Pressure sores
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 21 Aug 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
A pressure sore is also known as a 'bed sore' or a 'pressure ulcer'. It is a sore or broken (ulcerated) area of skin caused by irritation and continuous pressure on part of your body.
Pressure sores are more common over places where your bones are close to your skin (bony prominences) such as your heels, the lower part of your back and your bottom. There are various things that can increase your risk of developing a pressure sore. In particular, risk increases if your mobility is reduced for some reason and you are spending long periods lying in bed or sitting in a chair.
There are various measures you can take to prevent most pressure sores developing. These include changing your position as much as possible and also using pressure-relieving devices.
In this article:
Continue reading below
What is a pressure sore?
A pressure sore is an ulcerated area of skin caused by irritation and continuous pressure on part of your body. It starts as an area of skin damage. The damage can then spread to your tissues underlying your skin. In very severe cases, there can be permanent damage to muscle and bone underneath your skin. This is not common though. Pressure sores can be very painful and can take a very long time to heal.
Pressure sore symptoms
Pressure sores can affect any area of the body but are more common over places where bones are close to the skin (bony prominences). Common areas for pressure sores to occur are around the lower part of the backbone and buttocks (sacrum), heels, elbows, hips, back, bottom, the back of the head and shoulders.
Initial signs may just be discomfort, or tingling and itchiness in these areas.
Small areas of the skin change colour. Red patches on white skin, and purple or blue on brown or black skin. When you press on this patch it doesn't change colour.
The skin patch also changes how it feels to touch. The patch may feel warmer, harder or spongy.
Continue reading below
What do pressure sore look like?
Pressure sores initially look like areas of discoloured skin - as above. If they get worse the skin may look like a blister which develops into an ulcer. The image below shows an ulcer-type pressure sore over the base of the spine (sacrum).
Pressure sore
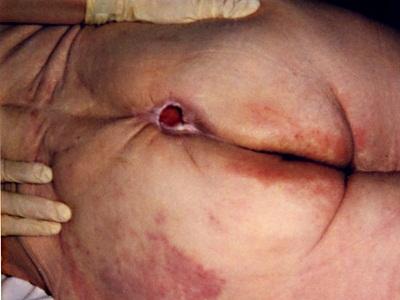
By Mennfield, via Wikimedia Commons
If pressure sores are not treated the ulcer can involve deeper layers of the skin, muscle and even expose bone underneath.
Pressure sores can develop very quickly. In people who are at high risk (see below), it can take less than an hour for a pressure sore to develop.
Who is at risk of pressure sores?
Most pressure sores occur when someone is admitted to hospital. They affect between 1 to 5 in every 100 people admitted to hospital. However, pressure sores can also develop in someone at home, or in a nursing or residential home.
A pressure sore is more likely to develop if you:
Are seriously ill (including someone in an intensive care unit).
Are not very mobile (for example, you may be confined to a chair or a bed), particularly if you are not able to change your position without help from someone else.
Have had a spinal cord injury (this means you are unable to move or feel your legs and sometimes your arms).
Have a poor diet.
Are wearing a prosthesis (for example, an artificial limb), a body brace or a plaster cast.
Are a smoker.
Are incontinent of urine or stool (faeces). This causes damp skin which is more easily damaged.
Have diabetes (this can affect sensation and ability to feel pain over parts of your body).
Have chronic obstructive pulmonary disease (COPD) or heart failure.
Have Alzheimer's disease, Parkinson's disease or rheumatoid arthritis.
Have recently had a broken hip or undergone hip surgery.
Have poor circulation in your legs or arms, caused by narrowing of your arteries by atheroma (peripheral arterial disease).
Continue reading below
What causes pressure sores?
Pressure
Pressure sores are caused by the pressure from the weight of the body pressing down on the skin. They usually occur when a place where bone is close to skin (a bony prominence) and is pressed against a surface such as a chair or a bed. This compresses the skin and underlying tissues and can also damage blood vessels. Rubbing (friction) of the skin can also play a part in the formation of a pressure sore.
Sliding layers of skin
Spending long periods in bed or in a chair, people may slide down and need to be pulled back up again by someone else (or they may be able to pull themself back up). However, as these sliding and pulling movements happen, the layers of the skin also slide over each other, as well as over the tissues under the skin. These sliding, or 'shearing', forces can also contribute to pressure sore formation. Changes to the skin as it ages may make this sliding of the skin more likely.
Moisture
A lot of moisture around the skin (for example, if there is urinary or stool (faecal) incontinence or sweating a lot) can increase the effects of pressure, friction and shearing forces. Damp skin becomes softer and more fragile. Try to keep the skin clean and dry. Use a moisture barrier cream over the buttocks and pelvic area.
Using the correct preventative measures (see below) should mean that most pressure sores are avoidable.
Pressure sore stages
Pressure sores can look different depending on how severe they are. They are graded depending on their severity and how deep they go:
Grade 1 - your skin is permanently red but is not broken at all. It may feel warm, hard or slightly swollen. In dark-skinned people, your skin may be purple or blue in colour.
Grade 2 - the skin is broken (an ulcer) but the ulcer is still superficial. It may look like a blister or abrasion.
Grade 3 - the ulcer goes through the full thickness of the skin and there is damage to the tissues underneath the skin.
Grade 4 - this is the most severe form. The ulcer is deep and there is damage to muscle or bone underneath.
Pressure sore treatment
If you already have a pressure sore, it should be assessed by a qualified healthcare professional. They may want to take a tracing or a photograph of the sore. This can then be used to monitor your response to treatment. They should be able to determine what grade of pressure sore you have, look for any signs of infection and try to work out what caused the sore.
For a pressure sore to heal, you need to change your position as much as possible (as described above) and also to use pressure-relieving mattresses and cushions. These both help to relieve the pressure on the pressure sore.
Seating is very important for pressure sores on the buttocks. The use of pressure cushions alone will not help the pressure sore to heal if posture is not properly assessed and the cause of the pressure sore identified. Chairs that are the wrong size or not adaptable to posture and positioning will increase the risk of developing pressure damage.
Current recommendations are that someone with a pressure sore should use a high-specification foam mattress. A high-specification foam or equivalent pressure-redistributing cushion should be used if you use a wheelchair or sit for prolonged periods.
Other treatments are often needed for pressure sores. These may include:
Pain relief - a pressure sore can be painful. Simple painkillers like paracetamol may be helpful. Sometimes stronger painkillers are needed.
A change to your diet - a poor diet can slow the healing of a pressure sore.
Dressings - various different dressings may be used, including gel and foam-based dressings and keeping the wound clean with mild soap and water.
Antibiotics - these may be needed if there are any signs of infection.
Surgery - sometimes surgery is needed to remove damaged or dead tissue or skin. The medical term that is used for this type of surgery is 'debridement'. Sometimes plastic surgery may be used to close a pressure sore that is not healing. Skin grafts may be needed.
Are there any complications of pressure sores?
If treatment is started early, pressure sores usually cause few if any complications. Complications are much more likely with advanced stages of pressure sores.
A pressure sore can become infected. Rarely, this infection can spread to the surrounding skin (cellulitis), to the blood (causing 'blood poisoning', or sepsis), or it can spread to the bone underneath the pressure sore (causing osteomyelitis). In severe cases, a pressure sore can cause permanent damage or loss of muscle or bone underneath the affected area of skin.
Other possible complications that may occur with advanced stages of a pressure sore include anaemia, kidney failure, coma and even death.
Pressure sore prevention
The National Institute for Health and Care Excellence (NICE) has produced guidelines with recommendations for best practice in preventing pressure sores (ulcers). NICE recommends that all people who are admitted to hospital, a nursing home or similar, or people who are receiving nursing care at home, should be assessed for their risk of developing a pressure sore. This is usually done by a healthcare professional (usually a nurse). This assessment should be reviewed regularly because the situation may change.
There are various pressure sore risk assessment scales that may be used, looking at factors such as diet, mobility, continence, consciousness level and any underlying illnesses, etc.
If you are assessed and found to be at increased risk then one or more of the following may be suggested:
1. Change position as much as possible
Ideally, you should get up and move around as much as possible. However, if this is not feasible, you should change your position at least every 15 minutes when you are sitting or lying in bed. You may need help from someone else to change your position. Changing your position means that you are relieving pressure on areas of your body that may be prone to developing pressure sores. Ask your healthcare professional for advice about:
How to sit or lie.
How often to move or have help with a position change and what position should be moved to.
How to support the feet.
How to maintain a good posture (for example, how to stop the body slipping down in a chair).
2. Eat and drink the right things
It is important that you are eating a balanced diet and drinking plenty of fluids to help prevent pressure sores. Your healthcare professional may discuss your diet with you to see if it is likely that you are lacking in any nutrients. They may refer you to a dietician and/or you may be advised to take some supplements.
3. Use pressure-relieving devices
There are various devices that are available that can help to relieve pressure and prevent pressure sores. They include special beds, mattresses, cushions and overlays (these are placed on top of a mattress). They can work in the following ways:
Spreading out the pressure (for example, by moulding around the body).
Regularly removing pressure from different parts of the body (these are the more 'high-tech' devices).
All the surfaces that the at-risk person sits or lies on need to be considered for pressure-relieving devices. This includes chairs and beds.
Mattress pads (overlays) lie on top of the mattress to help decrease pressure on the skin. This helps to prevent sores in people who have to stay in bed most of the time. There are many different types of mattress pads, such as egg crate mattress pads and alternating pressure pads.
4. Make regular checks of the skin
A healthcare professional should check the skin regularly to look for any signs of a pressure sore. You or your carer may also be able to check your skin (this may sometimes need the help of a mirror). Tell your healthcare professional if there are any areas of your skin that you are worried about.
What is the outlook for pressure sores?
The outlook (prognosis) for pressure sores is usually good if they are treated before they reach an advanced stage and before any complications develop.
The outcome can be much worse for advanced stages of pressure sores that aren't treated early enough. The outcome will also depend on where the pressure sore is on the body, their general well-being and how well they respond to the treatments.
If someone has a pressure sore, they're more likely to develop another pressure sore in the future.
Patient picks for Other skin problems

Skin, nail and hair health
Corns and calluses
Corns and calluses on the feet are thickened areas of skin that can become painful. They are caused by excessive pressure or rubbing (friction) on the skin and can lead to foot problems, especially on walking. The common cause is wearing ill-fitting shoes. A person who is qualified to diagnose and treat foot disorders (a podiatrist) can cut away (pare) corns and calluses and can advise on footwear, shoe inserts and padding to prevent recurrences.
by Dr Colin Tidy, MRCGP

Skin, nail and hair health
Lipoma
A lipoma is a non-cancerous (benign) fatty lump that usually causes no symptoms or problems. Most lipomas are small and can be left alone. However, a lipoma that develops under the skin can sometimes look unsightly. If required, it can be removed by a simple operation done under local anaesthetic.
by Dr Doug McKechnie, MRCGP
Further reading and references
- Pressure ulcers: prevention and management of pressure ulcers; NICE Clinical Guideline (April 2014 - last verified by NICE 2018)
- Boyko TV, Longaker MT, Yang GP; Review of the Current Management of Pressure Ulcers. Adv Wound Care (New Rochelle). 2018 Feb 1;7(2):57-67. doi: 10.1089/wound.2016.0697.
- Pressure Ulcer Guidelines; European Pressure Ulcer Advisory Panel (2019)
- Gefen A, Alves P, Ciprandi G, et al; Device-related pressure ulcers: SECURE prevention. J Wound Care. 2020 Feb 1;29(Sup2a):S1-S52. doi: 10.12968/jowc.2020.29.Sup2a.S1.
- Shi C, Dumville JC, Cullum N, et al; Alternating pressure (active) air surfaces for preventing pressure ulcers. Cochrane Database Syst Rev. 2021 May 10;5(5):CD013620. doi: 10.1002/14651858.CD013620.pub2.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 19 Aug 2028
21 Aug 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free