Atrial flutter
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGPLast updated 6 Feb 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Continue reading below
What is atrial flutter?
Atrial flutter is one of the more common atrial arrhythmias (supraventricular arrhythmias). Many patients with atrial flutter have associated atrial fibrillation.
There are many similarities in clinical presentation and management, and the guideline from the National Institute for Health and Care Excellence (NICE) makes hardly a distinction, stating the guideline for atrial fibrillation applies to patients with atrial flutter, specifying a particular management in the latter only in one sentence.1
European and American guidelines cover the conditions separately although there, much of the management is the same.2 3 Both arrhythmias can cause clinical symptoms such as palpitations, syncope, heart failure and fatigue, and are associated with a risk of thrombus formation and thromboembolism.
See also the separate Atrial Fibrillation article.
How is atrial flutter characterised? (Pathophysiology)2 4
Back to contentsAtrial flutter is characterised by an abnormal and rapid heart rhythm.. There is typically an atrial rate of around 300 beats per minute (bpm) and a ventricular rate that may be fixed or be variable.
Atrial flutter is a macro-reentrant tachycardia and can be classed as typical or atypical atrial flutter depending upon the origin. Flutter waves are seen on ECG. Like atrial fibrillation, it can be paroxysmal or persistent.
In typical atrial flutter the rhythm has its origin in the right atrium at the level of the tricuspid valve. This is also called cavotricuspid isthmus (CTI) or common atrial flutter. The ECG pattern shows regular mainly negative atrial deflections in the inferior leads with a 'saw-tooth pattern' at rates of 240-350 bpm per minute.
In atypical atrial flutter, the origin is elsewhere in the right atrium or the left atrium. Various circuits have been described. This is also called non-cavotricuspid isthmus-dependent atrial flutter. ECG patterns are variable and there may be faster atrial rates than in typical flutter.
Continue reading below
How common is atrial flutter? (Epidemiology)2 4
Back to contentsAtrial flutter is less common than atrial fibrillation, but epidemiology is less well studied. It is one tenth as common as atrial fibrillation.5
It is the second most common arrhythmia after atrial fibrillation.
Atrial flutter is commonly associated with atrial fibrillation. On presentation the two often alternate. Around 50% of those presenting with atrial flutter alone are said to develop atrial fibrillation within the next eight years.
The prevalence increases with age. With an ageing population, it is becoming increasingly common.
Atrial flutter is more common in men, with males accounting for 80% of cases.
Systemic embolism is less common than it is in atrial fibrillation (occurring about 30% as frequently). There is no difference if there is associated atrial fibrillation.
Causes of atrial flutter (aetiology)2 6
Back to contentsAge is the most important risk factor. Structural abnormalities are also a strong risk factor, with left atrial dilatation possibly one of the strongest predicting factors for the likely development of atrial flutter. This explains many of the associations below.
Coronary heart disease.
Atrial dilation due to septal defects, pulmonary emboli, mitral or tricuspid valve dysfunction or chronic ventricular failure.
Cardiac surgery and ablation procedures.
Obesity.
Alcohol abuse.
Atrial myxoma.
Pericarditis.
Sick sinus syndrome, cardiac conduction pre-excitation syndromes - eg, Wolff-Parkinson-White syndrome.
Thyrotoxicosis, phaeochromocytoma, electrolyte imbalance.
Very high-intensity sports.
One study found use of non-aspirin non-steroidal anti-inflammatory drugs (NSAIDs) - particularly new use - has been found to be associated with a 40-70% increased relative risk of developing atrial flutter or fibrillation.7 Other studies in the literature seem to relate to atrial fibrillation but a later meta-analysis found a 12% increased risk associated with NSAID use.8
Continue reading below
Symptoms of atrial flutter (presentation)
Back to contentsIt may be asymptomatic but can present in a variety of ways. Initial presentation varies from a coincidental ECG finding to being in extremis with heart failure or embolic stroke.
May present with ECG findings of atrial flutter.
Mild symptoms include palpitations, irregular heartbeat, fatigue, dyspnoea, chest pain, dizziness.
Syncope.
Heart failure.
Thromboembolism with transient ischaemic attacks or stroke.
Pulse may be irregular or regular, but is usually rapid. Arteriovenous conduction is usually 2:1, making the ventricular rate approximately 150 bpm. 1:1 atrioventricular (AV) conduction may lead to haemodynamic collapse. Carotid massage may decrease the ventricular rate.
Atrial flutter waves may be present in the jugular venous pulse.
May be associated with signs of underlying causes - eg, thyrotoxicosis, alcoholism, pericarditis, valvular dysfunction or septal heart defects.
Heart failure, hypotension and respiratory distress may be present.
Differential diagnosis
Back to contentsThis includes other supraventricular tachyarrhythmias such as:
Diagnosing atrial flutter (investigations)
Back to contentsFurther assessment is focused on identifying any specific underlying cause and an assessment of cardiac function:
Electrocardiogram:
The common form of typical atrial flutter has saw-tooth flutter waves, best seen in leads II, III, and aVF, with atrial rates of 240-340 bpm.9
ATRIAL FLUTTER
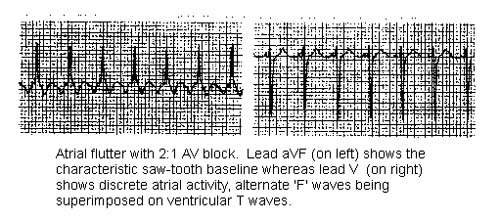
The ventricular response may be regular or irregular.
Variable AV conduction can also be seen (commonly present with 2:1 or 3:1 AV conduction).
May be normal if paroxysmal and between episodes of atrial flutter. Ambulatory ECG monitoring and event recorders may be required.
Investigations for associated causes: CXR, TFTs, FBC, ESR, renal function and LFTs.
Echocardiogram:
To evaluate underlying cardiac function, structural abnormalities, evidence of coronary artery disease or pericardial fluid.
If immediate cardioversion is considered, it is also used to detect any thrombus formation. A transoesophageal echocardiogram is ideal so the atrial appendage can be viewed to exclude thrombus there.
Management of atrial flutter1 2 10
Back to contentsLike atrial fibrillation, treatment options for atrial flutter involve either controlling the ventricular rate or attempting to restore and maintain sinus rhythm. However, atrial flutter generally responds less well to drug treatment than atrial fibrillation. If haemodynamically unstable: urgent rate control or cardioversion is required.
Control of the ventricular rate is usually an interim measure pending restoration of sinus rhythm:
Ventricular rate can be controlled by a beta-blocker, diltiazem hydrochloride, or verapamil hydrochloride.
An intravenous beta-blocker or verapamil hydrochloride is preferred for rapid control.
Digoxin can be added if rate control remains inadequate, and may be particularly useful in those with heart failure.
Conversion to sinus rhythm can be achieved by electrical cardioversion (by cardiac pacing or direct current), pharmacological cardioversion, or catheter ablation.
Compared to AF, electrical cardioversion is more effective in atrial flutter, also requiring less energy.11
If the duration of atrial flutter is unknown, or it has lasted for over 48 hours, cardioversion should not be attempted until fully anticoagulated for at least 3 weeks. If this is not possible, parenteral anticoagulation should be commenced and a left atrial thrombus ruled out immediately before cardioversion. Oral anticoagulation should be given after cardioversion and continued for at least 4 weeks.
Direct current cardioversion is usually the treatment of choice when rapid conversion to sinus rhythm is necessary (eg, when atrial flutter is associated with haemodynamic compromise). Catheter ablation is preferred for the treatment of recurrent atrial flutter.
There is a limited role for anti-arrhythmic drugs as their use is not always successful.
Flecainide acetate or propafenone hydrochloride can slow atrial flutter, resulting in 1:1 conduction to the ventricles, and should therefore be prescribed in conjunction with a ventricular rate controlling drug such as a beta-blocker, diltiazem hydrochloride, or verapamil hydrochloride.
Amiodarone hydrochloride can be used when other drug treatments are contra-indicated or ineffective.
All patients should be assessed for their risk of stroke and the need for thromboprophylaxis; the choice of anticoagulant is based on the same criteria as for atrial fibrillation.
Management also includes the treatment of any underlying conditions, eg, hyperthyroidism, alcoholism, obesity. After the initial episode is terminated and the underlying disease is treated, the patient may not need any further intervention except avoidance of the precipitating factor (eg, alcohol, caffeine).
Catheter radiofrequency ablation
Catheter ablation is suggested as the first-line therapy in patients with atrial flutter and normal or mildly enlarged left atrial size. The success rate of radiofrequency catheter ablation for atrial flutter is 90-95%.12
It has been shown to have a higher success rate, better quality of life, lower occurrence of atrial fibrillation and less need for hospital re-admission when compared with pharmacological treatment.
Typical atrial flutter is amenable to cure with catheter ablation. Atypical flutter is potentially curable with catheter-based techniques but is more difficult.
NICE guidance
NICE has issued guidance on the management of atrial fibrillation (AF), including people with atrial flutter. Of relevance to people with atrial flutter:1
They recommend the use of the CHA2DS2-VASc stroke risk score to assess people at continued risk of arrhythmia recurrence after cardioversion back to sinus rhythm or catheter ablation.
They recommend that if beta-blockers are required, a standard beta-blocker (that is, a beta-blocker other than sotalol) should be used.
The ORBIT bleeding risk score should be used in preference to the HAS-BLED score to determine bleeding risk and to weigh up the risks and benefits of anticoagulation.
In other respects their advice in relation to patients with atrial flutter remains unchanged.
Electrical cardioversion
External electrical cardioversion is safe and effective.
If the atrial flutter has persisted for more than 48 hours then adequate anticoagulation is required before cardioversion to avoid the complication of emboli.
Pharmacological cardioversion
A number of agents are used to try to restore sinus rhythm. Some options include amiodarone, beta-blockers (such as metoprolol, carvedilol), calcium-channel blockers (verapamil, diltiazem), digoxin, Class IA agents (procainamide, quinidine, and disopyramide), and Class IC (flecainide, propafenone).
Ibutilide and dofetilide, which are able to achieve very rapid cardioversion, are not currently available in the UK.
Ventricular rate control
Rate control should not be used as the first-line strategy for people with atrial flutter whose condition is considered suitable for an ablation strategy to restore sinus rhythm .
Rate control is usually more difficult for atrial flutter than for atrial fibrillation. However, rate control is less likely than rhythm control to make the arrhythmia worse.
Ventricular rate control can be achieved with agents that block the AV node. Calcium-channel blockers (eg, verapamil, diltiazem), beta-blockers, digoxin and amiodarone can be used.
Pacemaker
Pacemakers are occasionally used where pharmacological agents and ablation have failed.
In some situations - eg, after cardiac surgery - overdrive atrial pacing may be required for acute control of atrial flutter.
Prevention of thromboembolism
Patients with atrial flutter should be given antithrombotic therapy in the same manner as those with atrial fibrillation. The CHA2DS2-VASc stroke risk score should be used to assess stroke risk and the HAS-BLED score to assess bleeding risk in people with atrial flutter.13 14 See the separate Atrial Fibrillation article for details.
Adequate anticoagulation has been shown to decrease thromboembolic complications in patients with chronic atrial flutter and in patients undergoing cardioversion.
Long-term anticoagulation is therefore advised for patients with persistent or paroxysmal atrial flutter where stroke risk is considered significant when balanced against bleeding risk as per the details in the Atrial Fibrillation article. Briefly, consider anticoagulation where the CHA2DS2-VASc score is 1 or more in men, and 2 or more in women, having taken bleeding risk into account.
After successful catheter ablation, if sinus rhythm is still present, NICE guidance suggests anticoagulation should be continued indefinitely. European guidelines state this question is less clear in the absence of any history of atrial fibrillation.
Cardioversion of atrial flutter presents similar risks to cardioversion of atrial fibrillation and therefore requires similar anticoagulation. See the separate Atrial Fibrillation article.
Complications of atrial flutter
Back to contentsHeart failure; acute atrial flutter can impair cardiac function, lower blood pressure, and initiate myocardial ischaemia.
Thromboembolism (transient ischaemic attacks and stroke). Systemic embolism is less commonly associated with atrial flutter than with atrial fibrillation, but is still a significant risk. One study showed the annual incidence of ischaemic stroke to be 1.38%.15
Tachycardia-induced cardiomyopathy.
Persistent untreated atrial flutter can become chronic atrial fibrillation.
Prognosis
Back to contentsAtrial flutter leads to an increased overall mortality.
It often converts within one week to normal sinus rhythm or atrial fibrillation but can occasionally persist for weeks or months.
Prevention of atrial flutter
Back to contentsEffective prevention and management of potential causes - eg, hypertension, obesity, excessive alcohol intake, hyperthyroidism and obstructive sleep apnoea.
Further reading and references
- Markowitz SM, Thomas G, Liu CF, et al; Atrial Tachycardias and Atypical Atrial Flutters: Mechanisms and Approaches to Ablation. Arrhythm Electrophysiol Rev. 2019 Mar;8(2):131-137. doi: 10.15420/aer.2019.17.2.
- Diamant MJ, Andrade JG, Virani SA, et al; Heart failure and atrial flutter: a systematic review of current knowledge and practices. ESC Heart Fail. 2021 Dec;8(6):4484-4496. doi: 10.1002/ehf2.13526. Epub 2021 Sep 10.
- Atrial fibrillation: diagnosis and management; NICE guideline (April 2021 - last updated June 2021)
- Katritsis DG, Boriani G, Cosio FG, et al; European Heart Rhythm Association (EHRA) consensus document on the management of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiologia (SOLAECE). Europace. 2017 Mar 1;19(3):465-511. doi: 10.1093/europace/euw301.
- Page RL, Joglar JA, Caldwell MA, et al; 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016 Apr 5;67(13):e27-e115. doi: 10.1016/j.jacc.2015.08.856. Epub 2015 Sep 24.
- Rodriguez Ziccardi M, Maani CV; Atrial Flutter. StatPearls Publishing; Dec 2022.
- Bun SS, Latcu DG, Marchlinski F, et al; Atrial flutter: more than just one of a kind. Eur Heart J. 2015 Sep 14;36(35):2356-63. doi: 10.1093/eurheartj/ehv118. Epub 2015 Apr 2.
- Shah SR, Luu SW, Calestino M, et al; Management of atrial fibrillation-flutter: uptodate guideline paper on the current evidence. J Community Hosp Intern Med Perspect. 2018 Oct 15;8(5):269-275. doi: 10.1080/20009666.2018.1514932. eCollection 2018.
- Schmidt M, Christiansen CF, Mehnert F, et al; Non-steroidal anti-inflammatory drug use and risk of atrial fibrillation or flutter: population based case-control study. BMJ. 2011 Jul 4;343:d3450. doi: 10.1136/bmj.d3450.
- Liu G, Yan YP, Zheng XX, et al; Meta-analysis of nonsteroidal anti-inflammatory drug use and risk of atrial fibrillation. Am J Cardiol. 2014 Nov 15;114(10):1523-9. doi: 10.1016/j.amjcard.2014.08.015. Epub 2014 Aug 27.
- Atrial Flutter with 2:1 AV conduction; ECG library
- British National Formulary (BNF); NICE Evidence Services (UK access only)
- Brandes A, Crijns HJGM, Rienstra M, et al; Cardioversion of atrial fibrillation and atrial flutter revisited: current evidence and practical guidance for a common procedure. Europace. 2020 Aug 1;22(8):1149-1161. doi: 10.1093/europace/euaa057.
- Lee G, Sanders P, Kalman JM; Catheter ablation of atrial arrhythmias: state of the art. Lancet. 2012 Oct 27;380(9852):1509-19. doi: 10.1016/S0140-6736(12)61463-9.
- CHA2DS2-VASc Score - Stroke Risk in Atrial Fibrillation; MDCalc Online Calculator
- HAS-BLED Score for Major Bleeding Risk; MDCalc On Line Calculator
- Al-Kawaz M, Omran SS, Parikh NS, et al; Comparative Risks of Ischemic Stroke in Atrial Flutter versus Atrial Fibrillation. J Stroke Cerebrovasc Dis. 2018 Apr;27(4):839-844. doi: 10.1016/j.jstrokecerebrovasdis.2017.10.025. Epub 2017 Dec 6.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 4 Feb 2029
6 Feb 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free