Pelvic organ prolapse
Peer reviewed by Dr Doug McKechnie, MRCGPLast updated by Dr Toni Hazell, MRCGPLast updated 31 Jul 2025
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
The organs inside a woman's pelvis include the womb (uterus), the bladder and the back passage (rectum). Normally, these are supported and held in position by certain structures including ligaments and the muscles at the bottom of the pelvis (pelvic floor muscles).
Pelvic organ prolapse (also known as genitourinary prolapse) occurs when these normal support structures are weakened and are no longer effective. The result is that one (or more) of the organs inside the pelvis drops down (prolapses). The space available for the organ(s) to drop down into is the vagina. There can be different degrees of prolapse, depending on how much, or how far, the organ(s) might have dropped down into the vagina. Sometimes, the prolapse can be so much that it causes the walls of the vagina, or the uterus, or both, to protrude outside the opening of the vagina.
In this article:
Video picks for Other women's health problems
How common is pelvic organ prolapse?
It is difficult to estimate how many women are affected by pelvic organ prolapse because many women do not visit their doctor for help. It is thought that around half of all women who have had children have some degree of GU prolapse but that most do not seek medical advice. In some cases this will be because the woman is not aware of the prolapse and it is not causing any problems.
Types of pelvic organ prolapse
Back to contentsDifferent types of pelvic organ prolapse can occur, depending on which pelvic organ, or organs, might have dropped down into the vagina. Generally, pelvic organ prolapse can be divided into the following, depending on which part of the pelvis it affects. However, pelvic organ prolapse may affect more than one part of the pelvis at the same time.
Prolapse affecting the front part of the pelvis (anterior prolapse)
There can be prolapse of the urethra (the tube along which urine passes from the bladder to the outside) into the vagina. The medical term for this is a urethrocele.
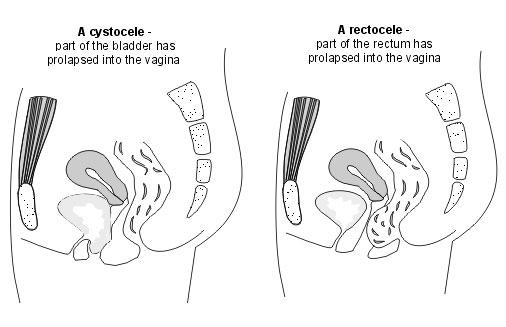
There can be prolapse of the bladder into the vagina. The medical term for this is a cystocele.
Or, both the urethra and the bladder can prolapse into the vagina at the same time. The medical term for this is a cystourethrocele. This is the most common type of pelvic organ prolapse.
Prolapse affecting the rear part of the pelvis (posterior prolapse)
There can be prolapse of the back passage (rectum) into the vagina. The medical term for this is a rectocele. This is the third most common type of pelvic organ prolapse.
Cystocele and rectocele
Prolapse affecting the middle part of the pelvis
Uterine prolapse

There can be prolapse of the womb (uterus) into the vagina. This is called a uterine prolapse. It is the second most common type of pelvic organ prolapse.
If a woman has had her womb removed (a hysterectomy), the end of the vagina that would normally attach to the neck of the womb (cervix) is closed up during the operation. This now blind end of the vagina is referred to as the vaginal vault. The vaginal vault can prolapse into the vagina. This is known as a vault prolapse.
There can be prolapse of the space between the rectum and the womb, known as the pouch of Douglas, into the vagina. The medical term for this is an enterocele. Loops of bowel may be present in the prolapse.
Continue reading below
Pelvic organ prolapse symptoms
Back to contentsYou can have a pelvic organ prolapse and not have any symptoms from it. It may just be noticed by a doctor when you are examined for another reason - for example, when you have a cervical smear test.
However, it is common for women to have some symptoms. There are certain symptoms that women with all types of prolapse can have. Symptoms include:
Feeling of a lump in your vagina or having a feeling of something 'dragging' or 'coming down'. You may actually be able to feel a lump or protrusion.
You may experience pain in your vagina, back or tummy (abdomen).
Sometimes, you may also notice a discharge from your vagina, which may be blood-stained or smelly.
Sex may be uncomfortable or painful.
Symptoms are usually worse after long periods of standing and they improve after lying down.
Other symptoms that you may experience can depend on the type of prolapse that you have. They can include the following:
Urinary symptoms
You may have urinary symptoms if your prolapse affects the front (anterior) part of your pelvis (your urethra and bladder). Symptoms may include:
The need to pass urine often, both during the day and at night.
Leaking of urine on coughing, sneezing, laughing, straining or lifting.
Feeling a sudden urge to pass urine, and also sometimes leaking urine before getting to the toilet.
A flow of urine that stops and starts.
A feeling that your bladder has not emptied properly and the need to pass urine again soon afterwards.
The need to change position whilst sitting on the toilet or the need to use your finger to push back the prolapse to enable urine to pass.
Also, complications may occur. These include:
Urine infections.
Not being able to pass urine at all (retention of urine), which may need treatment by inserting a small, flexible tube (a catheter) into your bladder to drain the urine.
Bowel symptoms
You may have bowel symptoms if your prolapse affects the rear (posterior) part of your pelvis (your rectum). Symptoms may include:
Difficulty passing stools (faeces) and having to strain to pass stools.
Feeling a sudden urge to pass stools.
A feeling that your bowels have not emptied fully.
Incontinence of stools.
Passing lots of wind.
A feeling of a blockage or an obstruction whilst you are passing stools.
The need to push on, or around, your vagina or perineum to enable stools to pass.
Sexual difficulties
Most women can have sex without problems with a prolapse but in some it may cause problems. It may be difficult to have sex, or it may be uncomfortable. The prolapse can affect arousal. For some women the prolapse is embarrassing so they may avoid having sex. There is no need to feel embarrassed about this and it is important to consult your doctor if a prolapse is causing you problems.
Other symptoms
If the prolapse is large enough to protrude from your vagina, this can lead to ulceration of the neck of your womb (your cervix) or skin. It may sometimes cause bleeding and infection.
Note: you may have a combination of these symptoms if prolapse affects the organs in different parts of your pelvis at the same time.
Causes of pelvic organ prolapse
Back to contentsIt is not known for sure why pelvic organ prolapse happens to some women but not to others. It is thought that a number of things may increase the risk of developing pelvic organ prolapse. They include the following:
Childbirth
Pregnancy and childbirth are the commonest factors which cause prolapse, but it does not affect everyone who gives birth. It may be more likely after a difficult, prolonged labour, a forceps or suction delivery, or if a woman gives birth to a large baby. It also becomes more likely the more times a woman has given birth. Prolapse is more common in women who have had vaginal births than those who have had caesarean sections.
Increasing age
The chance of having a prolapse increases as a woman becomes older. The lack of oestrogen hormone that occurs after the menopause affects the pelvic floor muscles and structures around the vagina, making them less springy and supportive.
Increased pressure inside the tummy (abdomen)
Anything that causes an increase in the pressure inside a woman's abdomen and pelvis can also be a risk factor for the development of pelvic organ prolapse. This can occur because of the strain put on the supporting ligaments and muscles. The most common reason for this increased pressure is during pregnancy and childbirth. However, the same increase in pressure can also occur in:
Women who are overweight.
Women who have persistent (chronic) lung problems, such as a chronic cough.
Women who frequently strain due to constipation.
Women who do heavy lifting as part of their job.
Gynaecological surgery
If a woman has had her womb (uterus) removed (a hysterectomy), or other gynaecological surgery, she may be more likely to develop pelvic organ prolapse. This is because the surgery may have weakened the ligaments, pelvic floor muscles and other support structures for the pelvic organs. However, with new advances in surgical techniques, including keyhole (laparoscopic) surgery, this is becoming less of a problem.
Other risk factors
Very rarely, pelvic organ prolapse can occur because of Ehlers-Danlos syndrome (EDS), a congenital problem (a problem that someone is born with) that causes deficiency, in the body, of a substance called collagen. Collagen is needed to help form the ligaments that normally support the pelvic organs. Also, it is thought that having a mother or a sister who has pelvic organ prolapse may increase a woman's risk.
Continue reading below
How is pelvic organ prolapse diagnosed?
Back to contentsPelvic organ prolapse is usually diagnosed by your doctor performing a simple examination of your vagina. They will usually ask you to lie on your left side with your knees bent slightly towards your chest. Your doctor may also ask to examine you whilst you are standing, or lying on your back, similar to when you have a smear test.
When they examine you, your doctor will usually insert an instrument called a speculum into your vagina. This may be a similar instrument to that used during cervical screening, or a differently shaped speculum. The doctor will usually move the speculum to the front and back walls of your vagina, allowing them to look for prolapse. Your doctor may ask you to cough or strain. These examinations are not usually painful. If you have bowel symptoms, your doctor may suggest that they examine your back passage (rectum).
Will I need any investigations for pelvic organ prolapse?
Back to contentsFor most women, examination alone is enough to make a diagnosis. If you have any urinary symptoms, as described above, your doctor may ask you to collect a specimen of urine to be sent off to the laboratory to check for signs of infection. They may also suggest that you have a blood test to check your kidney function. They may refer you to a specialist for some more detailed tests on your urine and bladder - for example, some tests known as urodynamic studies. These are tests of your urine flow and they are usually done in a hospital unit. If you have bowel symptoms, a specialist may suggest some special tests to look into these. Occasionally further tests, such as an ultrasound scan, are used.
Pelvic organ prolapse treatment
Back to contentsThe aims of treatment for pelvic organ prolapse are to ensure that you:
Are comfortable and pain-free.
Are able to pass urine and stools (faeces) adequately and have no problems with urinary or faecal loss of control (incontinence).
Are able to have sex comfortably.
Do not experience any complications relating to the prolapse, such as urine infections or ulceration of the prolapse.
Are able to continue to have children if you so desire.
As we will see below, some women will need surgery for their prolapse. However current guidance is that non-surgical methods should always be tried first.
Watchful waiting
If you have little in the way of symptoms, after discussion with your doctor, you may choose to wait to see how your symptoms develop. In some women, symptoms do not become any worse over time, and they may even improve. However, if you develop any new symptoms, you should see your doctor.
Lifestyle changes
During this period of watchful waiting, however, there are a number of things that you may be able to do to help prevent the pelvic organ prolapse from becoming any worse. As discussed above, there are a number of things that can cause a rise in the pressure inside your tummy (abdomen), increasing risk of pelvic organ prolapse, or making it worse. There is no evidence currently that making these changes helps; however, it makes sense to give them a try. For example:
If you have pelvic organ prolapse and are overweight, it may help if you lose weight. See the separate leaflet called Weight loss (Weight reduction) for more details.
If you are constipated you should discuss this with your doctor to ensure that you are receiving adequate treatment. See the separate leaflet called Constipation for more details.
Coughing can make prolapse worse. If you smoke, you should try to give up, and if you regularly cough and have not seen anyone about this, you should see your doctor to get it diagnosed and treated. See the separate leaflet called How to Quit smoking for more details.
You should try to avoid heavy lifting, as this may make prolapse worse.
Pelvic floor exercises
All women with pelvic organ prolapse, whether they have symptoms or not, should do pelvic floor exercises. The exercises may stop mild degrees of prolapse from becoming any worse. They may also relieve symptoms such as backache and abdominal discomfort. See the separate leaflet called Pelvic floor exercises. Your doctor may refer you to a physiotherapist with specialised skills in this type of exercise, as it is now recommended that these are done with supervision by an appropriately qualified healthcare professional, rather than on your own. However, access to this level of supervision on the NHS can vary by area and it is not always available. Pelvic floor exercises do not work overnight and you should use them consistently for at least four months.
A vaginal pessary
A vaginal pessary can be a very good way to manage pelvic organ prolapse. It may be used by:
Women who do not wish to have surgery.
Women who are still of child-bearing age.
Women who are waiting for surgery.
Women who have other illnesses that may make surgery more risky.
Pessaries can come in a variety of shapes but are usually in the shape of a ring. They are usually made of silicone or plastic.
Vaginal pessaries

© By Huckfinne, via Wikimedia Commons
Various vaginal pessaries, by Huckfinne, via Wikimedia Commons
Vaginal ring pessary

Vaginal ring pessary
Vaginal pessary placement

Positioning of a type of vaginal pessary
The ring is inserted into your vagina. It is left in place and helps to lift up the walls of your vagina and any prolapse of your womb (uterus). Vaginal pessaries are easily inserted; many doctors and some nurses are able to insert them. They should be changed every 6-12 months. If no GP in your practice is able to insert them then you can be referred to a specialist, or a GP with a particular interest in this area. This may be at a hospital-based clinic, or one in the community.
Having a vaginal ring pessary does not prevent you from having sex. It can either be left in during sex, or removed before sex and replaced afterwards. Discuss this with your doctor.
If you have pain or difficulty passing urine after you have a vaginal pessary inserted, you should speak to your doctor as soon as possible. You may need the pessary changing for a different size.
Vaginal pessaries do not usually cause any problems but (very rarely) they may affect the skin inside your vagina which can become ulcerated. Some women notice some discomfort during sex.
Vaginal oestrogen creams
If the prolapse is mild, your doctor may suggest that you apply some oestrogen cream to your vagina for 4-6 weeks. This may help any feelings of discomfort that you may have. However, sometimes symptoms may return once the cream is stopped. This cream is a type of hormonal replacement therapy (HRT), although it is not thought to have many of the risks which may be associated with HRT and in some cases it can be used by women who cannot use normal HRT, for example those who have had breast cancer.
Surgery for pelvic organ prolapse
The aim of surgery is to provide a permanent treatment for pelvic organ prolapse. There are various operations that can be performed, depending on the type of prolapse that you have. Keyhole surgery may be possible for some of these operations. Your surgeon will be able to advise which operation is best for you. Operations can include the following:
A vaginal repair operation: in this procedure, the walls of your vagina are reinforced, and tightened up. This is usually done by making a tuck in the wall of your vagina and using stitches to hold the tuck in place. The operation is usually done through your vagina and so you do not need a cut in your tummy (abdomen).
Removal of the uterus (a hysterectomy): this is a common treatment for uterine prolapse. In fact, pelvic organ prolapse is the most common reason why women over 50 years of age have a hysterectomy. Sometimes a hysterectomy is suggested at the same time as a vaginal repair operation.
An operation to lift up your uterus or vagina: there are various different types.
An operation to seal up the vagina (a colpocleisis). This is rarely done as it is not possible to have sex after this operation. However, it is a safe and effective operation for some women. Obviously the implications would be discussed before choosing to go ahead with this operation. It is a quicker operation than other types of surgery and is sometimes used in women who have a medical condition which means that a longer anaesthetic may be dangerous.
You may need to stay in hospital for a few days after your operation. Full recovery may take up to 6-8 weeks and your surgeon should give you a fit note if needed, to cover the entire duration that you will need to be off work. They should not ask you to see your doctor for a fit note. You should avoid heavy lifting and sexual intercourse during this time. There is a chance that a prolapse can return after surgery.
Why has surgery for prolapse been in the news recently?
Back to contentsIn 2020, Baroness Cumberledge published a report which looked at three areas where there was concern that patients might have been harmed. One of these was the use of pelvic mesh in surgery for prolapse. Pelvic mesh was used to support prolapsed organs, but led to significant complications in many women. These included pain, recurrent infections, incontinence and recurrence of their prolapse. In 2018, while the report was being written, a pause in the use of pelvic mesh was recommended and implemented. Current advice is that mesh procedures should only be carried out as part of research.
An update report was published in 2022, as a result of which NHS Resolution published a website for patients who may wish to bring a clinical negligence claim related to pelvic mesh. The link is in the further reading section of this leaflet. If you have ongoing symptoms related to the past us of pelvic mesh, your doctor should refer you to one of the specialist mesh services. There are currently nine of these, located in Cambridge, Manchester, Newcastle upon Tyne, Nottingham, Sheffield, Leicester, London, Southampton and Bristol.
All women who have surgery for pelvic organ prolapse should be recorded in a national registry which is being kept so that we can be alerted to complications earlier in the future than has happened in the past. Follow-up data must be recorded for at least five years.
As always, any surgeon who is proposing an operation should make sure that your consent is fully informed. This includes making you aware of the risks and benefits of the proposed surgery, and the likelihood of each, and giving you the right to make your own decision as to the type of surgery that will be carried out (whilst helping you with this decision if needed), as well as if you want to have surgery at all.
All patients having surgery for prolapse should be discussed with a multidisciplinary team which may involve a variety of professionals including surgeons, pain specialists and physiotherapists.
What is the outlook (prognosis) for pelvic organ prolapse?
Back to contentsLeft untreated, pelvic organ prolapse will usually gradually become worse. However, this is not always the case. Sometimes it can improve with no treatment. The outlook is best for younger women who are of a normal weight and are in good health. The outlook is worst for older women, those in poor physical health and those who have overweight or obesity. Pelvic organ prolapse can return after an operation. About 29 in 100 women need another operation at some point. For 13 in 100 women this occurs within five years of the original operation.
Can pelvic organ prolapse be prevented?
Back to contentsThere are a number of things that may possibly help to the risk of pelvic organ prolapse. However, not all of these have been proven. Simple things that you can do are:
Regular pelvic floor exercises, especially if you are planning to become pregnant, are pregnant, or have given birth.
If you have overweight or obesity, try to lose weight.
Eat a high-fibre diet (plenty of fruit and vegetables and wholegrain bread and cereal) and drink plenty of water to avoid constipation.
If you smoke, try to stop smoking.
Avoid occupations that involve heavy lifting.
Patient picks for Other women's health problems

Women's health
Pelvic pain in women
Pelvic pain is more common in women. There are many different causes of pain in your pelvic area. They can be separated by when they tend to happen, if you are pregnant and if they are accompanied by other symptoms such as vaginal bleeding. The most common causes are mentioned below. Most will improve with painkillers. Most recurring causes have treatments available.
by Dr Hayley Willacy, FRCGP

Women's health
Common problems of the cervix
There are many different conditions that can affect the neck of the womb (cervix), ranging from mild inflammation to cervical cancer. Some conditions affecting the cervix are more common than others; some are more serious than others. They can all cause different symptoms, such as abnormal bleeding or discharge from your vagina, or may not cause any symptoms at all. Some conditions are normal and do not need any treatment. The type of treatment, if needed, will depend on the underlying condition. Your doctor will be able to discuss the most appropriate treatment for you.
by Dr Toni Hazell, MRCGP
Further reading and references
- Hagen S, Stark D, Glazener C, et al; Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet. 2013 Nov 27. pii: S0140-6736(13)61977-7. doi: 10.1016/S0140-6736(13)61977-7.
- Ismail SI, Bain C, Hagen S; Oestrogens for treatment or prevention of pelvic organ prolapse in postmenopausal women. Cochrane Database Syst Rev. 2010 Sep 8;(9):CD007063. doi: 10.1002/14651858.CD007063.pub2.
- Post-Hysterectomy Vaginal Vault Prolapse; Royal College of Obstetricians and Gynaecologists (July 2015)
- Urinary incontinence and pelvic organ prolapse in women: management; NICE guideline (April 2019 - updated June 2019)
- Pelvic floor dysfunction: prevention and non-surgical management; NICE guideline (December 2021)
- Bugge C, Adams EJ, Gopinath D, et al; Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev. 2020 Nov 18;11:CD004010. doi: 10.1002/14651858.CD004010.pub4.
- First do no harm - the report of the independent medicines and medical devices safety review; 2020
- Vaginal mesh; NHS Resolution
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 29 Jul 2028
31 Jul 2025 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.