Coronary angioplasty
Peer reviewed by Dr Toni Hazell, MRCGPLast updated by Dr Doug McKechnie, MRCGPLast updated 9 Nov 2023
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
- Audio Version
Coronary angioplasty is a treatment to widen narrowed sections of the heart (coronary) arteries. It is also known as percutaneous coronary intervention (PCI). It involves the use of a thin, flexible tube (called a catheter) which is inserted into coronary arteries, via an artery in the wrist or groin and eventually the large blood vessels. It was developed as an alternative to major heart surgery, and is now the first-choice treatment for most people with heart attacks.
The small balloon at the tip of the catheter is blown up at the narrowed section of artery to open it up. A small mesh tube (called a stent) is usually left in place to keep the artery widened.
In this article:
Video picks for Other treatments
Continue reading below
What is a coronary angioplasty used for?
Coronary angioplasty is used:
In an emergency, to treat people who are having a heart attack (myocardial infarction), or have recently had one. Coronary angioplasty is used to open up blocked arteries that have caused the heart attack, allowing blood to flow to the affected area of the heart and reducing heart damage. Coronary angioplasty (and stent placement) can be life-saving for people with a heart attack.
As a planned ('elective') procedure, for people with angina. Coronary angioplasty can be used to open up narrowed arteries. It can help symptoms of angina. Now, it's usually only offered if medicines haven't been successful at controlling anginal symptoms.
How is a coronary angioplasty performed?
Back to contentsYou lie on a couch in a catheterisation room. An X-ray machine is mounted above the couch. Your heart rate, blood pressure, oxygen levels and heart rhythm will be monitored during the entire procedure. A thin, flexible 'guide' tube (catheter) is inserted through a wide needle or small cut in the skin into a blood vessel in the groin or wrist.
Local anaesthetic is injected into the skin above the blood vessel. So, it should not hurt when the catheter is passed into the blood vessel. The doctor gently pushes the catheter up the blood vessel towards the heart.
Low-dose X-rays are used to monitor the progress of the catheter tip which is gently manipulated into the correct position. You may be able to see the progress of the catheter on the X-ray monitor.
Once the catheter has reached the coronary arteries, dye is injected through the catheter. This dye shows up on the X-ray images, filling the coronary arteries and showing any narrowing or blockages. This part of the procedure is called an 'angiogram'.
Once the narrowing is identified, the tip of the catheter is pushed down through the coronary artery down to where there is a narrowed section caused by the fatty patches, or 'plaques', (atheroma). A second thinner 'balloon catheter' is then passed down the 'guide' catheter.
There is a balloon and a small tube (a stent) at the tip of the balloon catheter. The balloon is inflated for 30-60 seconds. This squashes the atheroma and widens the narrowed artery. When the balloon is blown up it stops the blood flow. Therefore, you may have an angina-like chest pain for a short time. However, this soon goes after the balloon is deflated.
Usually, a stent is left in the widened section. The stent is like a wire mesh tube which gives support to the artery and helps to keep the artery widened. The 'collapsed' stent covers the balloon and is opened as the balloon is blown up.
Some stents are coated with a chemical that helps to prevent the artery from becoming blocked again. People who are known to have an allergy to nickel may need a nickel-free stent.
The procedure may be repeated for one or more other narrowed sections within the coronary arteries.
Sometimes, if the narrowing (plaque) is very hard, or too tight for the balloon to get through, a procedure called 'rotablation' may be needed. Rotablation involves passing a catheter (tube) with a tiny drill on its tip over the guide wire, which gradually chips away at the plaque to open it up. This isn't painful, but can cause some mild chest discomfort.
You cannot feel the catheter inside the blood vessels. You may feel an occasional missed or extra heartbeat during the procedure. This is normal and of little concern. During the procedure your heartbeat is monitored by electrodes placed on your chest which provide a tracing on an electrocardiograph (ECG) machine. Sometimes a sedative is given before the test if you are anxious.
Coronary angioplasty
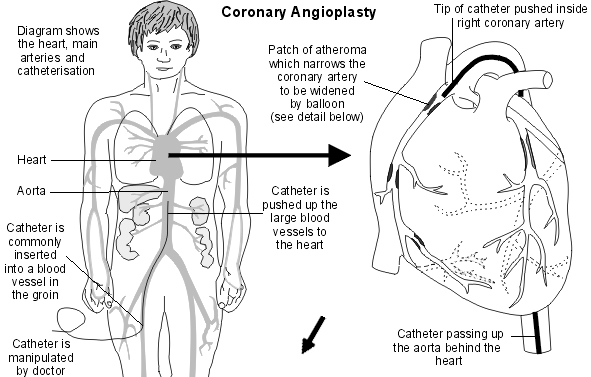
This image shows the path through the blood vessels that the angioplasty catheter uses to get to the coronary arteries.
Angioplasty and stent
This image shows how an angioplasty and stent placement is performed.
Continue reading below
How safe is a coronary angioplasty?
Back to contentsA coronary angioplasty is a commonly-used procedure, and is a safer alternative to heart surgery for treating blockages in the coronary arteries.
Coronary angioplasties do, though, have risks. How likely these risks are to happen differs from person to person, and is linked to things such as their age and any other medical conditions that they have. In general, though, serious complications are relatively uncommon, happening in fewer than 1 in 100 angioplasties.
See "Complications of a coronary angioplasty" below.
How to prepare for a coronary angioplasty
Back to contentsYou should receive instructions from your local hospital about what you need to do. The sort of instructions may include:
If you take 'blood-thinning' medicines such as warfarin or another anticoagulant, you may need to stop this for 2-3 days before the test (to prevent excessive bleeding from the site of the thin, flexible tube (catheter) insertion). Always tell your hospital team if you are taking a blood-thinning medicine, and take their advice about when to stop and restart them.
If you take insulin or medicines for diabetes, you may need to alter the timing of when you take these. Some medicines may need to be stopped for 48 hours. Your doctor should clarify this with you.
You may be asked to stop eating and drinking for a few hours before the procedure.
You may be asked to shave both groins before the procedure.
You will have to sign a consent form at some point before the test to confirm that you understand the procedure, understand the possible complications (see below) and agree to the procedure being done.
Continue reading below
How long does a coronary angioplasty take?
Back to contentsIf just one section of artery is widened, the procedure usually takes about 30 minutes. If several sections are to be widened then the procedure takes longer. You may need to stay in hospital overnight for observation following the procedure.
Recovering from a coronary angioplasty
Back to contentsAfter a coronary angioplasty, you should avoid heavy activities, such as lifting, for a week or until the small wound where the catheter was inserted is healed.
Driving
You shouldn't drive a car or a motorcycle for one week after having an angioplasty.
If you've had a heart attack, and had an unsuccessful angioplasty, you shouldn't drive for four weeks.
If you have a bus, coach, or lorry licence, you must inform the DVLA. You shouldn't drive for at least 6 weeks after the angioplasty, and will need a medical assessment before you can start driving again. The DVLA may ask for further tests to check that you meet the medical standard for driving.
Work
How long it takes to return to work depends on your job, especially how physically strenuous it is.
In general:
After an elective (planned) angioplasty, most people can return to work after a week.
After an emergency angioplasty (to treat a heart attack), it may take several weeks or months before you are well enough to return to work.
Speak to your doctor for advice on your individual situation.
Sex
Avoid having sex until the puncture site (in the wrist or groin) has healed - at least several days.
After that, you can start having sex again when you feel ready to do so. Sex is equivalent to mild-to-moderate physical exercise (for example, climbing two flights of stairs). So, when you are able to do that without feeling short of breath, having chest pain, or feeling very tired, you should be able to have sex again.
After having an elective angioplasty, you might feel ready to have sex again after a few days.
After an angioplasty for a heart attack, it might take longer before you're ready - usually at least two to four weeks.
Complications of a coronary angioplasty
Back to contentsCoronary angioplasties are generally safe procedures, but there are risks. Serious complications are relatively uncommon, usually occurring in fewer than 1 in 100 people. How likely they are differ from person to person and on the situation; for example, complications may be more likely if the angioplasty is treating a complicated artery blockage.
Risks and complications of a coronary angioplasty during, or shortly after, the procedure include:
Bruising around the puncture site (wrist or groin). This is common and usually settles after a few days.
A large pooling of blood under the skin near to the puncture site, caused by damage to the artery wall (pseudoaneurysm). This is uncommon.
Failure of the procedure. Sometimes, it's not possible to stretch the blocked or narrowed arteries. This might mean that a coronary artery bypass graft - a type of open heart surgery - is required instead.
Infection at the puncture site (wrist or groin).
An allergic reaction to the contrast dye.
Kidney damage due to the contrast dye (uncommon, and usually reversible, but more of a risk in people who already have kidney problems).
Serious damage to a coronary artery, requiring emergency heart surgery to fix. This is rare.
A heart attack caused by the procedure. This is uncommon.
A stroke caused by the procedure. This is uncommon.
Rarely, serious complications of the procedure can cause death.
Longer-term risks of coronary angioplasty include:
The treated coronary artery narrowing again (restenosis) over time. This is less likely with newer stents and medicines. If it does occur, it may be treatable with another angioplasty.
A blood clot forming in the stent, causing a blockage of the artery and a heart attack. This is rare, but can be very serious. Medicines such as aspirin and clopidogrel, prasugrel, or ticagrelor are prescribed after an angioplasty to prevent blood clots from forming in the stent. It's very important to take these as prescribed.
How successful is a coronary angioplasty?
Back to contentsCoronary angioplasty and stent placement is a very effective treatment for heart attacks. It has mostly replaced treatment with clot-busting drugs, as it's more effective. It's successful in opening the blocked coronary artery in around 9 out of 10 cases, and can be life-saving. For large heart attacks, coronary angioplasty is best done as soon as possible to reduce damage to the heart muscle.
For people with stable angina, coronary angioplasty can improve symptoms of angina. It improves symptoms of angina quicker than medicines alone. However, in stable angina, coronary angioplasty doesn't prevent future heart attacks, and doesn't make you live any longer. By contrast, medicines for angina do reduce the risk of having a heart attack, and can also control angina symptoms. So, cardiologists often advise treating angina with medications, and keeping the option of an angioplasty in reserve in case symptoms aren't well-controlled enough by medicines.
Sometimes, the narrowing of the coronary arteries can be too complex to treat with angioplasty; for example, the narrowing might be too long, too tight, or there might be too many. If this is the case, coronary artery bypass surgery may be required. However, angioplasty techniques are becoming more and more sophisticated over time, and have become better at treating complex narrowings.
Patient picks for Other treatments

Treatment and medication
Osteopaths and chiropractors
Both chiropractors and osteopaths provide treatments for bone, joint and soft tissue problems.
by Dr Philippa Vincent, MRCGP

Treatment and medication
Haemodialysis
The kidneys have a very important function in the body. Healthy kidneys balance fluid and chemicals in the body, and remove harmful waste products. The kidneys also make hormones that help to control blood pressure, make red blood cells, and keep bones strong and healthy. Dialysis can be used to remove waste products and excess fluid from the blood when the kidneys are unable to do this properly, such as in acute kidney injury or chronic kidney disease. There are 2 main types of dialysis, haemodialysis and peritoneal dialysis. Peritoneal dialysis involves pumping dialysis fluid into the space inside the tummy (abdomen) to draw out waste products from the blood passing through blood vessels lining the inside of the abdomen.
by Dr Colin Tidy, MRCGP
Further reading and references
- Drug-eluting stents for the treatment of coronary artery disease; NICE Technology Appraisal Guidance, July 2008
- Percutaneous laser coronary angioplasty; NICE Interventional Procedure Guidance, January 2011
- Assessing fitness to drive: guide for medical professionals; Driver and Vehicle Licensing Agency
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al; 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165. doi: 10.1093/eurheartj/ehy394.
Continue reading below
Article history
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 7 Nov 2028
9 Nov 2023 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.