Aspiration pneumonia
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Philippa Vincent, MRCGPLast updated 10 Sept 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Aspiration pneumonia is a lower respiratory tract (chest) infection caused by bacteria which have leaked into the lungs from fluid from the stomach or mouth. This can be as a result of vomiting or an inability to swallow properly. It causes symptoms of a lower respiratory tract infection (cough, fever, shortness of breath) and is usually treated with antibiotics.
In this article:
Video picks for Chest and lung infections
Continue reading below
What is aspiration pneumonia?
Aspiration pneumonia is a condition caused by fluid leaking into the chest from the stomach or mouth. This liquid causes a bacterial infection in the lungs. It is most common in people who have a condition making swallowing difficult - typically the very elderly, the very young or people with neurological disabilities (for example, people with multiple sclerosis or following a stroke).
Research suggests that about 1 in 10 cases of pneumonia that occur outside hospital (community-acquired pneumonia) is an aspiration pneumonia. Men are affected more than women.
It commonly occurs in hospital, mainly because hospital inpatients are likely to have reduced mobility which is another risk factor. Patients in residential care or nursing homes are also more likely to develop aspiration pneumonia because they are also likely to be bed-bound and have reduced mobility.
Aspiration pneumonia
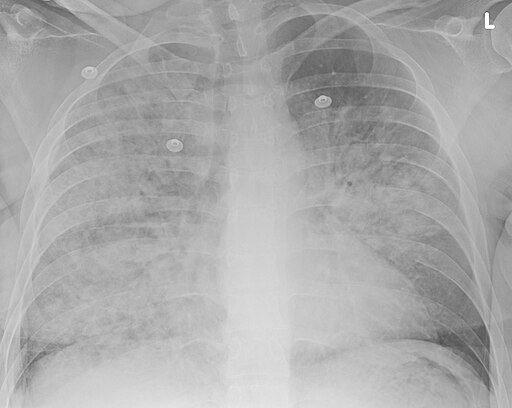
© Doc James, CC BY-SA 4.0, via Wikimedia Commons
Doc James, CC BY-SA 4.0, via Wikimedia Commons
Symptoms of aspiration pneumonia
Back to contentsSymptoms tend to be the same as with other pneumonias. Aspiration pneumonia causes a cough, fever and a feeling of being generally unwell. It can often cause aches, pains and headaches. People with aspiration pneumonia also often feel short of breath. There may also be a racing pulse and people often have a faster breathing rate than normal.
Early symptoms
These include:
Feeling generally unwell, with a high temperature (fever), headache, sickness (vomiting), reduced appetite and muscle aches.
A cough is the key feature.
Later symptoms
The breathing rate and pulse may become rapid.
Breathlessness, difficulty in breathing and chest pain which is worse when breathing in deeply may occur.
The oxygen levels in the blood may reduce.
Continue reading below
Causes of aspiration pneumonia
Back to contentsAspiration pneumonia is caused by saliva, food or stomach contents entering the lungs. This can be whilst attempting to swallow or following vomiting. These contain bacteria which don't cause harm in the mouth or stomach but can cause harm when inhaled into the lungs.
Risk factors for aspiration pneumonia
Aspiration pneumonia does not usually affect healthy people because the normal swallowing mechanism and the gag reflex is good enough to prevent this.
The risk of aspiration is increased in conditions which:
Reduce the level of consciousness such as
Drug overdose.
Alcohol use disorder.
Seizures.
Use of sedative medication.
Reduce the ability of the nerves to co-ordinate swallowing effectively or reduce the gag reflex such as:
Stroke.
Multiple sclerosis.
Parkinson's disease.
Dementia.
Brain tumours.
Increase the risks of fluid or food to enter the airway such as:
Nasogastric tube.
Gastro-oesophageal reflux disease.
Tracheostomy.
Being bed-bound or having poor mobility, particularly with difficulty keeping upright.
Tracheo-oesophageal fistula - a channel between the trachea (upper airway) and the oesophagus.
A variety of bacteria may be involved - for example:
Those that are always around the mouth and throat, such as Streptococcus pneumoniae, Staphylococcus aureus and Haemophilus influenzae.
Those acquired in hospitals, such as Klebsiella pneumoniae, Escherichia coli, Pseudomonas aeruginosa and meticillin-resistant S. aureus (MRSA).
Diagnosis of aspiration pneumonia
Back to contentsThis is usually made clinically because of the history of the condition and the examination. Other conditions that can cause some similar symptoms include:
Other causes of pneumonia, including viruses.
Upper respiratory tract infections.
Foreign body in the airway (respiratory system).
Diseases of the heart or blood circulation system.
Will I need any tests?
Sometimes no tests are needed if the diagnosis is clear. Tests may be required at times and these may include:
Blood tests.
A test of the phlegm (sputum culture).
A chest X-ray.
Occasionally a CT scan of the lungs.
Continue reading below
Treatment of aspiration pneumonia
Back to contentsAntibiotics will usually be required. These can be given orally (by mouth) if well enough to be at home.
Where someone is too unwell to be managed at home, intravenous antibiotics (into a vein) will usually be used.
Other medication may also be needed.
Assessment of any swallowing difficulties may be required - these will be carried out by speech and language therapists.
Complications of aspiration pneumonia
Back to contentsIf aspiration pneumonia isn't treated, the following complications can result:
A lung abscess (a collection of pus in the lung tissue).
Severe aspiration pneumonia can result in acute respiratory distress syndrome (a condition in which the lungs suddenly fill up with fluid and breathing becomes very difficult). This is a medical emergency as it is often fatal.
Prognosis of aspiration pneumonia
Back to contentsIn people with aspiration pneumonia who are unwell enough to be treated in hospital, between 1 in 6 and 1 in 10 will die during their admission to hospital. Patients with aspiration pneumonia are at increased risk of dying from all causes (this is because many patients with aspiration pneumonia are very frail before developing aspiration pneumonia). They are also at increased risk of developing other pneumonias in the future.
How can aspiration pneumonia be prevented?
Back to contentsPatients who may have swallowing difficulties, for example after a stroke, should be assessed to see if they can swallow safely. This is also the case for people with other long-term neurological conditions such as Parkinson's disease.
People who have a problem with swallowing can be helped by using strategies such as the "chin tuck" - touching the chin to the chest whilst swallowing improves the swallow and reduces the risk of aspiration. There is evidence that medications such as angiotensin converting enzyme inhibitors (ACE inhibitors, usually used to reduce blood pressure) can help to reduce the risk of aspiration. Traditionally, thickening foods and fluids has been used to reduce the risk of aspiration but there is little evidence of benefit and this can often result in people not wanting to eat or drink as much as the taste and texture of the food is impaired. This is important as having good nutrition improves the chances of getting better after an episode of aspiration pneumonia.
Sometimes a feeding tube (a naso-gastric, or NG, tube) can be used in people who at increased risk of aspiration pneumonia. This can be used short-term for people whose swallow is expected to improve, or long-term for those who have a permanently unsafe swallow. It is important that people are assessed carefully as they are not appropriate for everyone.
Patient picks for Chest and lung infections

Chest and lungs
SARS and MERS virus
Severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) are viral infections. Both infections can cause very serious illnesses that particularly affect the lungs. SARS caused many infections, especially in Asia, in 2002-2004 but was not heard of for some time. A SARS-CoV-2 (COVID-19) outbreak emerged in Wuhan, China in December 2019. This spread rapidly and was declared a global pandemic in 2020. MERS was first recognised in the Middle East in 2012. Most of the initial infections were in the Middle East. However, by February 2018, the World Health Organization (WHO) had reported cases in many other countries.
by Dr Hayley Willacy, FRCGP

Chest and lungs
Tuberculosis
Tuberculosis (TB) is an infection with a germ (bacterium) called Mycobacterium tuberculosis. If you have symptoms, or a doctor can find signs of the infection when examining you, this is known as active tuberculosis. If you have TB infection without any signs or symptoms, this is known as latent TB.
by Dr Colin Tidy, MRCGP
Further reading and references
- Pneumonia (community-acquired): antimicrobial prescribing; NICE Guidance (September 2019)
- Pneumonia (hospital-acquired): antimicrobial prescribing; NICE Guidance (September 2019)
- Sanivarapu RR, Vaqar S, Gibson J; Aspiration Pneumonia.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Sept 2027
10 Sept 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.