Genitourinary history and examination - male
Peer reviewed by Dr Philippa Vincent, MRCGPLast updated by Dr Hayley Willacy, FRCGP Last updated 27 Jan 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Despite the increasingly widespread use of imaging of the urinary tract, a thorough history and examination are essential in the assessment of all patients presenting with genitourinary symptoms.
The presentation must be assessed in the context of the age, gender and past medical and surgical history of the patient. Urinary symptoms may not be indicative of urological abnormality but may have other causes such as frequency of micturition in anxiety or urinary symptoms caused by neurological disease.
The following account will both list important items as an aide-mémoire and provide diagnostic tips and suggestions for history and examination. Paediatric genitourinary history and examination are referred to and important aspects particular to developing children are outlined. The separate partner article Genitourinary history and examination -female covers detail specific to female patients.
Continue reading below
Male genitourinary history
Care should again be taken to ensure privacy and comfort for both history and examination. Establish confidence and rapport. Allow the patient to describe their complaint or problem. It may be appropriate and necessary to ask details about sexual and psychosexual history. Sign-posting these intimate and personal questions and explaining their importance can facilitate better co-operation from the historian. Specific, closed questioning may be appropriate. Significant symptoms and history are described below.
Urinary symptoms
The history of urinary symptoms should cover the following questions:
Is there dysuria?
Is there frequency of micturition? Is there any nocturia?
Is there any terminal dribbling of micturition?
Is there hesitancy of micturition?
How full is the urinary stream?
Have symptoms developed gradually or suddenly?
Is there any incontinence or urgency of micturition? There may be stress incontinence, detrusor instability, detrusor underactivity or urethral obstruction.
Abnormalities of micturition in men are most often caused by prostatism (see also the separate articles Benign prostatic hyperplasia and Prostate cancer). This leads to hesitancy, reduced strength of urine flow and terminal dribbling.
Symptoms of prostatism can be assessed by using the International Prostate Symptom Score (I-PSS) but this does not give an indication of the degree of prostate size or nature of underlying pathology. Complete obstruction may lead to complete inability to pass urine, or to overflow incontinence.
Urethral discharge
This is a relatively common presenting symptom. Ask about:
Dysuria.
Possible exposure to sexually transmitted infections:
When was contact?
Has the partner had symptoms?
Are there any other symptoms? - for example, with reactive arthritis:
Joint pains.
Eye inflammation, pain or grittiness.
Gastrointestinal symptoms.
Testicular pain
This can be an intense pain. Enquiry should be made about:
Trauma.
Speed of onset.
Association with other conditions (for example, mumps).
Other urinary symptoms, such as dysuria or urethral discharge.
Possible causes include trauma, infection, torsion and epididymitis.
Genital ulcers
Genital ulcers are likely to be caused by sexually transmitted infection. Enquiry should be made with this in mind.
Impotence
Impotence covers a number of different conditions and causes. Consider:
Emotional and psychological factors.
Drugs and alcohol.
Any association with other relevant diseases (diabetes mellitus, neurological disease, cardiovascular disease).
Whether there is:
Subfertility
This may be primary (no conception) or secondary (past conception). Subfertility history should cover:
Conception history.
Length of subfertility.
Sexual history:
Timing and frequency of intercourse.
Impotence and ejaculation.
Medication history.
Medical history:
Conditions affecting erectile function.
Any chemotherapy or cancer treatment.
History of sexual development.
Other symptoms
Important examples include:
Loin pain; urinary calculi can cause ureteric obstruction and lead to severe loin pain which radiates to the symphysis pubis or testis. The sudden onset of pain in renal colic or acute urinary retention contrasts with the gradual build-up of pain from a renal tumour or the slow development of urine symptoms from outflow obstruction. Ask about associated features such as pain, haematuria or incontinence.
Systemic symptoms of acute kidney injury or chronic kidney disease - eg, anorexia, vomiting, fatigue, pruritus and peripheral oedema.
Recent onset of back pain in an elderly patient may be indicative of prostate cancer with bone metastases.
Some patients have no symptoms but abnormalities are discovered on measuring blood pressure or abnormalities on routine urinalysis, renal function or serum biochemistry.
Occupational history
Exposure to chemical carcinogens such as 2-naphthylamine or benzidine in the chemical or rubber industries may induce bladder cancer many years later.
Foreign travel
Travel to Egypt or Africa may result in exposure to schistosomiasis.
Dehydration during a holiday in a hot climate may lead to the development of kidney stones.
Family history
A family history of kidney failure or polycystic kidney disease may be relevant to the underlying problem.
Past medical history
Neurological diseases may cause abnormal bladder function - eg, Parkinson's disease, multiple sclerosis or cerebrovascular disease.
Any history of kidney disease, hypertension, diabetes, gout or past back injury may also be relevant. Abdominal or pelvic surgery can cause denervation injury to the bladder.
Previous surgery - eg, for prostatic hypertrophy.
Ureteric injury may occur in abdominal operations.
Medication history
A full current and past medication history is important.
Past history of analgesic abuse may be a cause of kidney failure.
Dosages of some drugs may need to be adjusted or stopped in kidney failure.
Male genitourinary examination
Back to contentsThe genitourinary examination should incorporate a general examination and an abdominal examination.
General examination
General sexual development and secondary sexual characteristics.
Note whether there is evidence of gynaecomastia.
Establish whether the patient is distressed due to pain or appearing unwell, suggesting systemic illness and possibly kidney failure.
Note whether there is evidence of liver disease or thyroid disease.
Note whether there is evidence of anaemia.
All patients with urological symptoms should have their blood pressure measured.
Signs of dehydration such as a dry mouth and tongue may indicate kidney failure or polyuria associated with diabetes.
Lymphadenopathy; lymph nodes may be enlarged due to metastatic spread from any urological cancer.
Abdominal examination
Abdomen may be distended due to large polycystic kidneys or ascites due to nephritic syndrome or nephrotic syndrome. Palpate for an enlarged bladder or an abdominal aortic aneurysm.
The kidneys are examined by bimanual examination with a hand posteriorly lifting up the kidney towards the examining abdominally placed hand.
Tenderness over the kidney should be tested by gentle pressure over the renal angle.
Palpation for renal enlargement or masses. An enlarged kidney usually bulges forwards. In polycystic kidney disease, there may also be hepatomegaly from hepatic cysts.
Percussion for the presence of ascites (shifting dullness) and for an enlarged bladder.
Hernias and hernial orifices.
Auscultation for a renal bruit in renal artery stenosis (heard above the umbilicus, 2 cm to the left or right of the midline and also in both flanks with the patient sitting up).
Penis
The size and shape variation of the normal penis is quite wide. Examination should involve inspection and palpation of:
Prepuce, glans and foreskin - for example, to exclude a phimosis and signs of hypospadias.
The skin should be examined for ulcers and rashes.
The shaft of the penis is examined for plaques of Peyronie's disease.
Urethral discharge.
Scrotum
Inspect scrotal skin.
Palpate testes:
The testes should be equal in size, smooth and relatively firm.
Size/volume can be estimated using an orchidometer (see image).
Orchidometer
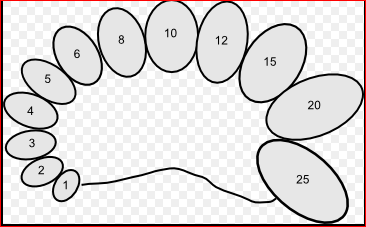
Filip em (Own work) CC BY-SA 3.0, via Wikimedia Commons
Small firm testes suggest hypogonadism or testicular atrophy.
Absence of a testis may indicate previous excision, undescended or retractile.
Identify scrotal swellings:
Determine whether it is possible to get above the swelling. With the patient standing, if it is not possible to define the upper border of a mass in the scrotum then it is likely to be an inguinal hernia.
Note whether the swelling is solid or cystic. Note whether there is a hydrocele, varicocele or epididymal cyst. Testing for translucency with a torch will determine whether the mass is cystic or a solid mass. Likely diagnoses are:
Attached to the testis:
Solid (non-translucent): testicular tumour.
Cystic (translucent): hydrocele.
Separate from the testis:
Solid (non-translucent): chronic epididymitis.
Cystic (translucent): epididymal cyst.
Examine the groin and lymphatics.
Prostate
This is examined by rectal examination to assess:
Size.
Consistency.
Any swelling. A hard lump in either or both lobes suggests a cancer and a biopsy is needed to obtain histological proof.
Presence of the medial sulcus.
Any tenderness.
Neurological examination
Dermatome sensory loss of the perineum or lower limbs and lower limb motor dysfunction suggest possible spinal cord or root pathology.
Trauma or compression of the spinal cord may cause urinary retention if acute, or urgency of micturition if a more chronic process.
Acute compression of either the spinal cord or cauda equina may cause bladder and bowel dysfunction and are both neurosurgical emergencies, requiring urgent treatment to prevent irreversible neurological damage.
Continue reading below
The genitourinary history and examination in children
Back to contentsThis should involve parents and be done sensitively and carefully. Genitourinary disease in children is more varied and complex (for example, ambiguous genitalia) than in adults. Developmental aspects may be important in both the history and examination. Aspects of this are covered in other separate articles - for example, Normal and abnormal puberty, Paediatric history and Paediatric examination.
Urinary tract infection in children is an important condition which should be diagnosed early and treated adequately if renal scarring is to be avoided in later life.
See the separate article Urinary tract infection in children for more details.
History
In general medical practice the history will usually focus on presenting complaints but, in babies particularly, will involve screening for disease as well. Some of the history overlaps with that for adults but an understanding of normal growth and development, particularly of normal pubertal development, is essential in paediatric practice. Child abuse may present with genitourinary symptoms. When child abuse is suspected the correct procedures should be followed with referral for further assessment and examination.
Examination
Again this will be conducted with a good understanding of normal growth and pubertal development. Sensitive handling is essential and, broadly speaking, intrusive and intimate examinations are rarely appropriate. Ultrasound and other investigative techniques can now be used to assess internal organs. Inspection is often all that is required.
Further reading and references
- Whitfield HN; ABC of urology: Urological evaluation. BMJ. 2006 Aug 26;333(7565):432-5.
- Urological cancers - recognition and referral; NICE CKS, February 2021 (UK access only)
- Urinary tract infection in under 16s: diagnosis and management; NICE guideline (July 2022)
- Sexually Transmitted Infections in Primary Care; Royal College of General Practitioners and British Association for Sexual Health and HIV (2013)
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 26 Jan 2028
27 Jan 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free