Nasal polyps
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 14 Sept 2022
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find the Nasal polyps article more useful, or one of our other health articles.
In this article:
See also the separate Rhinitis and Nasal Obstruction, Allergic Rhinitis, Non-allergic Rhinitis and Sinusitis articles.
Continue reading below
What are nasal polyps?
Nasal polyps are lesions arising from the nasal mucosa, occurring at any site in the nasal cavity or paranasal sinuses but most frequently seen in the clefts of the middle meatus. Nasal polyps can be considered as part of the spectrum of chronic rhinosinusitis. They must be distinguished from more serious pathology such as nasal tumours, particularly if they are unilateral. If they occur in children, cystic fibrosis testing is merited.
How common are nasal polyps? (Epidemiology)
Back to contentsThe population prevalence is reported as around 4%, with no racial predilection.1 The male-to-female ratio is approximately 2:1.
Continue reading below
What causes nasal polyps? (Aetiology)
Back to contentsThe exact pathogenesis is not known. Nasal polyps have been linked with chronic inflammation such as in chronic rhinosinusitis and vasculitis. Superantigens produced by Staphylococcus aureus may play a role.2 Polyps usually start close to the ostiomeatal complex (the sinus ostia) of the nasopharynx.
Histological examination reveals that in most polyps there are sac-like entities with an eosinophil-rich oedematous wall; their poor blood supply gives them a pale appearance. Over time, they may become fleshy and reddened due to squamous metaplasia. Benign and malignant nasal tumours can mimic or co-exist with nasal polyps.
Nasal polyps can be classified as eosinophil-rich (the most common type in the UK), infective, or due to other causes.
Recent research has identified differences in aetiology between chronic rhinitis with polyps and chronic rhinitis without polyps.3 Patients presenting with chronic rhinitis with polyps are found to have oedema of the nasal mucosa, low T regulatory cell activity and low levels of beta-tissue growth factor. Inflammatory mediators such as cytokines and chemokines may also have a role.4 The opposite picture is seen with patients who have chronic rhinitis without polyps. Considerable variation exists globally. Different factors may be involved, depending on factors such as geographical location, culture and differences in bacterial colonisation.2
Associations1
Aspirin sensitivity (see 'Aspirin-sensitive nasal polyposis', below).
Cystic fibrosis (particularly nasal polyps in children).
Allergic fungal sinusitis (rare in the UK but more common in warmer areas).
Nasal polyps are not associated with allergy.
Nasal polyps presentation
Back to contentsSymptoms
Patients may have a history of recurring acute or chronic sinusitis. Symptoms depend on the size of the polyp (small polyps may be asymptomatic) and include:
Nasal airway obstruction.
Nasal discharge:
Watery anterior rhinorrhoea, sneezing, postnasal drainage.
Green secretions suggest infection (due to a polyp blocking the sinus ostia).
Unilateral, blood-tinged secretion suggests a tumour, foreign body, nose picking, or misapplication of nasal spray.
Dull headaches.
Snoring and obstructive sleep symptoms.
Hyposmia or anosmia (decreased smell) and reduced taste.
Examination
A nasal speculum will allow visualisation up until the anterior edge of the middle turbinate (in good conditions). Misting of the speculum helps confirm good airflow. The nose may be examined with an aural speculum if nasal equipment is lacking.
Nasal polyps can be distinguished from the inferior turbinate by their lack of sensitivity, their yellowish-grey colour and by your ability to get between them and the side wall of the nose.
The nasal bridge may be widened in patients with nasal polyps; it may be depressed in patients with granulomatosis with polyangiitis.
Using an aural speculum, look for single, or clusters of, grape-like structures. Very large polyps may grow down into the oropharynx and can be visualised with a tongue depressor. Smaller polyps may not be visible without nasendoscopy.
Decongestants and local anaesthesia may help examination.
Continue reading below
Differential diagnosis
Back to contentsNasal polyps tend to be bilateral. With unilateral lesions, suspect a tumour (and in children, rule out an encephalocele).
Foreign body - particularly if there is unilateral, blood-tinged discharge in young children.
Chronic rhinosinusitis without polyps.
Allergic fungal rhinosinusitis.
Tumours, benign and malignant - eg, nasopharyngeal carcinoma, dermoid tumour and others.
Be aware of associated conditions (see 'Associations', above), including cystic fibrosis in children with nasal polyps.
Investigations
Back to contentsENT investigations
Rigid or flexible endoscopy (rhinoscopy) carried out by specialists - this allows localisation and determination of the extent of the polyps.
Plain X-ray films are of limited value - they are not recommended in this scenario.
CT scans are helpful - they should be reserved for patients failing medical therapy or those with atypical or severe disease.
Investigation for an underlying cause
Investigation of underlying chronic rhinosinusitis may be appropriate.
Patients with severe or recurrent polypoid rhinosinusitis merit investigations for aspirin sensitivity, allergic fungal rhinosinusitis or Churg-Strauss syndrome.
Nasal polyps treatment and management
Back to contentsThe evidence relating to the effectiveness of different types of surgery versus medical treatment for adults with chronic rhinosinusitis with nasal polyps is of low quality and further research is needed, including into new therapies such as biologic drugs.5 3
General principles
Medical management with topical and possibly systemic corticosteroids is usually considered the initial treatment of choice, with endoscopic sinus surgery reserved for those patients who fail to improve6 .
Referral
Unilateral polyps may be a sign of malignancy and should always be referred to ENT.
Children with nasal polyps should be referred to be tested for cystic fibrosis.
Review for associated/underlying disease (see 'Investigations, above) - eg, covert asthma and aspirin sensitivity.
As there is no single causative factor, treatment targets the underlying inflammatory process.
Medical management is first-line, unless the nature of the polyp is uncertain (eg, suspected malignancy).
Patients should be educated regarding the recurring nature of this problem.
Drugs
Topical corticosteroids
These are the the mainstay of medical management: in most patients, they improve symptoms and reduce recurrence after surgery.
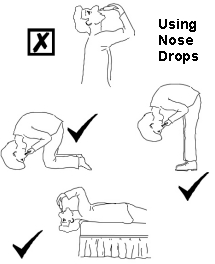
Nasal drops are preferred to sprays for nasal polyps. They should be used in the 'head upside down' position (see diagram).
Systemic absorption is negligible with mometasone and fluticasone, high for betamethasone and dexamethasone and modest for the remainder.
Fluticasone, mometasone and budesonide do not seem to affect children's growth - unlike beclometasone. However, take into account other steroid use (eg, chest and skin). Growth monitoring is advised for children.
Patients with glaucoma should be monitored more closely.
The pre-operative administration of steroids in patients with nasal polyps has been shown to reduce intraoperative bleeding.7
Diagram showing how to use nose drops
Other possible drugs
Antihistamine (if allergic rhinitis is present).
Nasal douche (saline) may be of moderate benefit, especially when combined with other treatments (eg, steroids, antibiotics).
Leukotriene receptor antagonists may be beneficial for some patients.8
Systemic corticosteroids - long-term use is not advised due to side-effects but a short course immediately after surgery has also been shown to have long-term benefits.9
There is insufficient evidence to support the use of antibiotics. Even patients with chronic rhinosinusitis with nasal polyps do not usually respond to antibiotics.2
Other treatments
Steroid injection of polyps has been used but there are safety concerns.10
Surgical treatment
The gold standard treatment is functional (as in restoring function) endoscopic sinus surgery (FESS). This has been found to be as safe and as effective as more invasive procedures.6 Accepted practice is to reserve surgery for medically refractory cases but there are some authorities who hold that performing such a procedure early in the condition reduces exposure to the adverse effects of medical treatment (eg, antibiotics, topical steroids).11
Complications
Back to contentsSevere complications are uncommon. Complications include:
Acute bacterial sinusitis - with potential complications of intracranial infections (eg, meningitis); cavernous sinus thrombosis, orbital complications (periorbital and orbital cellulitis, orbital abscess); subperiosteal abscess.
Sleep disruption.
May contribute to symptoms of asthma.
Rarely, massive polyps (such as those occurring in cystic fibrosis or with allergic fungal sinusitis) can lead to craniofacial structural abnormalities with resulting proptosis, hypertelorism (increased interorbital distance) and diplopia.
Prognosis
Back to contentsThere is no single curative treatment and recurrence is common, including after surgery.
Aspirin-sensitive nasal polyposis
Back to contentsAspirin sensitivity associated with nasal polyposis, rhinosinusitis and asthma is called asthma-exacerbated respiratory disease (AERD). Hypersensitivity to aspirin or other non-steroidal anti-inflammatory drug (NSAID) is associated with a more severe and protracted course of nasal polyps and a distinct pattern of cellular, biochemical and molecular markers of inflammation. 60-70% of patients with aspirin-sensitive asthma have nasal polyps compared to 10% of asthma patients who are not sensitive to aspirin.12
Presentation
Typically occurring in the third and fourth decades of life; more common in females and in non-atopics.
Ingestion of aspirin or an NSAID induces a reproducible reaction within 20-120 minutes:
In any individual the form of the reaction is consistent.
Any combination of symptoms may occur, including systemic upset with facial flushing, perspiration and intense lethargy, rhinorrhoea, nasal congestion, conjunctivitis, respiratory symptoms (cough and bronchospasm) and gastrointestinal symptoms.
A severe reaction can include shock and respiratory arrest.
Diagnosis
Aspirin sensitivity should be suspected in patients with severe or recurrent nasal polyps and intrinsic asthma. The diagnosis relies on either a clear history of two aspirin/NSAID-induced reactions or by aspirin challenge (nasal, inhaled or oral).
Aspirin challenge: this uses lysine aspirin (a soluble form of aspirin). Nasal challenge, if negative, should be followed by graduated oral challenge. These tests should be carried out by doctors with appropriate experience and with full resuscitation facilities readily available.
Management of aspirin sensitivity13
Patients should be warned to avoid all drugs with cyclo-oxygenase-1 (COX-1) inhibitory activity. Selective COX-2 inhibitors appear to be safe but it is suggested that the first dose should be administered in hospital under direct observation with monitoring for two hours and resuscitation facilities available.
Paracetamol is usually (not always) tolerated; single doses of ≤500 mg are safe in 94% of patients.
A diet avoiding preservatives, additives and high salicylate foods may be helpful (for some patients in open studies).
Aspirin desensitisation can be carried out in a hospital setting.
Surgery is less successful (compared with aspirin-tolerant patients).
Further reading and references
- Rajguru R; Nasal polyposis: current trends. Indian J Otolaryngol Head Neck Surg. 2014 Jan;66(Suppl 1):16-21. doi: 10.1007/s12070-011-0427-z. Epub 2011 Dec 29.
- Cheng KJ, Wang SQ, Xu YY; Different roles of Staphylococcus aureus enterotoxin in different subtypes of nasal polyps. Exp Ther Med. 2017 Jan;13(1):321-326. doi: 10.3892/etm.2016.3951. Epub 2016 Dec 2.
- Dennis SK, Lam K, Luong A; A Review of Classification Schemes for Chronic Rhinosinusitis with Nasal Polyposis Endotypes. Laryngoscope Investig Otolaryngol. 2016 Oct;1(5):130-134. Epub 2016 Sep 9.
- Chen S, Zhou A, Emmanuel B, et al; Systematic literature review of the epidemiology and clinical burden of chronic rhinosinusitis with nasal polyposis. Curr Med Res Opin. 2020 Nov;36(11):1897-1911. doi: 10.1080/03007995.2020.1815682. Epub 2020 Sep 25.
- Rimmer J, Fokkens W, Chong LY, et al; Surgical versus medical interventions for chronic rhinosinusitis with nasal polyps. Cochrane Database Syst Rev. 2014;(12):CD006991. doi: 10.1002/14651858.CD006991.pub2. Epub 2014 Dec 1.
- Jafari A, DeConde AS; Outcomes in Medical and Surgical Treatment of Nasal Polyps. Adv Otorhinolaryngol. 2016;79:158-67. doi: 10.1159/000445155. Epub 2016 Jul 28.
- Hwang SH, Seo JH, Joo YH, et al; Does the Preoperative Administration of Steroids Reduce Intraoperative Bleeding during Endoscopic Surgery of Nasal Polyps? Otolaryngol Head Neck Surg. 2016 Dec;155(6):949-955. Epub 2016 Aug 23.
- Wu X, Hong H, Zuo K, et al; Expression of leukotriene and its receptors in eosinophilic chronic rhinosinusitis with nasal polyps. Int Forum Allergy Rhinol. 2016 Jan;6(1):75-81. doi: 10.1002/alr.21625. Epub 2015 Sep 1.
- Jaksha AF, Weitzel EK, Laury AM; Recent advances in the surgical management of rhinosinusitis. F1000Res. 2016 Sep 26;5. pii: F1000 Faculty Rev-2377. eCollection 2016.
- Antunes MB, Becker SS; The role of local steroid injection for nasal polyposis. Curr Allergy Asthma Rep. 2010 May;10(3):175-80. doi: 10.1007/s11882-010-0104-4.
- Fokkens WJ, Lund VJ, Mullol J, et al; European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinol Suppl. 2012 Mar;(23)
- London NR Jr, Reh DD; Differential Diagnosis of Chronic Rhinosinusitis with Nasal Polyps. Adv Otorhinolaryngol. 2016;79:1-12. doi: 10.1159/000444957. Epub 2016 Jul 28.
- Simon RA, Dazy KM, Waldram JD; Update on aspirin desensitization for chronic rhinosinusitis with polyps in aspirin-exacerbated respiratory disease (AERD). Curr Allergy Asthma Rep. 2015 Mar;15(3):508. doi: 10.1007/s11882-014-0508-7.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 13 Sept 2027
14 Sept 2022 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free