
Coronavirus: how quickly do COVID-19 symptoms develop and how long do they last?
Peer reviewed by Dr Colin Tidy, MRCGPLast updated by Dr Sarah Jarvis MBE, FRCGPLast updated 8 Jan 2021
Meets Patient’s editorial guidelines
- DownloadDownload
- Share
- Language
- Discussion
By now, hopefully everyone knows about the key COVID symptoms - fever about 37.8°C, new, continuous cough and loss of (or new change to) your sense of smell and/or taste. But there's still much confusion about how quickly COVID symptoms develop after exposure to the virus and what you can expect if you do become infected.
In this article:
Video picks for Long COVID
Let's start with a disclaimer - it may feel as if COVID-19 has been around for ever, but this is still a relatively new disease and evidence is changing at speed. And as countries around the world see more cases and manage the pandemic in their own ways, lessons are being learnt.
In the first weeks after a country is affected or a new wave of cases occurs, there is usually adequate hospital and Intensive Care Unit (ICU) capacity. But as health services are overwhelmed, patients who would previously have been admitted to hospital for observation are cared for at home; patients who might previously have been ventilated in ICU are kept on hospital wards, with less invasive methods of breathing support such as continuous positive airways pressure (CPAP) to keep them going; and ventilation on ICU is reserved for the sickest of the sick.
In fact, since the first wave of the pandemic, it has become clear that outcomes for most patients are better if mechanical ventilation can be avoided. A move by hospitals to nurse patients 'prone' (lying on their fronts) as much as possible, and to delay mechanical ventilation where feasible, has been at least in part credited with the improved survival rates seen since the first wave.
To make matters more confusing still, definitions of mild, moderate and severe infection also vary between countries.
All these variables make it impossible to offer completely accurate predictions of average time to hospital admission, or average time before ICU recovery. The figures in this article are based largely on a report by the World Health Organization of the Chinese experience. Some reflect the experience of other European countries.
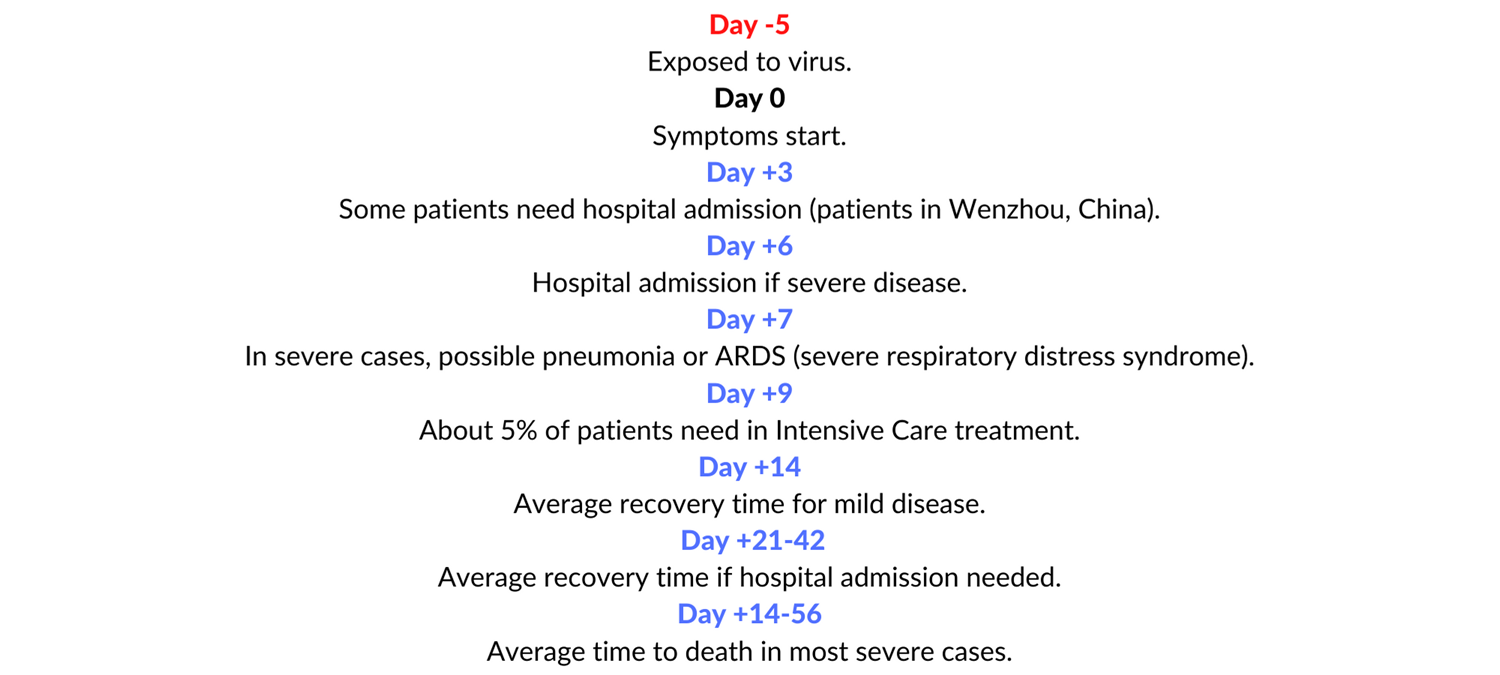
The timeline below gives approximate/average dates. They are designed for guidance - please do not rely on them. They are not a substitute for seeking help about your individual symptoms.
COVID-19 Timeline
Continue reading below
Incubation - how long before COVID symptoms start?
The incubation period of an infection is the time between being exposed to it and developing COVID symptoms. There are several challenges with working out the incubation period for coronavirus:
It is not always possible to know when people were first infected, especially if they may have received several 'doses' of virus.
There seems to be significant variation in the length of time it takes people to develop symptoms.
Some countries only test (and confirm) coronavirus in people with severe infection, and it's not known if the incubation period for people with critical/severe/moderate/mild infection is different.
It's thought that many people do not develop symptoms (they are 'asymptomatic') so there are no symptoms to count back from.
However, one study has looked at confirmed cases from 50 provinces, regions and countries outside Wuhan, where it was possible to identify a single source of infection. They found that:
The median incubation period (half of all cases occur before this time and half after) was 5.1 days.
97.5% of people who develop symptoms will have got them within 11.5 days.
Stages of COVID symptoms
Back to contentsA World Health Organization report based on 56,000 confirmed cases revealed the most common symptoms to be:
Fever (88%).
Dry cough (68%).
Tiredness (38%).
Coughing up sputum (33%).
Shortness of breath (19%).
Aching muscles or joints (15%).
Sore throat (14%).
Headache (14%).
Blocked nose (5%).
Coughing up blood (1%).
Pink/redness of the whites of the eyes (1%).
Up to 1 in 10 people present with diarrhoea and feeling sick 1-2 days before they develop other symptoms.
Editor’s note
Dr Sarah Jarvis, February 2021
New data from the Office for National Statistics look at the frequency of COVID symptoms reported by people in the UK since late 2020. They show that with the 'new' Kent variant, which is now the most common strain in the UK, some COVID symptoms are slightly more common and some slightly less common than with the original variant. These include:
More common:
Sore throat (22% with the new variant vs 18% with the original strain).
Cough (33% with the new vs 28%).
Weakness and fatigue (32% vs 28%).
Muscle aches (25% vs 22%).
Less common:
Loss of/change to sense of smell and taste(15% vs 18%).
Similar frequency with both strains:
Feeling sick or being sick (10%).
Shortness of breath (13%).
Diarrhoea (7%).
Abdominal pain (7%).
There does not appear to be any particular pattern in the stages of COVID symptoms. Some people will start with a cough; others will develop fever, with cough arriving only a few days later. Among my patients, exhaustion and aching all over appear to be common early signs.
Continue reading below
How and when do COVID symptoms progress?
Back to contentsIf you have mild disease, fever is likely to settle within a few days and you are likely to feel significantly better after a week - the minimum time at which you can leave self-isolation is ten days.
You may continue coughing for a couple of weeks - while you should be very careful to maintain social distancing, as everyone should, you don't need to stay in isolation just because your cough has not completely resolved. If you're well in other respects, your likelihood of infecting others at this stage is low.
Loss of sense of smell can also persist - in many patients this has continued for several months. However, persistence of a loss of or change to your sense of smell or taste is not a reason to continue to self-isolate if your other COVID symptoms have settled. If you still have a fever after ten days, you must stay in self-isolation.
In people with more severe infection, shortness of breath is likely to become more marked 7-10 days after they develop symptoms. This occurs because the infection takes hold deep in your lungs, leading to inflammation which prevents efficient transfer of oxygen from your lungs to your bloodstream. COVID symptoms can develop rapidly (in hours) and worsen in minutes.
Even if you have completed the form before and been advised you do not need medical help, you need to call 999 if:
You are too breathless to speak more than a few words; or
Your breathing has become harder and faster in the last hour, even when you are not doing anything.
You need to call 111 and speak with a nurse if:
You are feeling so ill that you have stopped doing everything you normally do (eg watching TV, using your phone, getting out of bed); or
You have suddenly become confused (this can be a symptom of lack of oxygen to the brain).
The final outcome - how likely am I to die?
Back to contentsIt's important to remember that even if you are ill enough to need hospital admission, most people are much more likely to recover than to die.
At the start of the pandemic, the UK was very poor at providing COVID-19 testing - in fact, people were only tested for COVID-19 if they were ill enough to require hospital admission. Therefore, the 'case fatality rate' - the proportion of people diagnosed with COVID-19 who died as a result of their infection - was very high.
Thus in April 2020, a UK study suggested that among people diagnosed with COVID-19, 0.66% (1 in 150 people) died. Even at this stage, the influence of increasing age was clear - among this group of patients, death rates ranged from 0.0016% among under-9s to 7.8% (1 in 12) among over-80s.
In fact, fewer than 10 children under 14 have died from COVID-19 in the UK during the entire pandemic, and the average age at death is over 80, with more than 90% of deaths among the over 65s.
While the NHS Test and Trace system has been beset by problems, it does by now have capacity to test the vast majority of people who develop symptoms. By the beginning of August 2020 the REACT study - a nationwide surveillance study - found antibody evidence suggesting 6% of people in England (about 3.3 million) had been infected since the pandemic began. At this stage, about 47,000 people (1 in 1,170 of the population) had died from it.
A 'model-based analysis' of the widely varying statistics on death rates for coronavirus, based on figures from 37 countries, suggests that even among people with more severe disease, the 'case fatality' ratio (the proportion of people with confirmed disease who died) is about 1.4% - about 1 in 300 among people under 60, 1 in 15 among all over-60s and 1 in 7 among over-80s.
Another paper backs up the idea that your risk of dying, even if you end up in hospital, depends largely on your age. While a significant number of people needing ICU treatment will not recover, recovery rates for people who do not need ventilation are good.
Continue reading below
How worried should I be?
Back to contentsThe great majority of people with coronavirus will have mild or moderate disease and will make a full recovery within 2-4 weeks. But even if you are young and healthy - meaning your risk of severe disease is low - it is not non-existent. And a significant proportion of people who do recover are left with debilitating long-term symptoms - so-called 'long covid'.
We ALL need to play our part in reducing the spread of coronavirus by following government rules.
If you develop COVID symptoms:
Check for red flags on the NHS 111 online checker.
Isolate yourself from the outside world and anyone you live with, for at least ten days.
If you have symptoms, you can book a free test online.
Ensure everyone you live with isolates for ten days from the onset of your symptoms or positive test result or ten days from when they develop symptoms, whichever is the longer.
Look after yourself with plenty of rest, fluids and painkillers if needed.
Look out for the worsening symptoms above.
Seek medical help as needed.
Patient picks for Long COVID

COVID-19
Long COVID: What are the symptoms and treatment?
The term 'long COVID' may have only been coined last year, but with 1.1 million people in the UK now thought to be living with the illness, there is an urgent need for new expert advice.
by Amberley Davis

COVID-19
Long COVID: what support is available?
As the COVID-19 pandemic continues, we are learning more about the illness and the impact it has. One thing we now know is that for some people it has a more long-term effect, dubbed long COVID.
by Andrea Downey
Continue reading below
Article history
The information on this page is peer reviewed by qualified clinicians.
8 Jan 2021 | Latest version

Ask, share, connect.
Browse discussions, ask questions, and share experiences across hundreds of health topics.

Feeling unwell?
Assess your symptoms online for free
Sign up to the Patient newsletter
Your weekly dose of clear, trustworthy health advice - written to help you feel informed, confident and in control.
By subscribing you accept our Privacy Policy. You can unsubscribe at any time. We never sell your data.