head injury: assessment and early management; NICE Clinical Guideline (January 2014, updated September 2019) (Replaced by NG232 (refid=66597)
- Atrial fibrillation: diagnosis and management; NICE guideline (April 2021 - last updated June 2021)
- Anticoagulation - oral; NICE CKS, July 2024 (UK access only)
- SPARCtool; Loewen, P. Sept 2023.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 17 Sept 2028
19 Sept 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.