Serotonin syndrome
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 25 Jan 2024
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
Medical Professionals
Professional Reference articles are designed for health professionals to use. They are written by UK doctors and based on research evidence, UK and European Guidelines. You may find one of our health articles more useful.
In this article:
Continue reading below
What is serotonin syndrome?
Serotonin syndrome (SS) - also called serotonin toxicity - is a potentially life-threatening drug-induced condition caused by too much serotonin in the synapses of the brain.
The condition presents with a combination of neuromuscular, autonomic and mental state symptoms. Most cases involve two drugs that increase serotonin in different ways or an overdose of one serotonin-elevating drug.
The most common implicated drugs are monoamine-oxidase inhibitors (MAOIs), serotonin-norepinephrine reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs); the list of potential causes includes certain herbal remedies and illicit drugs.1
SS can occur as a consequence of normal therapeutic drug use, self-poisoning or drug interactions.2 There is a wide spectrum of illness ranging from barely noticeable minor symptoms such as tremor, through to life-threatening acute illness.3
The syndrome is not widely recognised amongst clinicians. A failure to appreciate the syndrome means that mild cases may be overlooked; continuing or increasing the offending drug can cause progression to severe illness.3
It is underdiagnosed due to the heterogeneity of its presentation, because there are evolving diagnostic criteria, a lack of awareness amongst prescribers and mistaking of the symptoms for features of a pre-existing psychiatric illness. It should not be confused with the neuroleptic malignant syndrome.4
There is some controversy about the pharmacology of SS.5 There is evidence that it is activation of the 5-HT2A receptor that is required for serious SS rather than 5-HT1A receptors.6 Accordingly, there has been much scientific criticism of government agency warnings of a serotonin syndrome risk from co-prescriptions of triptans and SSRIs; while cases of SS have been reported, the risk seems to be very low.7
How common is serotonin syndrome? (Epidemiology)
Incidence is unclear due to the extent of underdiagnosis.
Post-marketing surveillance studies on nefazodone (no longer licensed but unlicensed preparations are still available) suggest an incidence of 0.4 cases per 1,000 patient-months of treatment.3
It is estimated that 14-16% of those who take overdoses of SSRIs display features of the syndrome.8
Deaths with SSRI overdose are associated with combinations of other medications or illicit substances.
Risk factors
Use of serotonergic agents is the risk factor for SS. SS may be produced by large doses/overdose of a single drug or by combinations of drugs. The most common causative combinations include an MAOI.6
Drugs implicated in SS include:
Antidepressants: SSRI, SNRI, TCA, MAOI, St John's wort, lithium.
Analgesics: tramadol, pethidine, fentanyl, dextromethorphan (in OTC cough remedies).
Antiemetics: odansetron, metoclopramide.
Recreational: cocaine, MDMA, amphetamine, LSD.
Others: eg, linezolid, tryptophan, buspirone, methylthioninium chloride (methylene blue).
It is worth checking with a reputable formulary or toxicologist whether there are any known drug interactions causing the syndrome, where it is suspected in an individual taking serotonergic agents.9
Although the epidemiology of SS has yet to be extensively studied, the combination of age and comorbidities may increase the risk.10
Continue reading below
Serotonin syndrome symptoms (presentation)
SS is characterised by the presence of a triad of:1
Autonomic hyperactivity
Neuromuscular abnormality
Mental status changes
Not all of these features are present in all cases.
The diagnosis is likely only in the setting of starting or increasing the dose (or, indeed overdose) of a potent serotonergic drug, or shortly after a second serotonergic drug is added leading to a drug interaction.6
Symptoms usually occur within six hours of taking the provoking drug. Mild cases may go unrecognised. Tremor, akathisia and diarrhoea are early features. Agitation, hypervigilance and pressured speech may occur. Acute delirium is a feature of severe cases.
Examination
Examination should seek signs of:
1. Autonomic disturbance - namely:
Hypertension.
Tachycardia.
Hyperthermia.
Hyperactive bowel sounds.
Mydriasis.
Excessive sweating.
2. Neuromuscular dysfunction - namely:
Tremor.
Clonus - inducible or spontaneous.
Ocular clonus.
Hypertonicity.
Hyperreflexia (this symptom can be masked if there is severe muscle rigidity).
3. Altered mental state - namely:
Anxiety.
Agitation.
Confusion.
Coma.
The severity of symptoms ranges from mild to life-threatening. Progression from restlessness, diaphoresis, and neuromuscular dysfunction to confusion, convulsions and death has been described.
Skin appearance should be normal in SS, a fact that helps to differentiate it from two similar diagnoses (see below). The presence of muscular hypertonicity, sustained clonus and hyperthermia (which may rise as high as 41°C) indicate severe disease.
A neonatal behavioural syndrome - also called poor neonatal adaptation syndrome - can also occur as a result of maternal SSRI use during late pregnancy.11
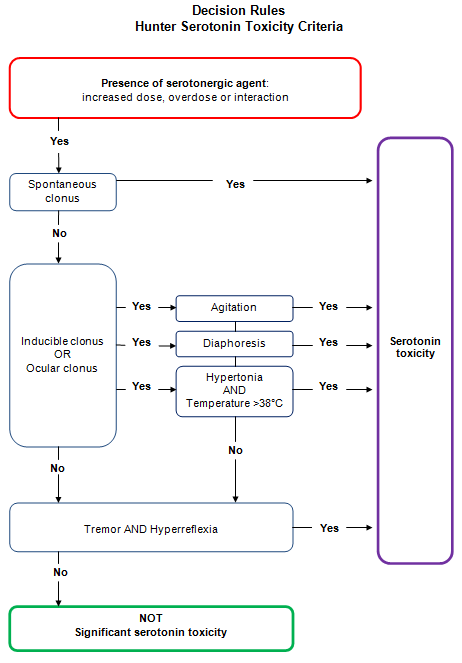
The Hunter serotonin toxicity criteria
These criteria have been developed (following a review of a large series of patients with serotogenic drug overdose) to confirm the diagnosis of moderate or severe toxicity.4
Hunter Criteria
Continue reading below
Differential diagnosis
Anticholinergic poisoning (normal reflexes, dry mouth, hot and dry skin, absent bowel sounds).
Malignant hyperthermia (caused by inhalational anaesthetics; mottled and patchily cyanotic skin, severe rigidity and hyporeflexia).
Neuroleptic malignant syndrome (slow-onset idiopathic reaction to dopamine antagonists, with bradykinesia and 'lead-pipe' muscular rigidity).
Other poisoning.
Dystonia.
Recreational drug toxicity, especially amphetamines/cocaine (many features of their toxicity are due to serotonergic effects).
Withdrawal syndromes.
Wernicke's encephalopathy.
Investigations
There are no specific confirmatory investigations - the diagnosis is clinical.
Check U&Es and creatine kinase to look for evidence of rhabdomyolysis and consequent renal impairment.
Toxicology screen, particularly for agents likely to be responsible.
FBC and blood culture/microbiological samples can suggest alternative causes of fever.
LFTs.
CXR if respiratory complications.
CT scanning of the head for patients with trauma, seizures, hypertension or focal neurology.
Lumbar puncture for patients with fever and altered mental state.
Serotonin syndrome treatment
If SS is suspected then the likely causative drug(s) should be stopped. Refer patients with severe symptoms or patients who have ingested an MAOI and an SSRI to the hospital, as their condition can worsen quickly.
Once SS has resolved, try other drugs or restart low doses slowly, and rule out other contributing drugs such as OTC medications or illicit drugs. For most patients who experience serotonin-mediated side-effects, appropriate changes to their medications will manage symptoms and prevent toxicity.1
In all cases the most important step is to remove the offending agent or interacting drugs. In cases of recent ingestion/large overdose, activated charcoal may help to prevent absorption. Supportive measures such as IV fluids and control of agitation with benzodiazepines are also used.
Mild cases usually resolve within 24 hours of discontinuation and may need supportive measures only. Beware of drugs with long half-lives or active metabolic breakdown products (for example, fluoxetine), where it may take longer.
Moderately severe cases should have cardiovascular and thermal disturbances corrected and receive 5-HT2A antagonists such as cyproheptadine (as yet there is no definitive evidence for its efficacy).
Severe cases need aggressive treatment and intensive care with early sedation, neuromuscular paralysis and ventilatory support.
In the UK, advice for health professionals is available from the Toxbase® website.
Complications
Hyperthermia can lead to metabolic acidosis, rhabdomyolysis, acute kidney injury and disseminated intravascular coagulation. Thermal disturbance should be aggressively managed. Any patient with a temperature over 40.5°C should be managed with:
Paralysis and ventilation.
Ice bath immersion/ice packs if not responsive (to prevent disseminated intravascular coagulation and organ failure).
Antipyretic agents have no role, as hyperthermia is due to muscular activity rather than hypothalamic mechanisms. Chlorpromazine may be used to treat agitation and hyperthermia.Seizures.
Aspiration pneumonia.
Respiratory failure.
Prognosis
If patients recover from an acute episode and avoid provoking agents then the outlook is good. Most deaths occur within the first 24 hours.
Preventing serotonin syndrome
Caution in the prescription of serotonergic agents. All patients starting SSRIs should be counselled about:
Potential interactions (including OTC and 'herbal' medication).
The symptoms of serotonin toxicity and SS.
Improved knowledge amongst the medical community. Do not prescribe an SSRI together with an MAOI. Particular care should be taken when changing SSRIs or prescribing more than one antidepressant.
Improved pharmacogenetic understanding to identify those at increased risk.
Adequate post-marketing surveillance of new serotonergic therapies.
Further reading and references
- Foong AL, Grindrod KA, Patel T, et al; Demystifying serotonin syndrome (or serotonin toxicity). Can Fam Physician. 2018 Oct;64(10):720-727.
- Dvir Y, Smallwood P; Serotonin syndrome: a complex but easily avoidable condition. Gen Hosp Psychiatry. 2008 May-Jun;30(3):284-7.
- Boyer EW, Shannon M; The serotonin syndrome. N Engl J Med. 2005 Mar 17;352(11):1112-20.
- Dunkley EJ, Isbister GK, Sibbritt D, et al; The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003 Sep;96(9):635-42.
- Ken Gillman P; Triptans, Serotonin Agonists, and Serotonin Syndrome (Serotonin Toxicity): A Headache. 2009 Nov 17.
- Buckley NA, Dawson AH, Isbister GK; Serotonin syndrome. BMJ. 2014 Feb 19;348:g1626. doi: 10.1136/bmj.g1626.
- Jin G, Stokes P; Drug interaction between a selective serotonin reuptake inhibitor and a triptan leading to serotonin toxicity: a case report and review of the literature. J Med Case Rep. 2021 Jul 26;15(1):371. doi: 10.1186/s13256-021-02946-8.
- Isbister GK, Buckley NA; The pathophysiology of serotonin toxicity in animals and humans: implications for diagnosis and treatment. Clin Neuropharmacol. 2005 Sep-Oct;28(5):205-14.
- Houlihan DJ; Serotonin syndrome resulting from coadministration of tramadol, venlafaxine, and mirtazapine. Ann Pharmacother. 2004 Mar;38(3):411-3. Epub 2004 Jan 23.
- Wang RZ, Vashistha V, Kaur S, et al; Serotonin syndrome: Preventing, recognizing, and treating it. Cleve Clin J Med. 2016 Nov;83(11):810-817. doi: 10.3949/ccjm.83a.15129.
- Levy R, Naymark S; Case 1: A newborn in distress. Paediatr Child Health. 2011 Nov;16(9):557-8. doi: 10.1093/pch/16.9.557.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 23 Jan 2029
25 Jan 2024 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free